Skin melanomas are malignant neoplasms originating from neuroectodermal melanocytic cells [1]. In Poland, melanomas are relatively rare – the standardized incidence rate is about 4.9/100,000. The most important factors of the increased risk of developing the disease are intense exposure to natural and artificial ultraviolet radiation, constant mechanical or chemical irritation, low pigment content in the skin and genetic predisposition. The recommended test used in the initial diagnosis is dermatoscopy or videodermoscopy. The basis for the diagnosis of skin melanomas is the histopathological examination of the entire excised pigmented lesion.
Brain metastases are the most frequently diagnosed intracranial tumours in adults; they are diagnosed about 10 times more often than primary tumours [2]. More than 80% of metastatic brain tumours are found after the diagnosis of the primary tumour [3]. The clinical symptoms of metastasis depend on the presence and growth of the tumour itself, accompanying cerebral white matter oedema and/or the development of hydrocephalus [4, 5]. The diagnosis is made on the basis of nuclear magnetic resonance (NMR) or computed tomography (CT) imaging tests.
Chronic subdural hematomas (CSDH) are most common among the elderly [6]. The predisposition of their occurrence among older patients is associated with the process of cerebral atrophy and reduction of its volume in the cranial cavity, and the weakening of the walls of superficial veins of the brain. Chronic subdural hematomas are most often manifested by headaches, progressive cognitive decline, personality changes, psychomotor retardation, paresis or aphasia. The decisive examination is CT of the head, which, with approx. 99.9% sensitivity, visualizes CSDH.
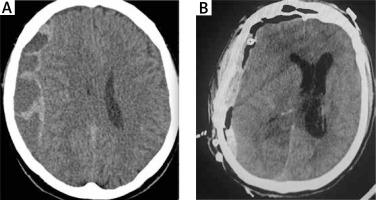
In 2015, a 63-year-old patient was admitted to the Department of Neurosurgery, Neurotraumatology and Paediatric Neurosurgery, Collegium Medicum Nicolaus Copernicus University in Bydgoszcz due to symptoms of progressive weakening of the muscles of the left limbs. The CT scan of the head revealed the presence of an extensive chronic right-sided cerebral hematoma. The patient denied the head injury. According to the data from the history, he was treated oncologically for dorsal melanoma about 10 years earlier. On admission, the patient was conscious, in logical verbal contact, slightly psychomotor slowed down, with a slight left-sided paresis. The patient underwent surgical treatment via craniotomy: the hematoma was removed along with the membranes within the bone opening, including the thick internal membrane of the hematoma, which prevented the expansion of the brain. At the same time, within the dura mater, numerous metastasis changes of about 5–10 mm in size were observed – the visible range of the dura mater was removed and sent for histopathological examination. The control CT of the head showed a reduction in the weight of the hematoma. Improvement in the patient’s neurological condition was observed within a few days after the procedure (Figure 1). Subsequent imaging examinations and outpatient control revealed no recurrent subdural hematoma. After receiving the results of the histopathological examination, the patient was transferred for further oncological treatment.
Melanoma is responsible for 7–13% of brain metastases and is the third leading cause of their formation, after lung cancer and breast cancer [7, 8]. The incidence of brain metastases in patients with regionally advanced melanoma is about 10%, while in patients with generalized disease it is 15–46% [9, 10]. In nearly half of patients with central nervous system (CNS) metastases of melanoma they are the cause of death, while autopsy examination shows the presence of melanoma in 50–75% of such cases [11]. The prognosis of patients with CNS metastases in the course of melanoma is poor, moderate survival is 3–6 months; in patients receiving only corticosteroid therapy, the average survival is 2 months, while after whole brain radiotherapy (WBRT) it is 3 to 4 months [12, 13]. Numerous data from the literature indicate that some patients may benefit from surgery or radiosurgery, where survival ranging from several to over 12 months is observed; this applies to patients with single metastatic foci [12]. In the latter, anti-CTLA-4 antibodies directed against the cytotoxic antigen-4 of T lymphocytes (ipilimumab) or the BRAF receptor serine-threonine kinase inhibitors (vemurafenib, dabrafenib) are used [10, 13].
We present the discussed case for two reasons: the above-mentioned casuistic rarity of the simultaneous occurrence of chronic subdural hematoma and numerous metastases to the CNS in the course of melanoma in the period of about 10 years after the treatment of the primary lesion. The clinical symptoms first suggested only a chronic subdural hematoma. However, intraoperatively, multiple metastases within the dura mater were visualized. The histopathological preparation of the surgical material was assessed by two independent pathologists who also analysed the patient’s clinical data before making the final diagnosis. Metastases within the dura mater in the course of melanoma can be differentiated from meningeal carcinoma, diffuse meningeal oligodendrogliomatosis [14], infectious diseases, amyloidosis, and idiopathic hypertrophic dura mater. Initially, primary meningeal melanoma (no infiltration characteristic of this form) and primary neoplasms diffusely occupying the meninges, such as sarcoma, glioblastoma or meningeal lymphomas were excluded. The microscopic image and the location of the lesion were decisive for the diagnosis. Unfortunately, despite the oncological treatment, the patient died within 4 months after the end of neurosurgical hospitalization.