Introduction
Infertility is a condition affecting about 15% of all couples and assisted reproductive technology (ART) represents the most important scientific progress in the quest to cope with this condition and to reach the desired parenthood. Different techniques are used, which include in vitro fertilization (IVF), intra cellular sperm injection (ICSI), crioconservation of oocytes and embryos, embryo transfers, and every shrewdness to favour the embryo-endometrial lining contract [1–5]. Nevertheless, even if a pregnancy is made possible by ART, it is very hard to go beyond the feelings of grief and loss linked with infertility, especially when considering the difficult hormonal treatment women undergo [6]. Gynaecological conditions such as endometriosis could be responsible for the development of anxiety and depression in such women [7], but the exhaustive ART pathway can bring more significant psychological distress to both men and women, especially in cases of repeated failures [8]. The medical conditions hindering a spontaneous pregnancy can act as specific psychological risk factors for the development paths of the individual and the couple. These complications include anxiety and depressive disorders, compulsive behaviour to manage anxious states, and inclinations to self-blame [9, 10]. Moreover, the sexual wellbeing of the women is hampered [11].
Most of the studies focus on psychological variables, such as depression and anxiety, disorders that contribute to causing a specific global infertility-stress condition and can influence the maternal/paternal-infant attachment [8, 12].
Concerning the anxiety levels, many aspects have been considered. Some studies focus on how depression and anxiety levels change during pregnancy according to the number of ART attempts (first attempt vs. consecutive ART treatments) [9]. Other studies investigate the role of gestational age in decreasing anxiety levels: in particular, these assume that anxiety could be lower after the third month of pregnancy, thanks to the early use of medical checks that can confirm the health of the foetus and the absence of genetic syndromes [13]. Moreover, studies in ART investigate if the psychological maladjustment of couples during fertility treatments, such as anxiety levels, depression, and feelings of helplessness, influence the patients’ intentions to comply with treatment [14].
The relationship between anxiety levels experienced during pregnancy and the low quality of maternal and infant prenatal and postnatal attachment has been investigated because anxiety about the survival of the foetus could adversely affect early parenting competence [15].
These studies on anxiety reveal that helplessness and the feeling of lack of control over one’s own life could determine a dysfunctional use of coping strategies [16].
In addition to these specific psychological variables, the impact of ART on the quality of life (QOL) and general health of pregnant women in the field of medically assisted reproduction has been investigated [17]. The increased rate of children born after insemination in many cultures has led to the examination of social and demographic characteristics, family backgrounds, reproductive histories, and attitudes towards motherhood in single and cohabiting women seeking treatment with donor semen [18].
Some studies also focus on many kinds of treatment and psychosocial interventions for risk condition management in medically assisted reproduction. These studies refer to the efficacy of the preparatory counselling or mind/body interventions [19].
An additional consideration regarding the quality of family interactions is made for couples undergoing ART; it is necessary to investigate the ability of these parents to accept their parental role, also due to a sense of parental self-efficacy and adequate self-esteem that can have a positive impact on the management of the desired child (Ibid.).
Finally, the risk condition of twin birth inherent in ART and the fact that excessive levels of parental distress can lead to dysfunctional outcomes in terms of family functioning and therefore in terms of child development deserve consideration [20].
All these considerations are fuel for the need for a systematic review that could group all the evidence in psychological wellbeing in ART.
Material and methods
This systematic review followed the PRISMA guidelines for methodology and data extraction. Furthermore, a protocol for this review was registered on PROSPERO in April 2020 (PROSPERO registration number CRD42020169243).
Aim
This systematic review aimed to investigate main psychological variables involved in the special risk conditions of medically assisted reproduction, and how they could direct specific guidelines to enhance mental wellbeing in the condition of infertility.
Study selection process
This systematic review included randomized, controlled, prospective studies of longitudinal design with repeated measures, cross-sectional studies, and baseline data collection in multicentre cohort studies (i.e. study design). The outcome measures considered were psychological variables (i.e. anxiety, depression, infertility related-stress, parental-foetal attachment, coping strategies, acceptance cognition, self-esteem, resilience) and social/relational variables (i.e. social support, QOL, general health, family relation quality, family backgrounds). Moreover, the intervention program evaluated during the medically assisted procreation path, suggesting support treatment (preparatory counselling, mind/body intervention, maladjustment early assessment) to promote parental competence, have also been considered eligible criteria for inclusion in this review.
Studies involving homosexual-parents with donor semen or surrogates’ mothers were excluded, as studies which were not published in English language and were published before 2011. In addition, systematic review and meta-analysis were excluded also.
The studies have been identified through database research on PubMed, PsychInfo, MEDLINE, and Google Scholar. In each database, the following key words were searched for: ART and parental competence, medically assisted reproduction and social support, ART and psychological variables. Their synonymous were identified (i.e. medically assisted reproduction in combination with “psychology”, “maternal behavior”, “maternal-fetal relation”).
Data extraction and quality of assessment
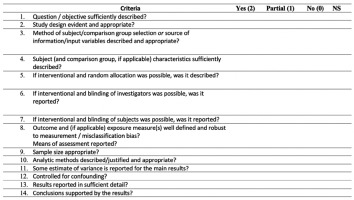
Specific information was extracted pertaining to the following: reference (title of papers), source (author and year), study population (age and sample size), aim of the study, intervention program, outcome measures, results and discussion (main issues), and quality assessment (Table 1). The quality of assessment was carried out using a checklist, as described by Kmet et al. [19] (Fig. 1), which evaluated, through a 14-item checklist, the following variables: methods description, outcome assessment, and conclusions. Each analysed study was given a score of 2 if the answer to the item’s checklist was yes, 1 if the answer was partial, and 0 if the answer was no or not specified.
Table 1
Characteristics of the articles included in the systematic review
[i] ART - assisted reproductive technology, EPDS – the Edinburgh Postnatal Depression Scale, IVF - in vitro fertilization, LMIB - ????, MAR - medically assisted reproduction, MFA - ???, MIBS-J - Mother-to-Infant Bonding Scale, NC - ???, PGD - preimplantation genetic diagnosis, QOL - quality of life, WHOQOL-BREF World Health Organization Quality of Life-BREF Questionnaire, SC – spontaneous conception, STAI – State-Trait Anxiety Inventory
Two researchers were involved in giving these scores, and any disagreements were resolved by scores given by a third researcher. The cut-off to consider each examined article as methodologically sufficient was set at 70%; hence, the articles assigned a score lower than 70% were considered with low methodological quality.
Results
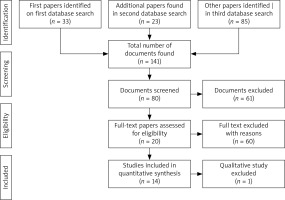
The first searches in databases showed a total of 141 papers; according to the PRISMA checklist [21] and inclusion criteria, a more accurate search was performed, selecting 14 papers for data extraction (Fig. 2).
The studies analysed in this systematic review showed a large variety in methodological approach. In detail, 2 of the examined studies used a randomized controlled trial design, 3 were cross-sectional, 4 had a longitudinal prospective, 2 were prospective cohort studies, 1 study was explorative, 1 was a case-control study, and another was an observational study.
Twelve papers had a methodological quality higher than 70%, and only 2 studies had a methodological quality lower than 70%.
The samples of participants varied widely, although most studies focused on women [14, 17, 22-26]; more than 2 of these studies considered women in relation to their children and in relation to their partners [14, 25]. Some samples were formed by couples [9, 13, 15, 16, 19], 1 study considered men, and 1 paper included family groups [20, 27].
The variables taken into consideration for the psychological impact assessment of medically assisted procreation reported considerations about anxiety levels, depression, infertility-related stress, prenatal attachment, parental role, coping strategies, QOL, family functioning, and clinical pregnancy rate. Here, the principal results of the studies are reported that obtained higher scores in the quality assessment path [28].
In a study by Udry-Jørgensen et al. [11], the analysis of variance (ANOVA) for men and women with ART and spontaneous conception (SC) compared anxiety levels, depression, and attachment scores from 12 weeks of gestational age (T1) and 14 weeks of pregnancy (T2); anxiety scores decreased in both women [F (1.85) = 11.15, p = 0.001], and men, [F (1.81) = 6.38, p = 0.013]. The same results for depression symptoms were highlighted for men [F (1.81) = 4.49, p = 0.037], whereas prenatal attachment was increased in both women [F (1.85) = 18.27, p < 0.001] and men [F (1.81) = 14.92, p < 0.001].
With regard to male depression symptoms, Pinto et al. [25] showed that the prevalence of men with high depressive symptomatology, assessed by the Edinburgh Postnatal Depression Scale (EPDS) (Cox 1987), was higher in the ART group than in the normal conception (NC) group (z = 3.20, p < 0.001). According to the results of multivariate analysis of covariance (MANCOVA) and univariate analysis of covariance (ANCOVA), significant multivariate effects of the interaction between type of conception and depressive symptomatology were found on paternal antenatal adjustment and paternal attitudes [Wilks’ lambda = 0.43, F (6.189) = 21.41, p < 0.001, η2 = 0.25]. Once again, significative univariate effects were found for the marital relationship, attitudes toward sex, and attitudes toward pregnancy and the baby during the second trimester of gestation (all p < 0.001).
The ordinal logistic regression analyses using emotional distress, social support, and primary infertility as predictors of expectations for preparatory counselling for women and men in the study by Hakim et al. [17] showed significative scores for woman and men in infertility-stress and expectation of counselling as “important” (0.023, p < 0.05), although they expected counselling to be “evaluative” (0.022, p < 0.05) before participating. In the same way, even men with high stress levels felt counselling to be “important” (0.020, p < 0.01) and “helpful” (0.020 p < 0.05).
The significant tests of the linear mixed model conducted by Kuo et al. [21] verified the values detect by the Social Support Apgar (0.45, p < 0.001), the Chinese Childbearing Attitude Questionnaire (0.46, p < 0.001), and the Awareness of Foetus Scale (1.29, p = 0.01) as statistically significant predictors of maternal-foetal attachment
The analysis of variance conducted by ANOVA test in a study by Salimi Akin Abadi et al. [24] showed significant differences in mean scores of maternal self-esteem between intervention and control groups (p < 0.001). The intervention group, composed of mothers undergoing IVF, participated in a maternal preparation psychoeducational program, whereas the control group only received the routine care provided by the hospital.
In particular, the intervention group scores were significant different immediately post-intervention (M = 42.4, SD = ±3.9) and 1-month post-intervention (M = 42.5, SD = ±4) (p < 0.001). The control group showed no significant differences (p < 0.31).
Discussion
The psychological wellbeing of infertile couples is a medical issue that is gaining popularity day by day. In this context both the partners are important, and more effort should be spent in reducing gender-specific differences [29].
The analysis of the results presented in the studies identified 9 main topics falling within psychological and social variables. The first ones included anxiety, depression, stress, and coping strategies; the last ones included maternal-infant attachment, parental role, QOL, and family functioning. Finally, the pregnancy rate was studied as a measure of intervention efficacy.
Anxiety
Anxiety levels, assessed by the state-trait anxiety inventory [30] in most of the studies, decreased as the time of gestation increased. In Taiwanese women, scores were significantly lower at 20 weeks than at 9 weeks [23]. These results are consistent with the literature, according to which pregnancy and the hormones involved make it possible to lower anxiety levels [31, 32]. Moreover, the first screening test of prenatal diagnosis could reduce anxiety in couples undergoing ART and SC [13]. More specifically, women in the ART group experienced a greater decrease after testing compared to women in the SC group, whose anxiety decreased only slightly.
The number of ART attempts was relevant for perceived anxiety; couples who were pursuing ART treatment for the first time showed higher levels of state anxiety compared to couples who had repeatedly undertaken ART [9]. However, some studies have shown that anxiety tends to increase especially after experiencing several failed attempts and longer treatments [33–35].
Results were discordant regarding the data on men, while in terms of state-trait anxiety, scores were significantly higher among men than among women in both single ART attempt couples and multiple ART attempt couples [9], and there were no associations between the mode of conception (ART vs. SC) and anxiety [27]. However, as the literature suggests, these data underline the importance of male psychological adaptation in clinical practice, which is too often left aside during infertility treatments [36].
In the assessment of anxiety levels as a predictor of couples’ expectations for the evaluation of preparatory counselling, half of the women demonstrated elevated symptoms of anxiety, but they were not significant predictors of positive or negative expectations about preparatory counselling [19]. Eleven women out of 72 (15%) displayed psychological disorders, and 6% of men reported clinically significant anxiety levels.
Anxiety was relevant when associated with lower intentions to comply with treatment [14]; indeed, men who presented with high levels of acceptance cognition, in terms of ability to accept one’s infertility, showed high anxiety levels, and they were associated with lower intention to comply with treatment.
Regardless of the type of conception paths, couples undergoing preimplantation genetic diagnosis (PGD), ICSI, or SC showed no differences between groups. Couples experienced an increase in anxiety levels in terms of “fear of birth” during gestation and showed a progressive decrease of “fear of an ill child” [15].
Measured 4 times during gestation, “fear of changes” in ICSI and SC couples increased from 12/14 weeks of pregnancy and 30/32 weeks of gestation. More specifically, some gender differences were found: men seemed to be more afraid about birth than women, and they showed anxiety about changes in their life after giving birth.
Depression
The psychological impact of medically assisted procreation is evaluated through anxiety levels associated with depressive symptoms. Despite the lack of significant associations between the number of ART attempts and depressive disorders in a cohort study by Sejbaek et al. [22], couples with consecutive ART treatments showed higher depressive symptomatology than couples at first ART attempt [9]; more specifically, women had higher depression levels than men in both first ART attempt and consecutive ART treatment groups.
There are many studies in the literature about depression levels because depression is a widespread condition and is often related to infertility; even after assisted reproductive technique treatments, couples sometimes fail to overcome the feelings of mourning and loss associated with infertility [37].
However, the results of a Danish cohort study from 1994 to 2009 showed that only 1.3% of women had a certified diagnosis of unipolar depression after experiencing at least one ART attempt [24]; despite these data, it is interesting to note that 64% of the women with live births and 35.7% of the women with no live births received a diagnosis of unipolar depression. This indicates that women with live births had an increased risk of certified depression compared with women with no live births. This is because it is probably more difficult to manage a postpartum depression condition, the construction of parental competence, and taking care of a child, rather than experiencing infertility, mourning, and the loss of not having a child [38].
Prenatal diagnostic tests showed significant decreases in prepartum depression in women undergoing ART; this result was not repeated in women with SC, whose prepartum depression levels were stable before and after the first trimester combined prenatal screening test [13]. These data are not supported by the few studies in the literature showing that during the period of the first-trimester screening test, couples with SC felt the partner was more supportive, which resulted in a lowering of depression and anxiety levels, compared to couples undergoing ART [39].
Regarding levels of men’s depression, the ART group showed higher depressive symptomatology than the NC group [40].
In particular, men in the ART group with high depressive symptomatology showed low marital relationship satisfaction in comparison to men in the ART group with low depressive symptomatology and NC with high and low depression levels. Significant differences between groups were found concerning attitudes toward sex; the ART group with high depression symptomatology had less attitude toward sex than both NC with high and low depressive levels. Furthermore, men in the ART group showed significant differences with regard to attitudes towards pregnancy and the baby; the ART group with high depressive symptomatology had more positive attitudes toward gestation and the child than the NC group with high depression levels. Once again, with regard to this attitude, the ART group with low depressive symptomatology reported fewer positive attitudes than the NC groups with high and low depressive symptomatology.
These data are relevant because they can guide clinical intervention in evaluating the psychological well-being of these men; interventions should be targeted based on gender differences [40].
Finally, as for parental competence in terms of paternal adjustment and positive attitudes toward paternity, men in the ART group with high depression levels showed lower paternal adjustment and less positive paternal attitudes than the ART group with low depressive symptomatology and men in the NC group with high and low depression levels.
However, in a study by Hakim et al. [17] only 10% of women and 3% of men showed high depressive symptomatology. Psychosocial counselling intervention is considered less useful by women and men with more depressive symptoms; moreover, counselling sessions were deemed less informative by women with high depression levels. This result leads to further reflection: counselling is often not enough for those who have to manage such a seriously compromised mood [41].
Moreover, the results indicating that women undergoing ART rated the counselling session as less informative are supported by some studies that demonstrate biases in processing and a tendency to attribute negative meaning to neutral stimuli, and enhanced processing of mood-congruent stimuli [42–44].
The hierarchical regression analysis showed a significant effect on the interaction between helplessness cognitions and anxiety and the interaction between helplessness cognitions and depression among women; in particular, patients with high helplessness cognitions and high depression levels were associated with low intentions to comply with the treatment.
Winter et al. [13] indicated no significant differences between PGD, ICSI, and SC couples, in which registered depression levels decreased between T1 (12/14 weeks of pregnancy) and T2 (20/22 weeks of pregnancy), with the lowest scores at the third month of the baby’s life (T4). However, the SC participants reached the lowest point in terms of depressive symptomatology at T2, and the ART group decreased progressively from T1 to T4.
In the literature, some authors highlight the invasiveness of the PGD pathways, in which even after 3 years, couples perceived high symptoms of depression and anxiety [46]; other authors, however, have not found fluctuations in depressive symptoms during the PGD pathways, compared to what occurs with anxiety levels [47].
Stress
As highlighted by Yoshimasu et al. [23], significant correlations were found between maternal distress during pregnancy and at 1 year after delivery: psychological distress conditions during both periods were significantly positively correlated with poor mother-to-infant bonding assessed by the total score of the K6 scale [48] and more precisely with the “lack of affection” and “anger/rejection” subscales. These results are confirmed by the literature showing the presence of high stress levels in medically assisted reproduction paths [49, 50].
Regarding psychological intervention, in both men and women with high infertility-related stress, counselling expectations were perceived as more important compared to couples with lower levels of stress; in particular, men with high infertility-related stress levels expected counselling to be more helpful, and women evaluated counselling as more important after the session than women with less stress [19].
Maternal-infant attachment
The importance of ART in the maternal and fetal relationship is under debate. For example, interestingly, anger that develops during the ART pathway could be considered as a predictor of weight at birth [50]. In this scenario, the study by Kuo et al. [21] shows the scores assessed using the Maternal-Foetal Attachment Scale [51] significantly increased as the pregnancy progressed in Taiwanese women who conceived by in vitro fertilization. In order to analyse significant interactions between covariates (the Symptoms Checklist, the Pregnancy-related Anxiety Scale, the Social Support Apgar, the Chinese Childbearing Attitude Questionnaire, and the Awareness of Foetus Scale) as a factor influencing maternal attachment and weeks of gestation (9–12–20 weeks), the generalised linear mixed model showed no significant interaction, indicating the relation between maternal attachment and each covariate did not change over the weeks of gestation. However, a high score in the Chinese Childbearing Attitude Questionnaire, the Awareness of Foetus Scale, and the Social Support Apgar were significantly associated with high maternal-foetal attachment.
Maternal-infant attachment seems to increase before the first-trimester combined prenatal screening test at around 12 weeks of gestational age (T1) and after receiving the results at 14 weeks of gestational age (T2), as shown by Udry-Jørgensen et al. [11]. More specifically, no significant differences were found between ART and SC couples, which indicated an increase in prenatal attachment in both groups, as has been pointed out by some studies in the literature [12]. Regarding the group of 18 women with clinically significant anxiety, they were significantly more depressed and less attached to their foetus than women in the low-anxiety group.
These data are confirmed by Winter et al. [13], who showed no difference between groups in couples undergoing PGD, couples in the ART group, and couples with SC. Also in this study, the maternal and paternal antenatal attachment progressively and steadily increased from the first trimester of pregnancy until 3 months post-partum. Many studies confirmed that the attachment increases as the pregnancy progresses, regardless of the conception type [38, 46, 52, 53].
Nevertheless, considering ART mothers undergoing IVF and ICSI, non-ART mothers facing ovulation induction and artificial fertilization, and mothers with unaided pregnancy, non-ART women had a more significantly positive association with low mother-infant bonding compared to the ART group and the unaided pregnancy group [25]. This provides evidence that the desire for maternity of women in medically assisted reproduction facilitates the construction of the attachment bond, compared to women who have no difficulty in conceiving.
An increased risk of maternal lack of affection, 1 of the 2 components of low mother-infant bonding, seems to be significantly associated with both the ART and non-ART groups.
The assisted reproductive technology and non-ART groups showed significant association with anger/rejection toward babies, the second component low mother-infant bonding. This association is related to multiparous women. With regard to primiparous mothers, undergoing ART was associated with lower risk of anger/rejection toward babies than women with unaided pregnancy.
Moreover, poor mother-to-infant bonding and child development were significantly negatively correlated [54–57].
To analyse the association with low mother-infant bonding and ART mothers, demographic, personal, and medical factors were compared in women with low mother-infant bonding and women without low mother-infant bonding.
The women with lower baby attachment were characterised by a significantly high proportion of primiparity, small families, high stress life-events, no positive feelings toward pregnancy, harassment from the partner, poor health, and infant physical disability.
Parental role and self-esteem
In an Iranian randomised controlled trial study [26], there were significant differences in the mean score of maternal self-esteem between the intervention and control group.
The mean scores of maternal self-esteem among mothers undergoing the preparation program showed, instantly and one month after psychoeducational intervention, significant differences compared to the score shown before the intervention. This difference was not present in the control group.
Maternal self-esteem was assessed before birth through 2 dimensions: attitude to accept the maternal role and expected interaction with the foetus during pregnancy.
As shown by the results of mean scores, the attitude to accept the maternal role was significantly different immediately after finishing the psychoeducational intervention and one month after, compared to what was detected in the phase before the start of preparation program; however, the control group did not show this difference.
Finally, concerning the expected interaction with the foetus, the intervention group revealed significant differences in the mean scores before and just after the preparation program, as well as before and one month after the end of the program. These same significant differences were also found in the control group.
The results of this study showed the functionality and the need for psychosocial interventions with couples in medically assisted reproduction paths [58–61] in a situation where we often tend to focus more attention on the biological and somatic parts of the problem.
Coping
Coping strategies assessed by Nagy et al. [14] showed a tendency to use “search for emotional balance” and “withdrawal” in couples with IVF. Moreover, these couples were less oriented to use “emotional and impulsive behaviour”, especially among men.
This indicates that couples who face a medically assisted reproduction path try to have as much control as possible over stressful situations; on the one hand, the literature shows that the feeling that you have good control of events related to fertility and pregnancy is connected to less perceived stress [62, 63]. On the other hand, hyper-control leads to hyper-activation of the arousal responses that could affect perceived stress [64].
With regard to gender differences, women in the IVF group apply each coping strategy more often in comparison with men, whereas this difference was not seen in parents in the group with a naturally conceived child.
A significant difference was found between men and woman in both groups; more specifically, mothers were “seeking social support” more and had a greater tendency towards “withdrawal” than men, regardless of the mode of conception.
Among IVF couples, the ambition for a better emotional balance changed between men and women; these data seem to indicate the presence of emotional difficulties.
Instead, the psychological immune system, understood as the integration of personal resilience resources and adaptive capacities [65], appeared stronger in IVF couples than in the naturally conceived group; the results indicated higher scores in the subscales “sense of coherence” and “creative self-concept” in the ART group.
Quality of life
In Sarafraz Yazdi’s recent study [16], there were no significant differences in the perceived QOL between women in the ART group and mothers with SC in both the first and second trimester of pregnancy. Therefore, in the second trimester the QOL scores increased in both groups compared to what was found in the first period of gestation.
Unfortunately, there is no homogeneity in the results of the studies; the literature highlights inconsistencies between the studies that showed significant associations between poorer QOL and medically assisted reproduction pregnancy [66] and those that indicated higher QOL were associated with ART pregnancy [67].
With regard to the perceived general health, women in the ART and SC groups showed a significant difference at the first and second trimesters. More specifically, women in the ART group showed lower scores in the second trimester compared to those shown in the first period of pregnancy; however, in the control group, general health scores were higher in the second trimester.
Family functioning
In Anderson’s observational study [20], parent-child relationships in families with twins or singletons born from medically assisted procreation path, whose age ranges between 6 to12, was analysed.
Mothers showed few behavioural differences in interaction with twins and singletons: less inclination to be hostile or show irritable behaviours towards twins compared to singletons.
Conversely, fathers showed many differences in the interaction toward twins compared to singletons. They were less inclined to undertake supportive communication and active listening towards twins compared to singletons. Moreover, fathers showed both higher controlling behaviours and hostile and irritable actions towards twins rather than singletons. Male parents tended to have lower communicative positive behaviours, but they also expressed less hostility towards daughters compared to sons.
It might be appropriate to consider the importance of parental competence and the quality of the parents’ responsiveness to the child, especially in cases of twin pregnancies, a risk factor that should be avoided in medically assisted reproduction paths [37], because the stress burden may become excessive for the parent.
This study highlighted statistically significant differences between twins and singletons when children’s behaviours towards mothers were analysed. In particular, twins were less inclined to show supportive behaviours towards mothers, but at the same time they were less hostile towards their mothers. Thus, twins involved fathers less in supportive communication behaviours compared to singletons, and they showed lower controlling behaviour towards fathers compared to singletons.
Clinical pregnancy rate
Domar et al. [28] focused on clinical pregnancy rates among women who were around the beginning of the first IVF cycle. The selected women were randomised in the mind/body program for infertility (MB) group and control group; the intervention group was subjected to a stress management program through cognitive behavioural therapy, relaxation exercises, and a social support path, whereas the control group was encouraged to participate by an economic reward.
The patients followed for 2 IVF cycles showed no differences in demographic characteristics and clinical conditions in both the MB group and the control group. However, results indicated higher pregnancy rates among patients who took part in the intervention program than the control group; in particular, these differences concern cycle 2 of IVF, while no differences were found during cycle 1.
Some meta-analyses show that psychosocial intervention can have effects on the pregnancy rate, especially because the intervention reduces anxiety, and this increases the possibility of obtaining the desired pregnancy [67]; however, other meta-analyses and systematic reviews underline that the results of the effective influence of the psychosocial intervention on the pregnancy rate are still uncertain due to the low quality of evidence [68].
Final considerations about the infertility pathway
The infertility pathway is a complex path with lots of grief and pain. Often, a multidisciplinary approach is undeniable [69]. Moreover, when approaching oncologic patients [70, 71] who need fertility preservation, a similar medical behaviour should be considered [72]. A noticeable and futuristic medical approach should consider the collaboration of more diversified healthcare professional figures, who join together for the physical and mental wellness of patients. For example, also in complex dangerous situations such as ovarian hyperstimulation syndrome (OHSS) [73], a medical approach should be administered in combination with adequate psychological support.
Conclusions
This systematic review has its key role in presenting the results of the last 9 years of research and studies on the psychological outcomes in an area, such as that of the medically assisted reproduction, which is relatively new and niche. The clinical interventions can be designed starting from the results of these studies; in this way, from a clinical perspective, interventions could allow the collection of data and contribute to the knowledge of the literature, and scientifically guide clinicians to the personalisation of interventions.
The shortcomings include the conflicting results, and although they all underline the importance of taking charge of the psychological variables in infertility, few studies monitor and evaluate the effectiveness of these interventions from the use of ART to the post-natal period.
Another critical issue is that none of the selected studies monitors the evolutionary implications of parental competence on the development of children born from ART. It would be desirable for future research to focus precisely on these aspects.