Purpose
Uterine cancer remains a common malignancy in European women, with a large disparity in Europe and worldwide in the incidence, treatment, and mortality [1]. Endometrial cancer continues to have an important impact on health due to the presence of risk factors, including obesity, diabetes, and exogenous estrogenic exposure [2].
Generally, treatment of endometrial cancer and early stage cervical cancer is surgery plus external beam pelvic radiotherapy (APR), and adjuvant chemotherapy in high-risk patients [3, 4].
In stage I endometrial cancer patients with intermediate- or high-risk factors, APR has been shown to increase local control (LC) and in population-based studies, also overall survival (OS) [3]. In cervical cancer, APR alone decreases loco-regional recurrence in patients with intermediate-risk factors, and concurrent chemo/radiotherapy improves overall survival in high-risk patients [4].
Moreover, in some cases, a vaginal cuff brachytherapy (BT) boost in addition to APR is necessary [3, 4]. When administering both APR and BT, the estimation of cumulative doses is crucial to assess the total dose received by both radiation target and organs at risk (OARs). In the last two decades, there have been notable advances in radiotherapy techniques by the implementation of APR with image-guided volumetric modulated arc therapy (IG-VMAT), and BT with 3 dimensional high-dose-rate (HDR). These implementations allowed for a transfer from a point-dose evaluation to a volume-based treatment planning and delivery, giving particular attention to OARs dose constrains with the advantage of limiting iatrogenic toxicity [5, 6].
Considering different fractionations and lengths of treatment of APR and BT, radiobiological summation of doses can represent a valid tool for calculating cumulative dose, derived with an α/β calculator to convert physical dose to equivalent dose of 2 Gy per fraction (EQD2).
However, as all patients have received the same prescribed doses of 50 Gy in 25 fractions of APR and 10 Gy in 2 fractions of BT, we did only the physical sum of doses, and a rigid plan fusion and algebraic sum were carried out to estimate cumulative APR and BT doses.
The current availability of modern treatment planning systems allows to perform rigid plan fusion to calculate physical and radiobiological dose summation. A condition of this method implementation is that patient submitted to APR and BT must be treated in the same supine or prone position. The advantage of algebraic sum is the possibility to evaluate cumulative doses regardless of the patient position during APR and BT.
In two Italian radiotherapy centres participating in the study, sited in Terni and Ancona, uterine cancer patients are generally treated in supine position, both during APR and BT.
The present report compares algebraic sum and rigid plan fusion methods for the evaluation of cumulative APR and BT physical doses in patients treated in supine position. However, some patients from other Italian hospitals, complete treatment with BT in our centre after APR given in the prone position. Therefore, there is a need to validate the algebraic sum method with the intention of using it in patients treated with APR and BT in different positions.
Material and methods
In the two centres, linear accelerator (LINAC), HDR unit, and treatment planning system (TPS) for APR were different, whereas HDR-BT systems to deliver vaginal boost were the same. Adjuvant pelvic radiotherapy was delivered as an IG-VMAT with 6 MV photon energies in both the centres. Moreover, the two centres followed the same guidelines and dose prescriptions. Details of equipment and techniques adopted are summarized in Table 1.
Table 1
Details of the equipment and techniques adopted
Prescribed dose was 25 × 2 Gy for all patients, target volume included proximal vagina and paravaginal tissues as well as lower common, external, and internal iliac nodes, obturator, and presacral nodes. Clinical target volume (CTV) was defined by a 7 mm expansion of nodal regions with subtraction of pelvic bones, femoral heads, and vertebral bodies. A margin of 5 mm in all directions was added to CTV to obtain planning treatment volume (PTV). Volumes of OARs, including rectum, femoral heads, spinal cord and cauda, small bowel, and bladder were also contoured. All plans were optimized, such that 95% of PTV received 95% of the prescription dose. Quantitative analyses of normal tissue effects in the clinic (QUANTEC) constrains for OARs were considered [7].
Patients’ position was verified by kV cone beam CT system integrated in linear accelerator machine for the first 3 days of treatment. Then, any variation of set-up was checked once a week. Each patient was educated to maintain full bladder and empty rectum. For BT, a computed tomography (CT)-based planning was acquired using a cylindrical vaginal applicator and bladder catheter, which was closed to maintain the organ full. Brachytherapy was given with 2 fractions of 5 Gy in 2 consecutive days to reach the total dose of 10 Gy. CTV included 3 cm of proximal vagina. Treatment plans were generated with dose prescription at 5 mm from the surface of the applicator. CT was performed only for the first BT implant. Patients were treated in supine position both in APR and BT.
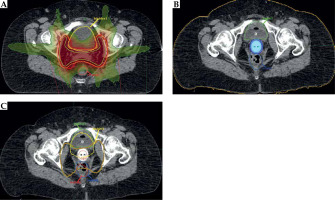
To evaluate OARs’ cumulative APR and BT doses, algebraic sum and rigid plan fusion were registered and compared using the rectum and bladder as reference organs. With algebraic sum, all dose parameters derived from APR and BT treatment plans were mathematically added, obtaining a total values corresponding to cumulative doses. The rigid plan fusion was performed using MIM-Maestro software version 6.7.7 (MIM Software Inc., Cleveland, OH, USA). To start with, CT image data set of APR were rigidly fused on CT images of BT by matching bony structures. Accuracy of the rigid fusion was carefully reviewed. Then, an addition of APR and BT doses was performed with a specific workflow that accumulated two doses of two separate CT data set using a rigid registration [8] (Figure 1).
Fig. 1
Flow chart of dose accumulation with the rigid plan fusion. Dose and computed tomography (CT) images of adjuvant pelvic external radiotherapy (A) and brachytherapy (B) were rigidly fused on a resulting CT images (C), using a software workflow
Regarding OARs, the following dosimetric parameters were examined: Dmax (0.5 cc), D20% and D50% for the rectum, and Dmax (0.5 cc) and D50% for the bladder. We decided to analyze these parameters because they are the most commonly used in clinical practice. The rectum and bladder volumes resulting from the contouring of CT-APR plan were named R1 and B1, whereas the rectum and bladder volumes delineated at CT-BT plan were termed R2 and B2, respectively. For each dosimetric parameter adopted, algebraic sum was obtained adding CT-APR and CT-BT plans calculated doses (i.e., DR1 + DR2; DB1 + DB2). The rectum and bladder cumulative dose values of R1 and R2, and B1 and B2 were extrapolated from dose volume histograms (DVHs) of accumulated dose distributions (Figure 1) in rigid fused CT plans (i.e., DcumR1, DcumR2, DcumB1, DcumB2). To obtain a dosimetric parameter, which was independent of OARs’ volumes, mean values of cumulative doses (Dmean) were also evaluated (i.e., DcumR1 + DcumR2/2; DcumB1 + DcumB2/2).
Percentages of dose differences between the algebraic sum and rigid fusion findings were reported as ∆-values. To compare the two methods, Bland-Altman plot (difference plot) was adopted. Differences between the two methods were plotted against algebraic sum, which was considered the gold standard [9]. In this statistical plot, the central horizontal line characterizes the mean difference, and upper and lower lines represent the limits of agreement, which are defined as the mean difference plus and minus 1.96 times standard deviation (SD) of the differences. Because the limits of agreement are point estimates, Bland and Altman also advised setting confidence intervals on these limits [10]. 95% confidence interval (CI) of the mean difference illustrates the magnitude of the systematic difference. If the line of equality is not in the interval, there is a significant systematic difference. If one method is higher, and the other method is higher, the average of the differences will be close to zero. If it is not close to zero, this indicates that the two assay methods are systematically producing different results. Statistical analysis was performed using a software package (MedCalc v.11.1 Broekstraat 52, B-9030 Mariakerke, Belgium) [11]. Compliance was assessed based on whether or not the program was completed. Common terminology criteria for adverse events version 5.0 was applied to grade toxicity.
Results
Twenty uterine cancer patients submitted to APR and vaginal cuff high-dose-rate BT after radical surgery were revised. In all patients treated in the supine position during both APR and BT, cumulative doses were calculated and compared using algebraic sum and rigid fusion methods.
The median age was 60 years (range, 44-84 years), and the median Karnofsky performance status was 100% (range, 90-100%). Regarding primary tumor histologies, 4 patients had squamous cell cervical carcinoma, 11 endometrioid cancer, and 5 clear cell or mixed histology endometrial cancer. Tumor stages according to FIGO (International Federation of Gynecology and Obstetrics) classification varied from IA to IIIC.
Differences between the mean cumulative doses and the algebraic sum were calculated for each dosimetric parameter analyzed. For the rectum, the percentage differences found were ΔDmax (0.5 cc) –0.8% (95% limit of agreement: –15.2% to +16.8%), ΔD20% –0.5% (95% limit of agreement: –4.7% to +5.7%), and ΔD50% 7.3% (95% limit of agreement: –42.8% to +28.2%) (Figure 2A-C). For the bladder, the percentage differences found were ΔDmax (0.5 cc) –31.9% (95% limit of agreement: –67% to +3.2%) and ΔD50% –0.6% (95% limit of agreement: –23.8% to +22.7%) (Figure 2D, E).
Fig. 2
Dose difference plots comparing algebraic sum and mean cumulative doses of rigid plan fusion with the representation of the limits of agreement (dotted lines): A) rectum Dmax (0.5 cc); B) rectum D20%; C) rectum D50%; D) bladder Dmax (0.5 cc); E) bladder D50%

For all examined parameters, the line of equality was in 95% CI of the mean difference, except for the bladder ΔDmax (0.5 cc), where 95% CI of the mean difference was –18% to –40%, an apparent significant value. Actually, this difference can be explained by the wrong estimation of real dose value. Position of the bladder during vaginal cuff BT was different from that recorded during APR. In fact, the cylindrical vaginal applicator used for BT moved the bladder forward and cranially with respect to its’ position during APR. Therefore, rigid fusion improperly recorded an excess of dose, specifically ΔDmax (0.5 cc), due to an apparent and not real positioning of the vaginal applicator inside the bladder.
After a median follow-up of 25 months (range, 6-39 months), all patients completed the treatment with a 100% of compliance. No major acute or late toxicities were registered. In particular, acute G1 diarrhea, G1 proctitis, G1 dysuria, G2 nausea were observed in 10/20 (50%), 1/20 (5%), 5/20 (25%), and 1/20 (5%) patients, respectively. One of 20 (5%) patients had late G2 proctitis, and 2/20 (10%) patients experienced vaginal stenosis.
Discussion
In uterine (endometrial and cervical) cancer patients submitted to upfront surgery, adjuvant radiotherapy is often administered as APR followed by BT [3, 4]. In these cases, there is a need to calculate the sum of doses administered to OARs resulting from the APR and BT treatments. The best method of summing the dose from APR and BT plans remains still unknown. Generally, in clinical practice a simple sum of doses is done using the algebraic sum of doses administered with each radiotherapy technique. The current availability of modern treatment planning systems allows to perform so-called ‘rigid plan fusion’, to calculate physical dose sum superimposing the APR and BT images deriving from the two CT treatment plans.
The advantage of rigid fusion with respect to algebraic sum is the possibility to estimate volume-based rather than point-based total dose, with a possible consequent clinical benefit, due to a better cumulative dose calculation to OARs and showing the cumulative dose distribution in the target area [5]. Deformable image registration has been recently discussed as a plan evaluation tool for clinical purpose to calculate dose accumulation. This method matches the regions of interest, including target volume and parts of OARs moving together with the applicator, rather than only matching BT applicator or bony structures. However in BT, target volume and parts of OARs can move together with the applicator especially after utero-vaginal implant, rather than vaginal cuff implant [12]. Of note, a condition of rigid fusion and deformable image registration is that patient submitted to APR and BT must be treated in the same supine or prone position.
The purpose of this report was to examine reliability of algebraic sum in evaluation of cumulative APR and BT doses with respect to rigid plan fusion in uterine cancer patients submitted to upfront surgery. As usual, BT is performed in supine position, while APR can be done both in supine and prone position. Considering that only patients treated in the same position can be evaluated with rigid plan fusion, patients undergoing APR in prone position were excluded, and only those treated in supine position were included in our analysis.
The comparison of the two calculation methods revealed that for the rectum, there were no differences between mean cumulative doses and algebraic sum in ΔDmax (0.5 cc), ΔD20%, and ΔD50%, and that for the rectum ΔD50%, BT contribution was minimal or zero. For bladder, ΔD50% was negligible between the methods, whereas ∆Dmax (0.5 cc) resulted quite different (31% ±17%) since the rigid fusion registered a higher bladder Dmax (0.5 cc) with respect to algebraic sum. As already explained in the Results section, this difference was a registration bias due to an overestimation of the dose associated with the bladder displacement by BT vaginal cuff applicator (Figure 1). To our knowledge, this is the first report, in which the sum of the doses between APR and vaginal cuff BT was calculated. In a few published similar studies, this evaluation was done in cervical cancer patients who were not submitted to surgery, and received only external-beam radiotherapy (EBRT) to the pelvis plus utero-vaginal BT. Also, in a recent review with the previously mentioned clinical scenario, artificial bias records were reported due to critical organs displacement by the utero-vaginal BT applicator [5].
Regarding ΔD50% parameter, both for the bladder and rectum BT, dose contribution was minimal or zero because it was mainly linked to the dose administered with APR. Based on these outcomes, dose evaluation to larger volumes of the rectum and bladder resulting from the APR and BT sum resulted not very useful. The previously mentioned review on pelvic EBRT plus utero-vaginal BT for un-resected cervical carcinomas, reaches the same as ours conclusions [5]. However, among parameters analyzed in this study, in clinical practice, most useful and reliable ones for dose sum calculation were the rectum Dmax (0.5 cc) and the rectum D20%, and no parameter for the bladder. For the bladder, other parameters need to be investigated.
Our analysis showed that algebraic sum and rigid plan fusion of doses assured similar results in evaluating cumulative OARs doses when post-surgical APR and vaginal cuff BT are performed. Moreover, a recent review concluded that direct addition of APR and vaginal cuff BT doses provides an accurate estimation of the doses received by OARs [12]. On the contrary, regarding the subset of non-operated cervical cancer patients submitted to APR and utero-vaginal BT, more sophisticated methods as rigid plan fusion and deformable image registration are recommended [13-15].
No major acute or late toxicities were registered, although the patients were in the supine position and the bowel loops should have re-entered the APR volume more easily than in the prone position [16]. Historically, results in uterine cancer patients have shown a dosimetric advantage favoring prone position to reduce small bowel doses. This finding was probably associated with the use of older radiotherapy techniques (e.g., 3D-APR) when the modulated radiotherapy procedure was unavailable, and the only way to spare small bowel was patient’s prone position with consequent displacement of the intestinal loops away from the irradiation field. Moreover, using the IG-VMAT technique, smaller PTV margins can be accepted without dosimetric disadvantages or negative consequences on set-up as indicated in the literature [17, 18]. In our experience, we added a margin of only 5 mm in all directions to obtain PTV from CTV.
Conclusions
Despite the limited number of patients analyzed and the retrospective nature of this review, this is the only study on APR and vaginal cuff BT in uterine cancer patients already submitted to surgery. In this setting of patients, algebraic sum and rigid plan fusion of doses assured similar results in evaluating cumulative OARs’ doses. Algebraic sum can be still used in clinical practice considering its’ simplicity, without the need of additional resources, its’ high accuracy in calculating bladder Dmax (0.5 cc) and the possibility of using it even when patient is not in the same treatment position, and/or when APR and BT are performed in different centres. Further investigations with increased number of patients are recommended to confirm our results.



