Purpose
Radiation therapy (RT) for prostate cancer is a well-established and effective treatment technique with various treatment options backed by randomized trials and single-institutional studies [1]. Although radiation modalities such as external beam radiotherapy (EBRT) and brachytherapy are effective in the management of prostate cancer, a concern regarding short and late toxicity plays a pivotal role in modality selection, dose, and duration of therapy, motivating recent advances in technique of delivery.
The ProtecT trial concluded no significant difference among the prostate-cancer-specific mortality rates in observation versus surgery or RT; however, they did note increased genitourinary (GU) toxicities and erectile dysfunction following surgery as well as increased gastrointestinal (GI) toxicities from RT [2]. Rectal toxicities are a limiting factor in RT for prostate cancer due to a high rectal dose attributed to the proximity of the prostate and rectum, with significantly higher toxicity correlated to dose to the inferior rectum [3,4,5]. In some patients, the degree of rectal toxicity may be a key factor governing treatment selection. Willet et al. [6] reported increased rectal toxicity associated with RT and irritable bowel disease (IBD), specifically ulcerative colitis (UC), as well as severe rectal toxicities in patients with IBD undergoing abdominopelvic irradiation. Furthermore, acute GI toxicity of grade 2 or higher is exacerbated in patients undergoing concomitant medical therapy for IBD [7]. Advances in modern RT have demonstrated a trend toward improved toxicity profiles from treatment in high-risk groups such as patients with IBD [8,9].
Although advances in image-guided radiation therapy (IGRT) and treatment technique may facilitate the use of RT in patients with a concern for rectal toxicity, modern trends in EBRT and brachytherapy application towards dose escalation and hypofractionation contribute to renewed concern regarding sparing rectal dose. Several reports and phase III clinical trials incorporating patients of varied risk stratification have demonstrated improved biochemical control with modern dose escalated EBRT [10,11,12,13,14,15]. Given favorable therapeutic ratio and logistic advantages, moderate and extreme hypofractionation have been a focus of recent randomized trials of the past decade [16,17,18,19,20]. Although not conclusively shown in the majority of hypofractionation trials to date, there have been reports of increased rectal toxicity associated with larger dose per fraction [21].
Brachytherapy remains a curative alternative to radical prostatectomy or EBRT for early stage disease, with no significant differences in treatment results but lower rates of urinary incontinence and increased preservation of sexual function [22]. Trends in brachytherapy have similarly explored dose escalation and completion of treatment within fewer sessions with high-dose-rate (HDR) techniques [23]. Although late grade 3 rectal toxicity is rare following definitive upfront brachytherapy, well below 5% in most series, dosimetric rectal outcome has been shown to be overall improved with HDR compared to EBRT [24]. In instances of salvage brachytherapy following biochemical failure post-EBRT, a higher incidence of grade 2/3 rectal toxicity has been reported in low-dose-rate (LDR) and HDR series [25]. When considering upfront treatments in the recent ASCENDE-RT trial, addition of brachytherapy boost to 78 Gy EBRT demonstrated an increase in grade 3 rectal toxicity from 3.2% to 8.1% [26]. In patients receiving HDR monotherapy (19 Gy in single fraction), Krauss et al. [27] reported grade 1/2 acute and chronic GI toxicities in 12%/0% and 12.1%/1.7% of patients, respectively, and Prada et al. [28] reported acute grade 1 GI toxicities up to 7%, with no grade 2 acute or grade 1/2 chronic GI toxicities. It is likely that further techniques designed to improve rectal dosimetry in the context of brachytherapy will continue to lead to less acute and late toxicity.
Displacement of normal tissue has long been explored as a viable strategy to improve dosimetry to organs at risk (OARs) [29]. For prostate RT, a novel technique for sparing high-dose to the anterior rectal wall is the use of a synthetic gel injection into the space between the prostate and rectum [30,31,32,33,34]. The feasibility and effects on toxicity of these rectal displacement gels has been reported by various investigators. Prada et al. [35] reported the successful use of a rectal wall displacement technique in single fraction HDR brachytherapy as monotherapy, with no additional toxicities and the same biochemical control at 32 months. Strom et al. [36] reported successful implementation of a polyethylene glycol (PEG) hydrogel for HDR brachytherapy plus or minus intensity-modulated radiation therapy (IMRT), with significantly increased prostate-rectal distance and significantly decreased mean rectal doses. Yeh et al. [37] similarly looked at a PEG hydrogel for HDR brachytherapy plus or minus IMRT and also reported increased prostate-rectal distance as well as low acute and chronic rectal toxicities despite aggressive dose escalation. SpaceOAR (Augmentix Inc., Waltham, MA, USA) is an FDA-approved gel, evaluated as having a benefit in reducing rectal dose, toxicity, and quality of life declines by a phase III trial with a median follow-up period of 3 years [33,38,39]. At our clinic, SpaceOAR is typically injected under ultrasound guidance at the conclusion of an HDR prostate procedure performed prior to external beam hypofractionated prostate RT, while patients are under general anesthesia. The use of SpaceOAR for these patients has effectively reduced high-dose to the rectum consistent with that shown in the phase III trial previously mentioned. Here, we report the potential benefit of injecting SpaceOAR prior to a monotherapy HDR prostate implantation, with the primary goal of mitigating GI toxicity due to UC.
Case presentation
A 73-year-old patient initially presented with an elevated prostate-specific antigen (PSA) of 9.94 ng/ml. He received a prostate biopsy, which confirmed intermediate-risk adenocarcinoma of the prostate, GG 2 stage IIB (cT2bN0M0, Gleason score of 3 + 4 = 7 in 3/12 cores). Brachytherapy with 19 Gy in a single fraction with SpaceOAR was chosen as monotherapy for this patient instead of EBRT due the patient’s UC and concomitant medication use of azathioprine.
The SpaceOAR gel implantation was performed 18 days prior to the HDR procedure in sterile dorsal lithotomy position with an ultrasound stepper and transrectal ultrasound (TRUS). This timing was a result of logistical and scheduling considerations between the time of injection and the HDR procedure. A waiting period of at least three days before HDR is necessary to allow local gas to adequately resolve, restoring visualization of the prostate gland, which is immediately lost following the injection. Using 1% lidocaine, the perineum was numbed, followed by the prostatic neurovascular bundles via TRUS guidance. The SpaceOAR needle was then advanced to the mid prostate at midline, and a 1 cc injection of saline was used to identify the correct position posterior to the prostate and completely anterior to the rectum. SpaceOAR was then attached and injected to completion. At Jefferson hospital, the average SpaceOAR volume injected into patients receiving hypofractionated EBRT following HDR prostate treatment is 10.5 cc (range, 6.88-14.08 cc) as seen on magnetic resonance imaging (MRI). The SpaceOAR volume used in this case as seen on MRI was 13.19 cc and unintentionally asymmetrically displaced slightly to the patient’s left during injection. Injection volume varies with application [30,34].
For the monotherapy HDR prostate brachytherapy procedure, the patient was in dorsal lithotomy position and induced under general anesthesia. A Foley catheter was inserted. Rectal preparation was verified, and perineum was prepped with betadine. A TRUS probe with a brachytherapy ultrasound stepper was inserted into the rectum, and the prostate was visualized and measured to be 39 cc. Using a template-based approach, 17 catheters were inserted from anterior to posterior prostate in a modified periphery loading technique. Catheter positions were verified in the transverse and sagittal positions and depths were confirmed. The target volume, normal tissues (rectum and urethra), and SpaceOAR were contoured by the attending physician, and real-time inverse planning (Nucletron Oncentra® Prostate v.4.2.2.4) was performed by physics. All constraints were met as follows: Prostate – V100% > 95%, V150% < 35%, V200% < 12%; Urethra – Dpoint max < 120%, D10% < 115%; Rectum – Dpointmax < 90%, V80% < 0.2 cc [27]. After plan checks by the physician and physicists, catheters were connected to the microSelectron® v2 Ir-192 HDR afterloader (Nucletron, The Netherlands) and the treatment was delivered via Nucletron Oncentra® TCS. After delivery, catheters were removed, perineum was cleaned, and the patient was extubated. The procedure was tolerated without incident.
Discussion
The SpaceOAR is placed between the ultrasound probe and needles, thus it was hypothesized to decrease visualization of the needles due to the potential for various distorting effects seen in ultrasound such as reflection, refraction, and shadowing that occur at tissue interfaces. Consistent with vendor literature, there was no visual hindrance or distortion of the needles due to the gel and the gel was clearly visible on the ultrasound image (Figure 1). After analysis, this makes sense since the SpaceOAR gel had an average Hounsfield Unit (HU) value of 7 based on the average SpaceOAR HUs from the CT scans of patients previously treated at our institution, which is very close to water (HU = 0) and should therefore have a similar density and acoustic impedance resulting in minimal ultrasound distortion. Maintaining satisfactory image quality validates the feasibility of utilizing SpaceOAR prior to HDR as a rectal protector for patients with UC. It is interesting to note, however, that there is a large discrepancy in SpaceOAR volume between ultrasound (5.622 cc) and MRI (13.19 cc). Part of this discrepancy arises from the superior resolution and quality of the MRI. Discrepancies also arise from the displacement of anatomy due to the rectal ultrasound probe. The large SpaceOAR volume discrepancy between ultrasound and MRI has no impact on patient care; however, is important to consider.
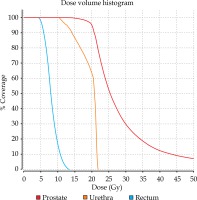
Fig. 1
Axial slices from an ultrasound image taken before (left; four anchor needles only) and after (right) complete needle implantation during an HDR brachytherapy prostate procedure post-SpaceOAR injection. The SpaceOAR gel (surrounded by red arrows in right image) and implanted needles (bright spots) are clearly visualized
The dosimetric benefit of increasing prostate and rectal separation is the primary objective of using the SpaceOAR gel during HDR prostate implantations. This can be seen in the craniocaudal direction on the sagittal image (Figure 2) and anteroposterior direction in the axial images (Figure 1 and Figure 3). The average distance between the closest needle and the rectal wall in the past ten HDR prostate procedures at our institution was 3 mm (median, 2.9 mm; max, 6.3 mm; min, 0.4 mm). Utilizing SpaceOAR, the distance between the closest needle and the rectal wall lacking SpaceOAR averaged 6 mm, and the distance between a needle within the region of the SpaceOAR and rectal wall was greater than 8 mm. In regions of no SpaceOAR, its contralateral presence increased the prostate-rectum spacing. This increased separation and shift in isodose lines is beneficial due to the large dose gradient obtained with an Ir-192 source (Figure 3). In a phase I study done at our institution to assess the safety, tolerability, and preliminary efficacy of HDR brachytherapy in combination with hypofractionated VMAT in intermediate-risk prostate cancer, the following median dosimetry was reported for 22 patient plans [40]: Prostate – V100% = 96.3%, V150% = 39.4%, V200% = 15.3%; Urethra – V118% = 1.39%, D2cc = 71.7%; Rectum – V75% = 1.3 cc. This case achieved: Prostate – V100% = 97.3%, V150% = 35%, V200% = 14.5%; Urethra – V118% = 0%; Rectum – D2cc = 51.6%, V75% = 0 cc (Figure 4).
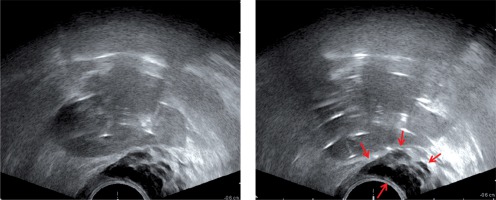
Fig. 2
Sagittal slice from an ultrasound image after complete needle implantation during an HDR brachytherapy prostate procedure post-SpaceOAR injection with overlaid contours. Please note that the poor image quality results from this image’s reconstruction from an axially acquired ultrasound and that the contours were generated in the axial view where image quality is adequate. This image is meant for visualization of the gel’s craniocaudal displacement of the prostate
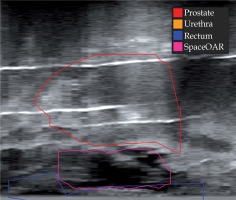
Fig. 3
Isodose distribution and contours from the HDR brachytherapy prostate implant overlaid on the ultrasound image
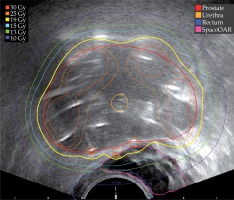
Using a more conservative α/β of 3 Gy for rectum, max equivalent dose at 2 Gy per fraction (EQD2) to 2 cc of rectum was 25.1 Gy, in accordance with GEC-ESTRO recommendations to include a D2cc to rectum less than 75 Gy by EQD2 [41,42]. SpaceOAR resulted in better dosimetry for all critical dosimetric indices as reported in our phase I trial [40]. QUANTEC guidelines suggest a conservative DVH constraint set for the rectum of V50Gy < 50%, V60Gy < 35%, V65Gy < 25%, V70Gy < 20%, and V75Gy < 15% [3]. As our D2cc rectum was 25.1 Gy after EQD2 conversion using an α/β of 3 for late effects, these dose constraints were easily met. This is likely attributed to an ideal implant in addition to increased prostate-rectum spacing, which allowed the optimizer to effectively utilize posterior catheters.
SpaceOAR did not impede standard procedure times, which is important as the patient is under general anesthesia and complication probabilities increase with increased duration of the procedure. The time from patient intubation to HDR initiation was 211 minutes, which is on par with our average HDR prostate procedure time of 203 minutes taken from eight previous procedures. However, there are many variables contributing to procedure time, which makes it difficult to assess and compare actual times on a case-by-case basis. Additional patient safety factors created by SpaceOAR are buffer space between needle placement and the rectum, which decreases the probability of rectal perforation. Mariados et al. [30] report no device-related adverse events or rectal perforations during the use of the spacer and discuss ease of use for applying the spacer with 98.7% placement success.
Conclusions
SpaceOAR successfully increased catheter-rectal wall spacing and decreased rectal dose due to improved planning capabilities, while decreasing the likelihood of rectal perforation. Although difficult to directly conclude given the lack of prospective randomized series, incorporating techniques to increase prostate-rectal wall separation may be of particular benefit to high-risk patients. This technique is prominent in EBRT and may be of interest in brachytherapy incorporating HDR hypofractionated treatment. This particular case report demonstrates one application of this concept in a patient with UC with favorable dosimetric outcome. The patient tolerated the SpaceOAR injection and HDR brachytherapy procedures well. At five months, one week, and one day follow-up, the patient reported no bowel issues following HDR brachytherapy.