White fibrous papulosis of the neck (WFPN) is a relatively new and rare disease. It was first described by Shimizu et al. in 1985. WFPN is characterized by the appearance of multiple papules with a diameter of 2–3 mm, and not attached to hair follicles. They are smooth, ivory, and often confluent. Most often sides and back of the neck are affected, but lesions may also spread across the upper part of the trunk [1]. Differential diagnosis should include pseudoxanthoma elasticum due to nearly identical clinical presentation and many common features on histological examination. Causes of these both diseases have not been fully elucidated, but aging of the body and environmental factors play a role in their pathogenesis [2].
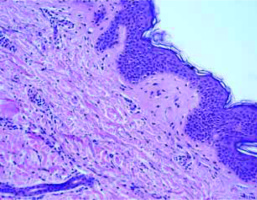
We present the case of a 57-year-old woman, a teacher with a several-year history of skin lesions on both sides of the neck. The patient denied prolonged exposure to sunlight as well as rubbing or scratching affected areas. Considering other diseases, she suffered from mild and well-controlled arterial hypertension treated in the cardiac clinic. She did not have any symptoms suggestive of vascular, gastro-intestinal, and ocular disorders; they were absent in other family members as well. Dermatological examination revealed numerous, discrete, whitish, papular lesions located predominantly on both sides of the neck and the nape (Figures 1). Biopsy performed 2 years before had shown no typical features of any of the dermatoses. The patient had not undergone any dermatological treatment. The current biopsy revealed a piece of skin with a slightly thinned epidermis and orthokeratosis; only in the central part, foci of mild acanthosis were present. The granular layer was visible along the entire length of the sampled tissue. In the dermis, scanty and diffuse lymphocytic infiltration with a tendency to gather around vessels was present. In the central part of the lesion, the presence of hair follicles and sebaceous glands with more abundant lymphocytic infiltration was visible (Figure 2). It is worth noting that in the papillary layer and in the upper part of the reticular layer, a thinning of collagen fibres without an increased vascular proliferation was present. The elastic fibre pattern assessed with elastic van Gieson (EVG) (Figure 3) and Fontana-Masson stain revealed a reduced number of those fibres (Figure 4). The presented patient has not started any of the proposed treatments for her skin lesions. She remains under observation care of our dermatology outpatient clinic.
Figure 1
Discrete, whitish, papular lesions located predominantly on both sides of the neck and the nape

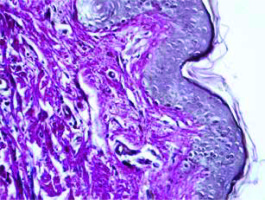
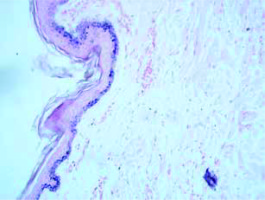
Figure 2
Histological findings – foci of mild acanthosis in the central part, the granular layer was visible along the entire length of the sampled tissue. In the dermis, scanty and diffuse lymphocytic infiltration with a tendency to gather around vessels. The presence of hair follicles and sebaceous glands with more abundant lymphocytic infiltration in the central part of the lesion
WFPN was first described by Shimizu et al. in 1985. Its clinical presentation include multiple, usually asymptomatic, whitish, and firm papules located on the lateral and posterior part of the neck. They may be of a different number and diameter, but rarely affect other areas than the neck such as the trunk and arms. No comorbidities were found to be associated with WFPN. Coexistence of a cardiovascular disease seems to be casual; it seems to be related more to the age of the patient than to the described disease itself. In the literature, there are no reports on the association between those skin lesions and medication [3]. No association with patients’ ethnicity was found either; few cases have been described among white, black and yellow people [4, 5]. The majority of patients are middle-aged women; the youngest described patient was 39 years old. The mean age of patients suffering from WFPN is over 60 years. Only few case studies on WFPN include male patients [4, 6].
On histology, white fibrous papules of the neck are characterized by mild, focal growth and thickening of collagen fibres in the papillary layer of the dermis. Elastic fibres may be physiologic, normally arranged or in a slightly decreased number [7, 8]. Ultrastructural studies show no abnormalities of the elastic fibres; collagen fibres present with a slight increase in their diameter and are tightly compacted. It is believed that those changes are non-specific features of papillary dermal fibrosis associated with structural collagen changes and/or abnormalities of the extracellular microenvironment mainly resulting from ageing of the skin.
The differential diagnosis should first of all include pseudoxanthoma elasticum. Table 1 presents features that should be taken into account when making a diagnosis [2].
Table 1
Differential diagnosis of white fibrous papulosis of the neck (adapted from Kandhari et al.)
Due to unclear aetiology, no causative treatments for WFPN have been established. First of all, the treatment should focus on flattening the lesions in order to achieve good, acceptable aesthetic result to the patients. Papers from the literature describe cases treated with a laser. Lueangarun and Panchaprateep reported a case of WFPN treated with a non-ablative fractional 1550-nm Ytterbium/Erbium laser [9]. Ho and Jagdeo claim that a good cosmetic result achieved using CO2 laser applications is associated with a reduction in itching perceived by a patient [10]. Other treatment options include protection against exposure to sunlight, particularly UVA. Also, topical preparations with retinoids seem to be well accepted by treated women.