INTRODUCTION
Total rhinoplasty allows reshaping of the nose and correction of anatomical defects, leading to improved aesthetic appearance and enhanced nasal function [1]. However, the outcomes are not always fully predictable, even when the procedure is performed according to the established standards. This unpredictability is more pronounced compared to other facial plastic surgical procedures, due to the complex anatomy and three-dimensional structure of the nose [2].
In addition, rhinoplasty can result in many complications that may occur in the early and late stages of recovery. Early complications of rhinoplasty include perioperative bleeding, tissue oedema, hematoma, sensory impairment, obstruction of the nasal passages, or infection. Such complications may lead to prolonged tissue healing and greater pain intensity, which may result in poorer postoperative cosmetic outcomes [3, 4]. Additionally, late complications include persistent oedema, asymmetry, perforation of the nasal septum, nasal respiratory impairment, mental disorders associated with an altered perception of one’s own body, and the recurrence of the bony or cartilaginous hump, which may impair surgical outcomes. Therefore, reoperation may be required. The most common causes of hump recurrence include incomplete resection of the hump, failed osteotomy, cartilage memory (the tendency of the cartilage to revert to its original shape), or the formation of an extensive internal scar.
We presented the case of a 22-year-old female patient who was diagnosed with a pilonidal cyst, which was an unusual cause of the recurrence of the cartilaginous hump after primary rhinoplasty.
OBJECTIVE
Raising awareness about pilonidal cysts as a potential cause of secondary nasal deformities after rhinoplasty.
CASE REPORT
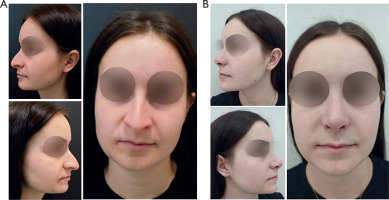
A 22-year-old female patient presented to the plastic surgery clinic for total rhinoplasty due to unsatisfactory nasal appearance and impaired nasal patency. She had no history of chronic diseases or allergies and denied regular medication use. On examination, the nose appeared disproportionately large relative to her face, with a nasolabial angle of approximately 90°, a prominent dorsal hump, and wide, long nasal wings (fig. 1 A). Anterior rhinoscopy revealed a deviated nasal septum and hypertrophy of the nasal turbinates, corresponding to her symptoms of nasal obstruction. The planned procedure included total septorhinoplasty via an external approach using the piezoelectric technique, resection of the bases of the nasal wings, and nasal turbinoplasty.
Figure 1
A – The patient’s condition before primary surgery. B – The patient’s condition after primary surgery
Open structure rhinoplasty was performed. The surgical procedure involved resection and reposition of the nasal septum, nasal bone remodelling, including the removal of the hump using a piezoelectric saw, narrowing of the nasal pyramid following low-to-high lateral osteotomies and reconstruction of the nasal dorsum using cartilaginous spreader flaps.
The procedure in the cartilaginous part involved remodelling of the lateral crura of the alar cartilages, their base reduction and nasal tip plasty. The bases of the nasal wings were reduced in size. Hypertrophied middle nasal turbinates were contracted to achieve a functional improvement. The surgery was completed as planned, and no early postoperative complications were reported (fig. 1 B). The patient attended follow-up visits regularly.
Approximately 2 months postoperatively, the patient returned due to recurrence of a dorsal hump in the supratip break region (fig. 2 A). On examination, the nodule’s texture was consistent with cartilage, raising suspicion of either a displaced cartilage fragment or early callus formation. Initially, a conservative wait-and-see approach was adopted. However, due to progressive growth and evident skin tension, revision surgery was performed 2 months later.
Figure 2
A – The patient’s condition after the recurrence of the nasal dorsal hump. B – Intraoperative image – dissected nasal dorsum with an encapsulated structure, including yellowish cheese-like contents that oozed following the incision
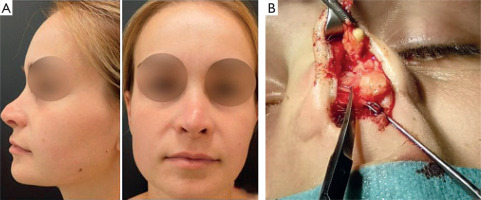
The revision was carried out via an external approach, using the previous scar. Upon dissection of the nasal dorsum, an encapsulated structure was identified and excised. Yellowish, cheese-like material was noted within the structure (fig. 2 B). Histological assessment confirmed the diagnosis of a pilonidal cyst. No complications occurred during revision surgery, and the postoperative recovery was uneventful. A satisfactory and durable cosmetic outcome was achieved without the need for additional procedures (fig. 3). Follow-up over the past year has shown no nasal tip drooping or lesion recurrence.
DISCUSSION
From the clinical perspective, as regards postoperative hump recurrence, the time criterion is crucial since it allows for the differentiation between persistent and recurrent humps [5]. The former are a direct consequence of poorly planned surgery and manifest early, mainly after the resolution of postoperative oedema. They are almost always caused by insufficient lowering of the nasal septum, which usually occurs as a result of the impaired intraoperative assessment caused by soft tissue oedema or a slight lowering of the bony part of the nose during the final stages of nasal remodelling, including the placement of an external splint. In turn, recurrent humps are visible only during the later stages of recovery. Based on the time of their occurrence, recurrent humps of the nasal dorsum can be classified into early (weeks after surgery) and late (months after surgery) humps. They can occur due to the instability in the keystone area or poor dorsal stability [6].
This case is atypical, as the recurrent nasal dorsum deformity was caused by a pilonidal cyst. According to published reports, pilonidal cysts in this location are almost exclusively post-traumatic [6]. Dermatology Review/Przegląd Dermatologiczny 2025/3 To our knowledge, there are no documented cases of iatrogenic pilonidal cysts occurring secondary to aesthetic or functional rhinoplasty, as observed in the present case.
A pilonidal cyst, also known as a hair cyst or epidermal cyst, is characterized by the inflammation of the skin and subcutaneous tissue that mainly manifests as a painful fluctuating nodule. The duct of the cyst is lined with squamous epithelium with which an abscess cavity or additional ducts can be connected. Sometimes, hair that does not have contact with the skin emerges from the hair follicles. Visible elevations of granulation tissue with oozing seropurulent discharge can occur. A pilonidal cyst affects about 0.7% of the population [7]. It is significantly more prevalent in men than in women (4–3 : 1) and mainly affects young adults before 25 years of age [8]. It rarely occurs in patients over 60 years of age [9, 10]. Most authors consider the hair cyst to be an acquired disease, although others take into consideration its congenital nature [11].
In most cases, however, the disease is primarily caused by an inflammatory reaction triggered by hair penetrating the sinus [12]. In this case, the hair should be treated as a foreign body whose penetration triggers a defensive reaction of the body. Risk factors for pilonidal cysts include poor access to air, humid environment, trauma or infection caused by anaerobic bacteria. Hair, bacteria, exfoliated epidermis and secretions from the hair follicles are absorbed deep into the skin, and keratin masses block and expand the hair follicles, leading to infection and abscess formation [13]. The blockage can be caused by excessive sebum production, dead skin cells, or external pressure on the hair follicle. Pilonidal cysts occur mainly in the intergluteal cleft. However, they can also occur in other areas where hair follicles are present, such as the scalp, face, neck, back, chest, armpits, or groins [14]. Studies also reported the location of the hair cyst on the nasal dorsum [15–17]. Most hair cysts on the nasal dorsum are post-traumatic [18]. In our study, it was an iatrogenic hair cyst of the nasal dorsum, which was a complication of primary rhinoplasty performed for aesthetic reasons.
In our patient, the most probable cause of the pilonidal cyst was the ingrown hair to the incised mucosa in the cartilaginous nasal dorsum. The lesion developed progressively, causing a gradual deformity of the cartilaginous part of the nasal dorsum. Considering the histological findings of the lesion and slight erythema of the skin above the lesion, the ex-post justification of the suspicion of such an anomaly in the region of a persistent cartilaginous hump should be considered. In turn, the atypical location of the lesion justified the suspicion of a more typical cause of the lesion. In retrospect, ultrasound might have allowed the differentiation between a dermoid cyst/teratoma and a pilonidal cyst. Importantly, due to the atypical clinical presentation, the suspicion of a cyst in this region is not the most probable diagnosis. Given the extreme rarity of pilonidal cysts occurring on the nasal dorsum – documented in the literature as isolated case reports – there is currently no standardized management algorithm for this clinical entity. Each case should be approached on an individual basis, adhering to the fundamental principles of plastic and reconstructive surgery, with meticulous attention to tissue preservation and optimal aesthetic outcome through minimization of postoperative scarring. However, the surgical approach for a persistent hump with a subcutaneous nodule remains the same. It involves the removal of pathological tissue using either an internal or external approach, depending on the surgeon’s preference and the technique previously employed. The same principles were applied in this case, resulting in a satisfactory outcome.
CONCLUSIONS
A hair cyst is a very rare cause of nasal dorsum deformity and may result from a congenital defect, trauma, or prior surgery. Further evaluation is necessary when the clinical presentation of a recurrent nasal hump is inconclusive. The differential diagnosis should include a dermoid cyst or teratoma. Surgical excision of the cyst provides a definitive treatment.









