Folliculitis decalvans (FD) and lichen planopilaris (LPP) were initially categorized as neutrophilic and lymphocytic scarring alopecia [1]. However, it is now recognized that they can occur together, leading to the recognition of a new condition called FD LPP phenotypic spectrum disease (FDLPPPS) [2]. Herein, we present the case of a male patient with the coexistence of FD and LPP, a little-known condition.
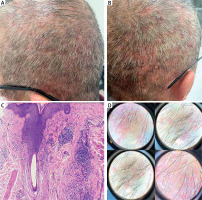
A 52-year-old male patient presented to the dermatology clinic with complaints of acne on his scalp and increased hair loss over the previous year. The patient had previously received various treatments, including systemic antibiotics, topical antibiotics, topical steroid lotions, and topical antifungal shampoos, but did not experience any improvement. The patient had a history of benign prostatic hyperplasia but did not take any regular medications. Dermatological examination revealed erythema, alopecia, and pustules in the vertex and parieto-occipital regions (Figures 1 A, B). A punch biopsy obtained from the area with alopecia on the scalp revealed anagen hair follicles and follicular stellae under the epidermis, showing mild acanthosis with fibrinopurulent exudate on the surface. Additionally, lamellar fibrosis and moderate mononuclear inflammatory cells were observed around the hair follicle, along with a fibrous tract extending perpendicular to the surface, surrounded by mononuclear inflammatory cells (Figure 1 C). The dermatoscopic examination also showed white scales around the follicles, absence of follicular openings, and milky-red areas (Figure 1 D). A culture taken from the patient’s pustule showed methicillin (oxacillin)-sensitive Staphylococcus aureus. Based on the clinical, trichoscopic, and histopathological features, the patient was diagnosed with folliculitis decalvans and lichen planopilaris. Treatment was initiated with trimethoprim-sulfamethoxazole followed by maintenance therapy with hydroxychloroquine. However, the patient showed a minimal response to treatment at the 1-month follow-up.
Figure 1
A, B – Erythema and pustules in alopecic areas. C – Fibrosis and inflammation around the follicle (H and E, ×100). D – Perifollicular white scale, red areas without follicle opening, erythema, and milky white areas
The hypothesis for the etiopathogenesis of FDLPPPS is that the altered microbiome of the hair follicle stimulates an abnormal immune response, leading to an inflammatory reaction that results in follicle destruction (scarring alopecia) and a secondary bacterial infection [3]. The clinical findings of FDLPPPS, mostly in the vertex, include alopecic patches, erythema, pustules, crusts, scales, and polytrichia, whereas trichoscopy shows milky-white areas, tufts, perifollicular yellow or white scales, and linear or arborizing vessels [2]. The histopathology of FDLPPPS has reported impaired hair follicle structure, loss of sebaceous glands and follicles, compound follicles, follicular epithelial atrophy, perifollicular fibrosis, inflammation with a predominance of lymphocytes and plasma cells, and perifollicular granulomatous infiltrate [2]. When FD and LPP coexist, the prevalent remedies include antiseptics, topical or systemic steroids, antibiotics, isotretinoin, dapsone, hydroxychloroquine, and immunosuppressive drugs (such as methotrexate) [4]. Adalimumab, a TNF-α inhibitor, has also been attempted as a therapeutic option because the disease is resistive to the majority of medications [4].
In our case, widespread pustules and cicatricial alopecia areas were present in the parieto-occipital region, and histopathology showed inflammation with a predominance of mononuclear cells. This condition, which is challenging to treat and has different clinical and pathological features than FDLPPPS, will contribute to a better understanding of the disease.








