Lichen nitidus is clinically characterized by the presence of multiple discrete papules that are tiny, shiny, and of varied colours. They most commonly occur on the neck, trunk, forearms, abdomen and the genitalia, however cases with generalized skin involvement have also been reported. Skin lesions are usually not accompanied by any additional symptoms with a sporadic exception of mild pruritus [1]. The differential diagnosis of lichen nitidus includes follicular eczema [2], frictional lichenoid dermatitis, lichen scrofulosorum, pinpoint polymorphous light eruption, and papular urticaria [3].
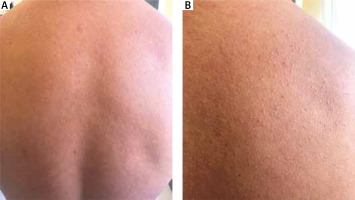
One example is a 45-year-old man with a 1.5-year history of recurrent lesions situated on the upper part of his back. The first symptoms appeared in the interscapular area with a tendency to widen the area to cover the entire surface of the back. The physical examination revealed numerous shiny papules of the colour of the surrounding skin, 1–2 mm in diameter (Figure 1). There were no pathological changes on the mucous membranes or on the nails.
The treatment so far has involved topical retinoids, glucocorticoids, and antihistamines; there was a noticeable improvement, but the symptoms worsened after drug discontinuation.
Diabetes was diagnosed during hospitalization, and no other pathology was found in the results of laboratory tests. The patient reported that he smoked about 30 cigarettes a day.
The dermoscopy performed (DermLite DL4 3Gen, 10-fold magnification, polarized) revealed the presence of white oval but irregular, structureless areas with a peripheral halo with pinkish pigmentation (Figure 2 A).
Figure 2
A – 10-fold polarized dermoscopic examination. B – A histopathologic picture with haematoxylin-eosin staining
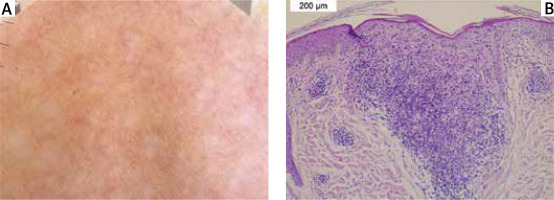
Histopathological evaluation of the 3 mm punch biopsy taken from the lesion showed a skin fragment with a single hair follicle on the left side. In the central part, there is a well-delineated mononuclear cell infiltration closely adjoining the epidermis. The epidermis at this height is thinned and covered with a compact layer of keratin and focally parakeratin. This contrasts with the normal basket keratin layer of the remaining epidermis. Increased rete peg laterally adjoins the infiltration on the right side. Sparse lymphocytic infiltrations are present around the vessels of the superficial plexus.
Although diagnosis is mostly clinical, some of the cases require histopathological confirmation for this entity [3].
The histopathologic findings of lichen nitidus are characteristic, consisting of well-circumscribed infiltrate of lymphocytes and histiocytes expanding the papillary dermis, enclosed by the rete ridges in a “ball and claw” configuration. The overlying basal epidermis can show vacuolar interface change [4].
The first dermoscopic description of lichen nitidus dates back to 2015 [5]. Dermatoscopic examination typically reveals roundish, well-defined, white areas devoid of physiological skin markings, which is a very relevant dermoscopic clue [6].
In terms of dermoscopic–pathologic correlations, whitish areas correspond to the dense dermal lymphohistiocytic inflammatory cell infiltrate, which lies in close proximity to the thinned epidermis and is enveloped by bordering elongated rete ridges (“claw clutching a ball” appearance) [7].
Depending on the location of the skin lesions, the lichen nitidus variant and magnification, different dermoscopic features could be found.
In palmoplantar lichen nitidus, Qian et al. described linear scales in parallel discontinued by oval, well-defined depressions and surrounded by ring-shaped, silvery-white scales, and the long axis of the depressed patterns was parallel to the lines of scales. Fewer and finer scales on the surface of depressed areas were found [8].
Durusu et al. reported a case of palmar lichen nitidus, with a dermoscopic picture of fine round to ovoid comedo-like central depression areas surrounded by white halo-like scales and white linear scales connecting the whole structure [9].
In the perforating variant, Martinez-Mera et al. described a central light-brown keratin plug surrounded by a whitish cloud-like area [10]. Li et al. presented a similar finding with a whitish-brownish area with a keratin plug in the centre, a structureless whitish annular cloud-like area, and a peripheral halo with a delicate brown pigmentation [11]. LeWitt et al. described pale-white papules with radial ridges emanating in a “sunburst” pattern from a depressed central keratotic core rimmed by a fine white scale. Some lesions had a pink hue and exhibited radial, linear and hairpin vessels [12].
In actinic lichen nitidus, Shrestha et al. described shiny, round, bluish-white streaks with a “fern leaf” appearance, interspersed between brownish reticular networks. Areas of koebnerization appeared as shiny linear streaks mimicking “shooting stars”.
Malakar et al. and Mohta et al., in their publications, reported a dermoscopy of lichen nitidus that showed a brown shadow within white circles [13, 14].
Jakhar et al., under 200x magnification, distinguishing between used dermoscopic mode described: absent dermatoglyphics, radial ridges, central depression, peripheral scaling (non-polarized) and ill-defined hypopigmentation, diffuse erythema, and linear vessels (polarized) [3].
Dermoscopy can also be used for differential diagnosis of lichen nitidus, as was described for follicular eczema and frictional lichenoid dermatitis. The first diagnosis shows roundish, keratotic, whitish areas with blurry margins, which are equidistant from one another. Frictional lichenoid dermatitis typically features discrete, more or less defined, whitish areas with retention of the normal skin furrows and regularly arranged dotted vessels [2].
Lichen nitidus is a rare disease for which a physical examination is often sufficient to diagnose it. In unclear situations, a skin biopsy is taken for histopathological examination, and dermatoscopy can be a valuable auxiliary examination facilitating diagnosis.