Eosinophilic annular erythema (EAE) is a rare eosinophilic skin condition characterized by annular erythematous plaques with dense tissue eosinophilia. Its presentation is usually characterized by annular and arcuate urticarial plaques, and there are only a few case reports of bullous lesions in EAE. Here, we present a rare case of EAE with generalized bullous lesions.
A 59-year-old woman came to our hospital with a 1-month history of multiple annular erythematous plaques on her trunk and limbs. The patient had a past history of asthma, hypertension, uterine fibroids and did not have any other diseases or family history. Physical examination showed multiple annular erythematous plaques on her trunk and limbs. Some of those erythematous plaques had multiple vesicles at the periphery (Figures 1 A–C). Nikolsky’s sign was negative.
Figure 1
A–C – Multiple annular erythematous plaques on her trunk and limbs. Some of those erythematous plaques had multiple vesicles at the periphery. D – Histopathological findings of the lesions. Subepidermal bulla with prominent oedema in the superficial dermis was seen/noted. A prominent infiltrate of eosinophils was observed in the superficial dermis and subepidermal bullae (HE stains, original magnification: 400×). E – One week after treatment. Erythema and bulla disappeared significantly
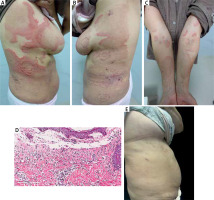
Laboratory investigations revealed normal eosinophils in blood routine examination. Liver functions, serum immunoglobulin (Ig) E, blood lipid, antinuclear antibodies (ANA), extractable nuclear antigen (ENA), bone marrow examination, blood smear, autoantibodies, parasite infection and tumour screening were all negative. A skin biopsy revealed subepidermal bullae with prominent oedema in the superficial dermis without basal cell vacuolation (Figure 1 D). A prominent infiltrate of eosinophils was observed in the superficial dermis and bullae. There were no obvious “flame figure”, mucin and vasculitis in dermis. Such a non-specific histopathological picture in connection with clinical features could suggest bullous pemphigoid. However, anti-desmoglein 1 (Dsg1), Dsg3, anti-BP180, anti-BP230 and anti-p200 antibodies were all normal. Direct immunofluorescence (DIF) and indirect immunofluorescence (IIF) tests on rat bladder epithelium were also negative. Based on history, laboratory and histological features, a diagnosis of bullous EAE was made. Then, systemic treatment of prednisolone at 1.0 mg/kg/day and topical therapy with halometasone cream achieved a very good response. Skin lesions improved significantly after 1 week (Figure 1 E). The patient is still being followed up periodically.
EAE usually presents as pruritic annular or arcuate plaques without scales [1, 2]. It predominantly involves the trunk and proximal extremities [3]. Bullae are not a common presenting feature. Histopathologically, the bullae formation is mainly due to prominent papillary dermal oedema, rather than autoimmune reactions. The principal differential diagnoses of EAE are erythema annulare centrifugum (EAC) and Wells’ syndrome (WS). EAC show an infiltrate of histiocytes, lymphocytes, and, rarely, eosinophils with fairly tight aggregate around vessels, known as “coat-sleeve” distribution [4]. In WS, a dense infiltrate of eosinophils damages normal collagen fibres by major basic protein from eosinophils and produces a characteristic histopathological feature termed a “flame figure” [3]. Several reports have described bullae as a skin manifestation of WS, while the absence of flame figures and granulomatous reactions histologically does not imply a diagnosis of typical WS in our case.
Systemic steroids and antimalarials (e.g. hydroxychloroquine) are the standard first-line therapy and most patients have a good clinical response [5]. Other treatments described for classical EAE include hydroxychloroquine, dapsone, thalidomide, ultraviolet B (UVB) phototherapy, dupilumab, or JAKs inhibitor [4, 5].
In summary, we have presented this rare case with such distinctive features in order to strengthen the awareness of such rare eosinophilic dermatosis. This case highlights the importance of an appropriate differential diagnosis, including autoimmune bullous diseases, in EAE presenting with relatively rare cutaneous lesions such as bullae.







