Folliculosebaceous cystic hamartoma (FSCH) is a rare cutaneous hamartoma composed of follicular, sebaceous, and mesenchymal components, and usually occurring on the head and neck [1]. Although giant FSCH has been previously documented, the novel presentation of a giant FSCH is extremely uncommon and easy to misdiagnose with pathologic variants. In this article, we reported a rare case of giant FSCH with unique multiple miliary manifestations and reviewed the literature about trichofolliculoma and sebaceous mantle-associated conditions.
A 45-year-old man presented with a 20-year history of a slowly enlarging plaque on the back of his neck. Since the onset of the disease, the patient had no symptoms. He had no medical history and no family history suggestive of Muir-Torre syndrome or Birt-Hogg-Dubé syndrome. On physical examination, the lesion is approximately 12 cm in diameter and has an unclear margin. The upper part of the lesion has many fused plaques, and the lower part has numerous translucent miliary papules (Figure 1).
Figure 1
Clinical appearance of the patient. There is a large plaque on the back of the neck with small miliary papules

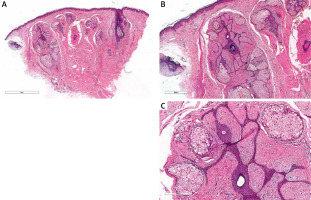
Histopathologic findings of the lesion showed thin cords of epithelial components emanating from several dilated follicular structures (Figure 2 A). The cords of squamous epithelium resembling the infundibular portion of a hair follicle or the epidermis were embedded in a fibrotic stroma with many mature sebaceous glands (Figure 2 B). The surrounding stroma consists of loose connective tissue containing fibrillary collagen, numerous fibrocytes, capillaries, and mucin (Figure 2 C). In addition, we performed magnetic resonance imaging (MRI) of the neck soft tissues to exclude possible infiltration of vascular or nerve branches and there was no involvement. Based on history, clinical features, and histopathological findings, a diagnosis of a giant FSCH was made. We recommended the patient undergo excision and skin grafting but he did not want further treatment. Based upon the benign nature of FSCH, no further intervention is planned. The patient is still being followed up periodically.
Figure 2
Histopathologic findings of the lesion. A – Thin cords of epithelial components emanating from several dilated follicular structures (H&E stains, original magnification ×40). B – The cords of squamous epithelium resembling the infundibular portion of a hair follicle or the epidermis were embedded in a fibrotic stroma with many mature sebaceous glands (H&E stains, original magnification ×100). C – The surrounding stroma consists of loose connective tissue containing fibrillary collagen, numerous fibrocytes, capillaries, and mucin (H&E stains, original magnification ×400)
FSCH is a distinct cutaneous hamartoma formed from epithelial and stromal elements initially described by Kimura et al. in 1991 [2]. The lesions in giant FSCH cases occurred in various sites, such as genital areas, upper extremities, and upper back (Table 1). The clinical features of our case were similar to those of the reported giant FSCH cases, except for the novel miliary surface at the lower part (Table 1). This unique manifestation brought a challenge for clinical diagnosis. Similar to that described by previous literature, the pathology evaluation of our patient showed well-developed hair follicles and the stroma containing groups of mature adipocytes and the cystic structures are surrounded by lobules of sebocytes.
Table 1
Literature review of published case reports of giant folliculosebaceous cystic hamartoma
| Authors, year | Age [years] | Sex | Size [cm] | Duration [years] | Location | Clinical presentation |
|---|---|---|---|---|---|---|
| Tasar et al. [6], 2023 | 84 | Male | 26 × 11 | 62 | Face | A tumorous flesh-coloured, partially erythematous skin lesion |
| Khan et al. [7], 2020 | 29 | Female | 5 × 3 | 3 months | Genital region | A lobulated, non-pedunculated, firm, non-tender plaque |
| Bobde et al. [8], 2019 | 1 | Female | 10 × 8 × 5 | 1 | Posterior thigh | Gradually increasing mass |
| Zheng and Han [9], 2011 | 23 | Male | 13 × 6 × 1.5 | 3 | Right forearm | Multiple, soft, skin-coloured papules and nodules |
| Haw and Lee [10], 2009 | 48 | Female | 10 × 8 × 5 | 20 | Right lower cheek | A pruritic skin-coloured soft tumour |
| Cole et al. [11], 2008 | 9 months | Female | 7 × 3 × 3 | 9 months | Posterior neck | A large, erythematous soft tissue mass |
| Hamada et al. [12], 2006 | 40 | Female | 5 × 3 | 13 | Genital region | Aggregated nodules |
| Sturtz et al. [13], 2004 | 32 | Female | 16.7 × 8.6 × 1.2 | Several | Left upper arm | Multinodular plaque |
| Yamamoto et al. [14], 1994 | 24 | Female | 7.0 × 4.5 × 2.5 | 24 | Back | Lobular appearance |
A variety of differential diagnoses including sebaceous trichofolliculoma, trichofolliculoma with sebaceous differentiation, and fibrofolliculoma should be considered. Perhaps one of the greatest questions surrounding this rare tumour is its potential association with trichofolliculoma [3]. There are numerous authors who believe that trichofolliculoma and FSCH are the same entity. However, we believe that even though these two tumours are not the same entity, they also belong to the same disease spectrum and histologically overlap. Trichofolliculoma has a mature sebaceous gland lobule instead of a secondary follicle. When sebaceous glands are abundant wrapping most of the area around the central cystic structure, it is the sebaceous trichofolliculoma described by Plewig [4]. When there is lipo-metaplasia and significant sebaceous gland differentiation in the stroma, it will overlap with FSCH [1, 3, 4]. In addition, fibrofolliculoma shows similar characteristics to FSCH but usually lacks the sebaceous component of FSCH [5].
Unlike prior descriptions of FSCH, the lesion in our patient showed occasional thin cords of mantle epithelium embedded in a fibrotic stroma and expression of primitive sebaceous differentiation. These features are more like the histopathologic finding of fibrofolliculoma rather than typical FSCH [5]. We speculated that the area resembling the histopathologic features of fibrofolliculoma in our case may be at a differentiated stage between FSCH and fibrofolliculoma.
To the best of our knowledge, this is the second case of giant FSCH in the Chinese population. We presented this rare case with such distinctive features in order to strengthen awareness of this uncommon form of cutaneous hamartoma.








