Introduction
Knee osteoarthritis (KOA) is a common joint condition associated with the aging process, leading to pain, reduced functionality, and disability, significantly impacting the quality of life, and incurring substantial societal and economic costs. Among the elderly population, it stands as the primary cause of disability [1]. Findings derived from comprehensive meta-analyses reveal that the worldwide occurrence of KOA among adults aged 40 years and above is approximately 22.9% (95% confidence interval [CI], 19.8%-26.1%), affecting an estimated 654.1 million people within this specified age demographic on a global scale. The rates of onset of this condition exhibit variations among nations and demonstrate an upward trend with advancing age. The documented occurrence and prevalence proportions for females and males are 1.69 (95% CI, 1.59-18.0, p<0.0001) and 13.9 (95% CI, 1.24-1.56) respectively [2].
The study by Shamekh et al. [3] shows that the prevalence of osteoporosis in the Middle East and North Africa has risen significantly compared with 1990, with an increase of 9.3 percentage points (95% UI 8.1- 10.5%; range, 4,815.9-5,907.8). The reported number of cases has reached 24.6 million (95% UI, 22.0-27.3 million) [2].
The study by Wallace et al. [4] found that men and women of the same age have an equal risk of developing osteoporosis. However, for women, the risk tends to increase notably after the age of 50 [4].
Modern treatment recommendations suggest a combination of medication and non-drug approaches [5], as a means to address KOA effectively [6]. A simple home exercise regimen, focusing on strengthening muscles, increasing the range of motion, and reducing discomfort, has shown beneficial effects for individuals suffering from KOA [7]. However, there is a lack of research on the effectiveness of home-based exercise (HBE) combined with cryotherapy for KOA patients. Therefore, further investigations in this area are warranted.
Cryotherapy, a non-pharmaceutical treatment, has been utilized in certain cases of rheumatic joints [8,9]. Its impact on discomfort, edema, and inflammation has been explored. It can be used as a standalone treatment or as a complement to other therapies [9].
Aim of the work
In light of these methodological challenges, further research is necessary to meet the required standards [9]. Accordingly, the purpose of our present study is to evaluate the impact of an HBE program combined with cryotherapy on the quality of life for individuals with KOA. It is expected that at week 8, both HBE and cryotherapy will have improved patients’ symptomatology, particularly enhancing lower limb muscular strength and gait, owing to their respective effects on KOA.
Material and methods
Study design
Within the framework of this randomized clinical trial, individuals diagnosed with KOA were subject to random allocation into three distinct cohorts. The initial cohort underwent a regimen encompassing both cryotherapy and an HBE protocol over a two-month period. The subsequent cohort exclusively engaged in the HBE program for an equivalent duration. The final cohort, designated as the second control group, received a consistent regimen of physiotherapeutic interventions and therapeutic care within the designated medical facility.
Comprehensive elucidation regarding the potential hazards attributed to KOA, as outlined in accordance with the established protocols of the institution, was disseminated to all participants across the three groups. The comprehensive medical and clinical assessments of these individuals were conducted at the Specialized Center of Rheumatic Pathologies and Medical Rehabilitation. After the diagnosis of KOA by a rheumatologist from the collaborative center, patients were deemed suitable for subsequent scrutiny. Following this preliminary validation, these individuals were subsequently referred by the rheumatologist to the researcher for an in-depth evaluation.
The investigators evaluated the potential eligibility of candidates through the examination of parameters such as body mass index (BMI) and other pertinent variables. Patients who fulfilled the stipulated prerequisites for subsequent scrutiny provided written consent for participation and were subsequently subjected to a random allocation process, thereby being assigned to either the experimental, control, or second control cohort. Further details regarding this process are available in Figure 1 through the flow chart provided.
From August 1st, 2021 to June 1st, 2022, the recruitment of participants was undertaken at the Specialized Center of Rheumatic Pathologies and Medical Rehabilitation situated within Duhok City, Iraqi Kurdistan. The intervention phase for the patients extended over a duration of two months, followed by an additional month designated for post-interventional follow-up.
Setting, participation, and sampling
The Specialist Center of Rheumatic & Medical Rehabilitation located in Duhok, Kurdistan, Iraq, served as the primary source of patients for this study. This center offers comprehensive diagnostic, therapeutic, and rehabilitative care for individuals with rheumatic illnesses, making it a unique facility for such conditions. Before enrolling patients, the researcher collected demographic data about the study participants. The medical staff at the center provided essential information, including gender, age, BMI, illness severity, and level of education, to ensure a diverse and representative sample for analysis. The study population exhibited variations in sex, age, BMI, level of education, and illness severity.
To achieve a representative sample, a data collection period of six months was chosen. During this period, the researcher dedicated two days a week to being at the facility, collaborating with doctors to conduct the investigation effectively. To ensure more comprehensive inclusiveness of local patients, the study participants were sourced from a diverse array of local healthcare providers. To enhance precision regarding diagnostic accuracy, the researchers conducted a thorough scrutiny of the patients’ medical and clinical records. Following the confirmation of eligibility, a random numerical assignment ranging from 1 to 3 was allocated to each qualifying patient, determining their placement within one of the three distinct groups.
For this purpose, the aggregate patient count was recorded in Statistical Software for Social Sciences 25 (SPSS 25), generating a predetermined three-tiered numeric allocation. This meticulous procedure resulted in the segregation of patients into three discreet subsets, devoid of any explicit designations, thereby mitigating potential biases. The subsequent nomenclature for the groups was then assigned in an entirely random sequence, aimed at upholding impartiality.
It should be emphasized that the medical practitioners affiliated with the center had no involvement in the implementation of study interventions or the evaluation of outcomes. In addition, these clinicians remained entirely uninformed about the specific group assignments of their respective patients, thereby further ensuring the study’s objectivity.
To prevent allocation bias, all patients were from different parts of Duhok province. Interestingly, there were two related patients, and the initial case was included in the final analysis while the second case, despite receiving identical treatment, was excluded from the analysis. Moreover, the control group was not informed about the use of cryotherapy to prevent any potential bias.
For the intervention, written consent was obtained from the patients. The researcher conducted follow- up interviews at the patients’ homes once a week, ensuring continuous monitoring of the intervention’s progress.
Sample size
To determine the sample size for the study, the researchers considered the expected positive effects of cryotherapy on KOA patients’ outcomes. They utilized previous research to establish typical values for KOA patients. The size of the sample was then determined by analyzing the impact of cryotherapy and at-home exercise on the functionality of individuals with KOA. With a Cohen’s d effect size of 1.39, the researchers anticipated that the mean value would increase from 6.85 (with a standard deviation of 1.57) to 1.57 (with a standard deviation of 1.67) in this scenario.
To achieve sufficient statistical significance, a minimum of 15 participants was needed in each group. The results, using a two-tailed test, with a 0.05 probability of possible mistakes, and an allocation ratio of 1 (N2/ N1), was determined to be 0.9562. G*Power 3.1.9 was employed to calculate the sample size.
Eligibility criteria
In order to meet the prerequisites for the participation in the research, prospective candidates were required to fulfill the following specific criteria for inclusion: a) presentation of a KOA diagnosis at a grade not surpassing 3, b) manifestation of prevailing joint symptoms, c) age bracket ranging from 40 to 60 years, d) indication of knee pain occurring on the majority of days within the preceding month, e) demonstration of an average knee pain rating between 3 and 7 on the visual analog pain scale over the most recent week, and f) maintenance of a BMI) below 40.
Exclusion criteria
Individuals meeting any of subsequent exclusion criteria were ineligible for participation in the study: presence of rheumatoid arthritis or other systemic rheumatic ailments, b) manifestation of dementia, psychosis, or an active substance abuse disorder, c) history of acute or chronic ailments, injuries, deformities, or prior surgical interventions affecting the lower extremity or knee, d) experiencing pronounced hearing or visual impairment, e) recent hospitalization due to cardiovascular ailment, cerebral infarction, or arrhythmia within the preceding three months, f) occurrence of three or more recent falls, g) concurrent engagement in an alternate intervention study targeting osteoarthritis (OA), h) existence of uncontrolled diabetes mellitus, receipt of intra-articular knee injections in the immediate six-month period prior to the study, and j) possessing contraindications to the application of cryotherapy, such as experiencing heightened discomfort or pain during its administration.
Everyone fulfilling the established criteria for eligibility provided written informed consent prior to participation, and the author conducted the evaluations. Patients failing to meet the stipulated eligibility standards were deliberately excluded from numerical allocation to preempt any potential introduction of bias. After these preliminary procedures, the assessment of outcomes commenced.
Once the designated time frame elapsed, the study’s outcomes were carefully recorded and organized. The primary author administered a combination of interventions to the patients, assisted by a nurse physiotherapist. To ensure impartiality and minimize bias, a skilled nurse, trained in the relevant measures for determining success, was responsible for data collection. To maintain the integrity of the research, a registered nurse with a bachelor’s degree was instructed by the researchers to keep score for both groups. Importantly, the identity of this nurse remained concealed during the patient assignment to the respective research groups. The skilled nurse, who was unaware of the patients’ group assignments, conducted both the baseline and follow-up measurements. This approach was taken to ensure the accuracy and objectivity of the collected data.
Pilot study
The initial phase of the research involved a small pilot study with only five participants. These individuals were the first five identified with KOA, and they were assigned therapies based on pre-generated random numbers. The main objective of this pilot study was to explore potential challenges and areas requiring further investigation for a more extensive research project. The researchers were uncertain whether the study could be successfully conducted. Fortunately, no significant issues were encountered during the pilot study, allowing the researchers to proceed with their work confidently.
Interventions
Experimental and control 1 group
In the initial session of the intervention group’s treatment, patients were educated about the risks associated with KOA. To minimize disruptions for other patients at the facility, these individuals received personalized information about KOA risk factors in the comfort of their own homes. Additionally, during the first session, patients were introduced to HBE and were guided by the first researcher in carrying out the HBE intervention as outlined in the manual. To ensure proper understanding, the patients were provided with a video demonstration and a pamphlet (translated into Kurdish and Arabic), detailing the correct way to perform the exercises.
To maintain adherence and reduce the chance of patients being lost to follow-up, a weekly follow-up visit was conducted by the researcher to ensure that the patients were performing the exercises correctly. For the remainder of the HBE routines, patients carried out the exercises independently. In addition to HBE, cryotherapy was recommended by the researcher and administered to the patients for a total of two months, followed by a one-month follow-up period.
The investigation extended over a period of 8 weeks, during which the investigator conducted home visits at intervals of weeks 1, 3, 5, and 7. These scheduled visits were strategically organized to mitigate attrition rates and optimize adherence to the prescribed exercise regimen. In the inaugural consultation, patients were provided with health guidance spanning thirty minutes. Subsequent sessions encompassed a total duration of 80 minutes, with approximately 70 to 75 minutes devoted to the exercise protocol and an additional 20 minutes allocated to the application of cryotherapy.
To sustain consistent communication and offer motivational support, the researcher engaged in telephone conversations with the participants at the intervals of weeks 2, 4, and 6. These interactions were aimed at tracking their advancement and fostering dedication to the prescribed regimen of home-based exercise and cryotherapy.
Throughout the 8-week study period, there were a total of 24 sessions, with each week featuring three separate meetings conducted on different days.
The educational program designed for individuals afflicted with KOA and their familial associates facilitated in-depth dialogues encompassing clinical manifestations, predisposing factors, nursing strategies, exercise advantages, and the merits of cryotherapy. Comprehensive insights into the HBE intervention and cryotherapy can be gleaned from the details presented in Figure 2. In the context of cryotherapy, the patients’ knees were subjected to treatment involving two gel ice packs of reusable nature (measuring 48×15×0.5 cm), each applied for a duration of 20 minutes. These packs were positioned to envelop the anterior, posterior, medial, and lateral aspects of the knee.
Control 1 participants were subjected to an identical educational curriculum and HBE intervention, mirroring that of the experimental group. Nevertheless, the administration of cryotherapy was omitted for this subgroup. Much like the experimental cohort, vigilant monitoring of these patients’ advancement was diligently conducted, as described in the supplementary documentation.
Control 2 group
During the initial session, these patients received health education regarding the risks associated with KOA. As there was no specific intervention involving home visits, the researcher did not make house visits to these patients. However, researchers maintained regular communication with them through phone calls to monitor their progress and ensure their adherence to the prescribed treatment plans.
These patients participated in routine physical therapy and education sessions at a specialized center dedicated to the treatment of rheumatic and medical conditions. During these sessions, they engaged in various exercises, including hip and knee flexion, short arc quad, straight leg raises, and long arc quad. These exercises were further detailed and described in-depth for the patients’ understanding and implementation.
Step 1: Hip and knee flexion:
Lying straight on your back, bend your knee and hip.
Your kneecaps must point toward the ceiling.
Hold your knee in the position for five seconds, then return to the start position.
Step 2: Short arc quad
Place a firm roll or a rolled towel under your knee.
Straighten the knee to lift your foot off the bed.
Hold it in this position for five seconds. Slowly lower the foot down to the bed.
Step 3: Straight leg raise
Lie on your back and put one leg in a comfortable position.
Slowly raise the other painful leg, keeping the knee straight.
Hold the knee in this position for five seconds and slowly lower your leg.
Step 4: Long arc quad
Assessment of outcomes
A standardized survey instrument was employed to systematically gather and document comprehensive demographic particulars and the medical background of the patients. This encompassed essential facets such as age, gender, stature, BMI, marital status, educational attainment, profession, smoking habits, frequency of falls within the preceding year, count of impacted knees, injury grading, utilization of analgesics and cartilage medications, in addition to concurrent comorbid conditions.
Primary outcome measures
The primary emphasis of this investigation revolved around the examination of three key endpoints: the severity of pain, the 5TSTS as proposed by Fudickar et al. [10], serving as an assessment tool for appraising functional strength of the lower extremities, transitional movements, balance, and susceptibility to falls, as well as the therapist instructions paradigm. During the therapist instructions, the patient was positioned in a seated stance with their back supported by the chair’s backrest. The therapist offered reassurance and audibly enumerated the repetitions of rising movements. The evaluation concluded upon the successful completion of the fifth standing action by the patient.
Secondary outcome measures
The secondary outcome of the study was assessed using the 4x10-meter fast-paced walk test [11]. This test measures a crucial ability often affected in individuals with hip problems and/or KOA: the capacity to walk quickly over short distances.
Statistical methods
Patient demographic information within the three groups was presented through the utilization of mean values accompanied by their corresponding standard deviations (SD) and proportions depicted as numbers and percentages (%). To facilitate a comparative analysis of the foundational characteristics of KOA patients across the distinct study groups, either ANOVA one-way tests or Pearson chi-squared tests were employed, as appropriate.
Furthermore, to juxtapose the results of the 5TSTS and the 4x10-meter brisk walk assessment among KOA-afflicted patients within the study groups, ANOVA one-way analyses were carried out. After this, post hoc comparisons were executed utilizing the Tukey test to discern specific inter-group differentials. Notably, disparities attaining a threshold of statistical significance, characterized by a p-value of less than 0.05, were duly acknowledged. The suite of statistical computations was executed utilizing JMP pro-14.3.0, facilitating a rigorous analytical framework.
Results
Upon reaching the intention-to-treat phase, an examination of the baseline data concerning participants within both the experimental and control cohorts revealed a marked degree of resemblance. To fortify the validity of the randomization process, a meticulous assessment of the comparability between lost-to-follow- up patients and the designated study groups was conducted in terms of baseline and medical attributes. Notably, an observation emerged, indicating that patients within the control, experimental, and lost-to-follow- up subsets exhibited noteworthy parallels with regards to their overarching general and medical particulars. A more detailed depiction of this alignment is available in Table 1, accentuating the confluence of analogous general and medical attributes among the encompassed study cohorts.
Table 1
Comparisons of general after removing lost-to-follow-up
At baseline, the participants in the control and experimental groups exhibited similarities in various factors, including fall history (92.86, 100, and 100; p=0.2893), affected knees (64.29, 92.33, and 70.59; p=0.5114), grade (85.17, 76.47, and 70.59; p=0.6078), as well as analgesics, cartilage drug, comorbidity, and disease duration. Additionally, there was comparable similarity among participants in the Pain Visual Analog Scale (VAS) (0.68, 1.00, and 1.03; p=0.0624), the 5TSTS (4.26, 4.02, and 2.78; p=0.3794), and the 40-meter fast-paced walk test (6.84, 5.08, and 6.20; p=0.0587), as presented in Table 2.
Table 2
Comparisons of medical and baseline outcomes at the intention to analysis step
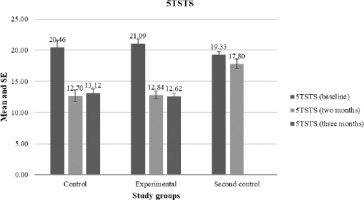
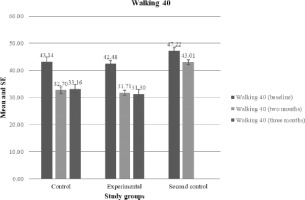
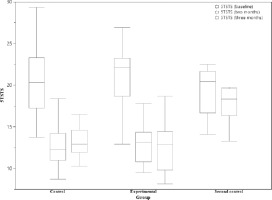
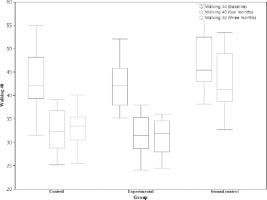
Upon reaching the two-month juncture, both the control and experimental cohorts exhibited markedly reduced scores in the 5TSTS relative to the second control group, recording scores of 12.70, 12.84, and 17.80, respectively, a discrepancy that proved to be of pronounced statistical significance (p<0.0001). Analogously, in the 4x10-meter, the control and experimental groups likewise attained notably diminished scores in comparison with the second control group, registering scores of 32.70, 31.71, and 43.01, respectively, with the observed disparities being characterized by substantial statistical significance (p<0.0001).
Upon reaching the three-month milestone, the control group displayed marginally enhanced scores in both the 5TSTS and 4x10-meter evaluations in relation to the experimental group, denoting scores of 13.12 compared with 12.62 (p=0.5959) and 33.16 compared to 31.30 (p=0.1913), respectively. It is noteworthy, however, that these discrepancies failed to attain statistical significance, a depiction that is further explained in Table 3 and Figures 2-5.
Table 3
Comparisons of outcomes among study groups at two and three months
Within the confines of the control group, noteworthy reductions were observed in the 5TSTS score, signifying a substantial decline from the baseline measurement to the two-month juncture (20.46 to 12.70), and subsequently to the three-month interval (13.12). Analogously, the 4x10-meter score underwent a significant decrease, progressing from the baseline value to the two-month time point (43.14 to 32.70), and extending to the three-month evaluation (33.16).
Correspondingly, within the experimental group, analogous patterns of decline were manifest in the 5TSTS score, demonstrating significant reductions from the baseline measure to both the two-month (21.09 to 12.84) and three-month marks (12.62). Notably, the Walking 40 meters score exhibited similar dynamics, registering substantial diminution from the baseline to the two-month assessment (42.48 to 31.71), and persisting through the three-month appraisal (12.62).
Conversely, discernable variations were absent in the second control group, where neither the 5TSTS nor 4x10-meter scores exhibited statistically significant changes over the course of two and three months, as outlined in Table 4.
Table 4
Comparisons of outcome between pre and posttest in each study group
Discussion
This is the initial study we are aware of, that compares the effectiveness of HBE and cryotherapy in aiding patients with KOA to enhance their functional capabilities. Patients who received both HBE and cryotherapy showed significantly greater improvements in lower-limb muscle strength and walking ability at two and three months compared with those who only received HBE or no intervention at all.
As far as our current understanding extends, there exists no previous investigation examining the efficacy of amalgamating HBE with cryotherapy to enhance functional capacity among individuals afflicted by KOA. Nonetheless, it is evident that cryotherapy constitutes a principal outcome arising from this amalgamation. Recognizing the imprudence of withholding physiotherapeutic interventions from patients, the decision was taken to integrate cryotherapy within the ambit of the HBE intervention.
In the context of a RCT by Dantas et al. [12], encompassing a cohort of sixty individuals diagnosed with KOA, an appraisal was undertaken to assess the efficacy of cryotherapy. Strikingly, within this cohort, a subset of 30 patients underwent cryotherapy intervention, which entailed the application of ice packs consisting of crushed ice contained within two plastic pouches (measuring 24 x 3 x 34 x 0.08 cm), each weighing one kilogram, to the afflicted knee joint. These ice packs were administered with gentle compression across the medial, posterior, and lateral facets of the knee for a duration of 20 minutes, once daily, and sustained over a period of four consecutive days [12]. In contrast, the remaining study participants were designated to the sham group, where sand-filled packs were utilized as a substitute for the crushed ice packs. Intriguingly, both the cryotherapy recipients and those in the sham group reported comparable levels of discomfort after their respective interventions [12]. Notably, despite this observation, the affirmative impacts of cryotherapy on functional capacity and quality of life were acknowledged and underscored [13].
Cryotherapy was omitted from the final recommendations of the Ottawa Panel, the European League Against Rheumatism, and the International Osteoarthritis Research Society, as a result of the expert panel’s inability to achieve a consensus regarding its efficacy [13,14]. Their conjecture was that cryotherapy could potentially lack advantageous effects KOA. Nonetheless, it is noteworthy that both the American College of Rheumatology and the National Institute for Health and Care Excellence have provisionally advocated cryotherapy as an adjunctive therapeutic avenue for individuals grappling with KOA [15].
A clinical inquiry was executed with the intent of comparing the efficacy of exercise, cryotherapy, and short waves as therapeutic interventions for grade I KOA. The study by Silva et al. [16] encompassed a cohort of 25 participants, aged between 58 and 78 years. In Group A, a combination of 20-minute exercise sessions and short waves was administered, whereas Group B underwent 20-minute cryotherapy sessions. Group C engaged in dedicated exercise regimens. All participants partook in ten physical therapy sessions per week, twice weekly, at an outpatient facility. These sessions encompassed the execution of isometric exercises targeting a spectrum of muscle groups including the hip abductors, sural triceps, adductors, ischiotibial, and quadriceps. Supplementary to this, ergometric bicycle exercises and proprioception exercises involving cushions were undertaken. In certain instances, short waves or ice applications were additionally employed [16]. The study outcomes indicated that the combined utilization of ice and kinesiotherapy emerged as the best strategy for pain management. Furthermore, exclusive application of kinesiotherapy yielded limited pain relief effects, albeit resulting in favorable outcomes concerning functional competence, muscle strength, and range of motion [16].
In a separate investigation by Deyle et al. [17], a RCT was undertaken to juxtapose the efficacy of two distinct therapeutic approaches for KOA: the amalgamation of manual treatment with cryotherapy versus the implementation of kinesiotherapy in conjunction with cryotherapy. The cohort allocated to the intervention group (n=64) received a combination of both cryotherapy and manual treatment. Cryotherapy was executed through the application of a cold nitrogen vapor set at a temperature of 130°C, directed towards the knee joint. The administration necessitated that the machine nozzle maintains a distance not exceeding 10 cm from the patient’s skin, with the cryotherapy session’s duration confined to a span of 3 minutes. The manual treatment modalities encompassed tibiofemoral distraction, anteroposterior tibial gliding, medial and lateral tibial rotation, as well as patellar gliding [17]. The sessions were conducted within an approximate time frame of 45 minutes at maximum. The control group was subjected to kinesiotherapy, comprising a five- minute preparatory warm-up, a five-minute segment of stretching exercises, a fifteen-minute session of muscular strength training, an interval of five minutes of stationary cycling, culminating with five minutes of cryotherapy application (referred to as the KIN-C group) [17].
The study by Lizis et al. [18] demonstrated that in comparison with the kinesiotherapy merged with the cryotherapy approach, the amalgamation of manual therapy alongside cryotherapy elicited more pronounced reductions in pain, improvements in quality of life, augmentation of range of motion, and enhancements in functional exercise capacity. While we acknowledge the potential advantages associated with cryotherapy, our perspective diverges in terms of its suitability as a principal strategy for averting subsequent injuries. The direct impact of ice extends to the tendinous structure and muscular spindle, and the possibility of inducing overexertion post-muscle cooling raises concerns regarding the heightened sensitivity of the motor control threshold, potentially culminating in fresh muscle injuries. Consequently, we are inclined to disfavor its adoption as the foremost measure to counteract further injuries [19].
A systematic review of three RCTs by Brosseau et al. [20], analyzed various aspects, such as the methodology employed, the variables measured, the application of heat or cold, and the rigor of result verification. One of the experiments evaluated the effectiveness of ice massage compared with a control group. Following two weeks of daily 20-minute ice massages, five days a week, a statistically significant improvement in quadriceps strength was observed, with a 29% point relative difference compared with the control group [21].
In an additional study by Clarke et al. [22], encompassed within the systematic review, an investigation was conducted to contrast the impact of ice pack application on pain relative to a control group. Both the ice pack therapy and the placebo intervention were administered thrice weekly, although the precise duration of the placebo treatment remained unspecified. Following three weeks of intervention, the ice pack group demonstrated a marginally noteworthy enhancement in comparison with the control cohort, with the effect size nearly attaining statistical significance (Weighted Mean Difference [WMD] = -2.70, 95% Confidence Interval [CI]: -5.52 to 0.12; p=0.06). Nevertheless, subsequent to a follow-up interval of three months, no notable disparities in pain levels were observed between the control and ice pack cohorts [22].
The third study in question by Hecht et al. [23] investigated the efficacy of both hot and cold packs relative to a placebo intervention. In this investigation, participants were subjected to either thermal therapy involving the application of heat or cold to both the anterior and posterior regions of the affected knee. This therapeutic regimen encompassed a sequence of ten successive sessions, each lasting 20 minutes. The findings of the study unveiled a statistically notable amelioration in knee edema, substantiated by a reduction in knee circumference after the completion of ten sessions of cold therapy (p=0.04). However, contrasting outcomes emerged for the hot pack group, where no statistically significant divergence was observed when compared with the control group [23].
According to the comprehensive review by Lizis et al. [18], the application of ice massage exhibited substantial enhancements in knee strength, range of motion, and functional performance, displaying superiority over the control group. The outcomes indicate that cold packs offer greater effectiveness in mitigating knee swelling in contrast with both hot packs and placebo interventions. Nevertheless, the influence of hot packs on edema was found to be inconsequential when juxtaposed with cold packs or placebo treatments. Furthermore, in the context of patients afflicted with KOA compared with a control group, the utilization of ice packs with compression did not yield discernible relief from pain [18].
To further investigate the multifaceted advantages of cryotherapy, our inquiry encompassed hydrotherapy combined with balneotherapy and HBE. This intervention was rooted in a quasi-experimental study examining the impact of HBE on 141 individuals aged 60 and above, all diagnosed with KOA. The framework for HBE was tailored based on insights found in the data and the outcomes of the aforementioned antecedent study by Lizis et al. [18]. Both the comparison group and the experimental group received different treatments. The comparison group received health education for a duration of 12 months, while the experimental group received hydrotherapy with balneotherapy and HBE in addition to health education. McMaster University utilized a questionnaire to evaluate various outcomes, including the severity of KOA-related pain and joint stiffness in both groups [24]. Pain levels decreased from an initial value of 7.34 (with a standard deviation of 3.36), and joint stiffness reduced from 2 (with a standard deviation of 0.3) to 1 (with a standard deviation of 0.3). Furthermore, lower limb muscle strength increased from 14.22 (with a standard deviation of 3.10) to 12.13 (with a standard deviation of 2.93), balance improved from 13.30 (with a standard deviation of 3.14) to 11.73 (with a standard deviation of 1.97), mobility increased from 408.45 (with a standard deviation of 60.54) to 442.39 (with a standard deviation of 49.70), and overall quality of life improved.
Our observations aligned with the results of a preceding investigation by Xie et al. [24] that similarly revealed a noteworthy enhancement in lower-limb muscle strength and walking capability within the treated cohorts through the amalgamation of HBE and cryotherapy, when contrasted against the control group.
However, after a two-month interval of commencing the treatment regimen, recipients of both cryotherapy and HBE did not exhibit any substantial improvements in comparison with those allocated to the control 1 group. Additionally, at the conclusion of a one-month period following the cessation of interventions, no marked distinctions emerged between the group subjected to the intervention and the control 1 group.
Cryotherapy has the potential to alleviate pain and inflammation while also slowing down local metabolism, leading to reduced cellular energy demands and a decreased risk of additional tissue damage caused by hypoxia [25]. Cold treatment induces vasoconstriction and hinders significant increases in microvascular permeability, which could potentially reduce the filtration of fluid into the interstitial region [26]. The findings of this investigation propose that cryotherapy has potential for alleviating pain, reducing edema, and mitigating inflammation in patients afflicted by KOA. Moreover, there is an indication that the synergistic incorporation of cryotherapy with manual treatment or kinesiotherapy might yield supplementary advantages for individuals grappling with KOA [27,28]. In an experimental rat model simulating post-traumatic KOA, the application of cryotherapy appears to exhibit a capacity for diminishing synovial inflammation. This effect is achieved through the modulation of inflammatory cytokine levels and the attenuation of leukocyte migration into the knee joint cavity [29].
Strengths and limitations of the study
We endeavored to fully encompass a representative cross-section of the population within the scope of this study. To this end, we procured comprehensive general and medical data from select patients diagnosed with KOA prior to their participation and engagement in the interventions. Furthermore, we meticulously executed a randomized allocation process, exerting concerted efforts to curtail the instances of attrition among participants, while rigorously adhering to the established criteria for inclusion and exclusion. This deliberate approach facilitated the exclusion of individuals potentially influencing pain and functional outcomes. However, it is imperative to acknowledge that the study bore certain limitations, notably the exclusion of patients with higher BMI. Nonetheless, the present findings may still hold relevance for individuals with elevated BMI, thereby extending the potential applicability of the observed effects to this subgroup; no group comparison was performed after 3 months.
Future attempts
The authors proposed the utilization of crushed ice in lieu of commercially available gel for individuals afflicted with KOA, aiming to enhance the impact of cryotherapy. Additionally, the researchers advocate for the assessment of cryotherapy’s effects at the intervals of three and six months after the intervention.
Conclusions
In summary, the outcomes derived from this investigation manifest a marked enhancement in the domain of lower-limb muscle strength and walking capacity through the utilization of a synergistic approach involving HBE and cryotherapy modalities, in contrast with the cohort designated as control 2. Nonetheless, it is worth noting that no discernible impact was found concerning the augmentation of lower-limb muscle strength and walking ability when the confluence of HBE and cryotherapy techniques was juxtaposed against the control 1 group within the context of individuals grappling with KOA.