INTRODUCTION
Lichen planopilaris (LPP) is a chronic form of scarring alopecia that manifests through follicular hyperkeratosis, perifollicular erythema, and the loss of follicular orifices [1]. It is classified as a variant of lichen planus, which involves perifollicular inflammation and eventual destruction of hair follicles, followed by their replacement with scar tissue. Although the aetiology of LPP remains unclear, its association with autoimmune dysregulation is strongly suggested, with some evidence pointing toward a T-cell-mediated inflammatory mechanism directed against follicular antigens [2].
Treating LPP is challenging due to its progressive nature. Most treatments are primarily aimed at halting inflammation and preventing further hair loss. They include the use of corticosteroids, systemic immunosuppressants like hydroxychloroquine and calcineurin inhibitors [3]. Despite attempts to control the inflammatory process, long-term remission still remains difficult to achieve, and it is not uncommon for relapses to occur [4].
Follicular unit excision (FUE) is considered a possible method for hair restoration in patients with stabilized scarring alopecia [5]. FUE involves extracting individual follicular units from the donor area, typically in the occipital region of the head and then implanting them into areas affected by alopecia [6]. However, hair transplantation in LPP patients is only feasible when the disease has been inactive for a significant period of time – usually 12 to 24 months. Reactivation of LPP following hair transplantation is a well-recognized risk, with recurrence rates varying depending on the duration of LPP remission before surgery [7].
OBJECTIVE
The discussed report is based on the case of a patient treated in our clinical practice. Its goal is to highlight the potential use of hair transplantation in the treatment of hair loss associated with lichen planopilaris.
CASE REPORT
A 36-year-old male patient was admitted to our clinic complaining of hair loss in the occipital part of the scalp formed as a result of lichen planopilaris. The area of hair loss on the day of admission had an approximate diameter of 3 cm. The primary disease had been diagnosed 6 years prior to the patient’s first visit to our clinic. Since then, the patient had undergone three local flap repairs aimed at reducing the size of the area lacking hair follicles. The last of these procedures was performed a year before admission. Apart from that, the patient had no chronic diseases.
The area of hair loss was assessed by a physician from our team as soft, and therefore, the patient was qualified to undergo a hair transplantation procedure, specifically FUE.
The FUE procedure was performed under local anaesthesia using a 1% lidocaine solution applied to the margins of the treated areas, along with tumescent local anaesthesia comprising bupivacaine, sodium bicarbonate, and adrenaline solution. Initially, 300 grafts composed of follicular units were retrieved from the unaffected occipital region of the scalp. For this purpose, DeVroye’s WAW FUE system, together with the Hybrid Tornado punch and a Nouvag handpiece, was used. The implantation process was distributed evenly across the donor area to avoid a visible decrease in hair density.
Subsequently, after the administration of anaesthetic fluids to the recipient area, the grafts were implanted using Lion Implanter Pens following the creation of incisions with a sapphire blade. Upon completion of the implantation process, the entire treated area was thoroughly cleaned using a 0.9% sodium chloride solution, a compression bandage was applied to the donor site, and the patient was discharged from the clinic.
The convalescence period lasted one month, during which the patient was instructed to wash his hair using a provided shampoo containing bovine colostrum and to avoid physical exercise and intense sun exposure.
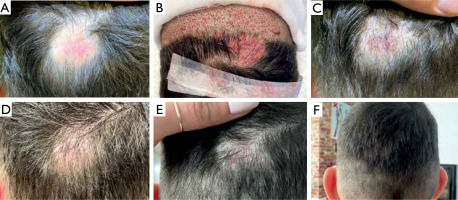
The schedule for follow-up appointments included visits at 1 month, 6 months, and 1 year after the procedure (fig. 1). We observed typical changes in the density of the implanted grafts over time following the FUE procedure – a decline after the first month, followed by regrowth in the subsequent months. The outcome of the FUE procedure was evaluated by both the patient and the operating physician as satisfactory. A follow-up was carried out 2 years after the procedure, and no decrease in hair follicle density in the treated area was observed.
DISCUSSION
The course of the hair transplantation procedure did not pose any major technical differences compared to a standard FUE procedure performed in cases of androgenetic alopecia. The post-operative sequence involving the loss and subsequent regrowth of the implanted hair follicles also did not show any significant deviations. The satisfactory effect achieved in the reported case suggests the potential use of hair transplantation in the treatment of hair loss in lichen planopilaris.
Although such reports remain limited, similar effects have been observed. In a systematic review conducted by Lee et al., out of five different studies, 8 patients with lichen planopilaris who had undergone hair transplantation were assessed. In that study it was found that 75% of the patients experienced positive results. The graft survival rate in a long-term follow-up (> 12 months) ranged from 70% to 95% [8]. Such rates do not seem to significantly differ from standard procedures performed in androgenetic alopecia patients [9].
An important factor considered to play a role in the delivery of positive outcomes of hair transplantation procedures performed in lichen planopilaris is the duration of disease remission prior to the surgical procedure. Since mechanical trauma, such as that associated with hair transplantation, can promote the formation of new scarring areas in unstable forms of cicatricial alopecia, a recommended remission period of 1 to 2 years prior to surgery has been proposed [10].
Another important issue to address is the possible adverse, negative effect of hair transplantation in the treatment of primary scarring alopecia. In a systematic review published by Ekelem et al., patients with cicatricial alopecia who had undergone hair transplantation procedures were studied. While the majority of assessed patients experienced moderate to positive outcomes, 8 out of 34 patients experienced negative results or disease recurrence [11].
A possible role of surgical treatment in disease activation has been shown in studies assessing the development of lichen planopilaris following hair transplantation. In a study by Donovan, 17 patients who were initially presumed to have androgenetic alopecia underwent hair transplantation procedures and subsequently developed lichen planopilaris. The final diagnosis was confirmed by biopsies [12]. However, it remains debatable whether these patients, despite being clinically diagnosed with androgenetic alopecia, may have had undiagnosed cicatricial alopecia that was activated by the transplant procedure.
Hair transplantation procedures, like FUE, seem to have a great potential in the treatment of hair loss in patients with lichen planopilaris. However, the limited data supporting this approach requires more extensive research involving a larger number of patients. Given the possible adverse effects and the risk of lichen planopilaris activation due to mechanical trauma during the procedure, long-term follow-up and careful patient monitoring are essential.