Primary infection with varicella zoster virus (VZV) can cause varicella which principally occurs during early childhood. Then, followed by life-long residence of the VZV genome in the dorsal-root or cranial-nerve ganglia. Viral reactivation later in life can result in herpes zoster. In clinical practice, concurrent herpes zoster and chickenpox in middle-aged and old adults have seldom been reported, these rare cases usually occur in kidney transplantation, human immunodeficiency virus infection, and other immune dysfunction. However, antiviral treatment with acyclovir in a patient with renal failure was controversial. Here, we report the case of successful treatment of concurrent herpes zoster and chickenpox with brivudine.
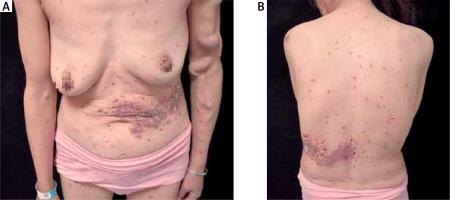
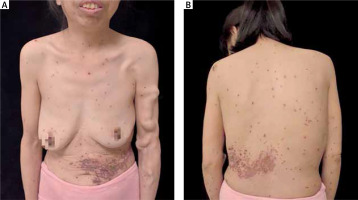
Here, we record a 47-year-old Chinese female who was affected by blisters on her left abdomen and back, accompanied by pain for 20 days and generalized symptoms for 5 days. This patient underwent a kidney transplant surgery in 2019. Moreover, she was taking oral tacrolimus 2.5 mg in the morning and 2 mg in the evening, mycophenolate mofetil 0.5 g twice daily, febuxostat tablet 20 mg at night, prednisone 5 mg once daily. She denied having a history of hepatitis, tuberculosis, diabetes, and hypertension. Physical examination discovered red macules and papules scattered throughout the body, with varying sizes and well-defined boundaries. Transparent blisters with cloudy blister fluid are occasionally observed on the skin. Those blisters were identified as varicella. Red patches were distributed in strips on the left abdomen and waist, covered with brown scabs (Figure 1), extending beyond the body’s midline. These symptoms were considered as herpes zoster. Laboratory investigation: white blood cell count was 1.85 × 109/l (normal range: 3.5–9.5 × 109/l), red blood cell count was 1.53 × 1012/l (normal range: 3.8–5.1 × 1012/l), haemoglobin level was 62 g/l (normal range: 115–150 g/l), platelet count was 115 × 109/l (normal range: 125–350 × 109/l), lymphocyte absolute value was 0.26 × 109/l (normal range: 1.1-3.2 × 109/l), lymphocyte percentage was 13.8% (normal range: 20–50%), neutrophil absolute value was 1.34 × 109/l (normal range: 1.8–6.3 × 109/l), blood sedimentation rate was 85 mm/h, serum amyloid protein (SAA) was 122.4 mg/l, C-reactive protein was 19.34 mg/l, and ferritin was 248 µg/l (13–150 µg/l). The urinary routine tests showed occult blood+ and a urine specific gravity of 1.007. The stool routine occult blood test was positive for OB+; blood creatinine level was 188.1 µmol/l (normal range: 41–73 µmol/l), urea was 15.15 mmol/l (normal range: 2.6–7.5 µmol/l), D-dimer level was 0.88 mg/l. The immunoglobulin G level was 7.27 g/l (normal range: 7.51–15.6 g/l), complement C3 level was 0.67 g/l (normal range: 0.79–1.52 g/l), and complement C4 level was 0.14 g/l (normal range: 0.16–0.38 g/l). Procalcitonin, three aspects of thyroid function, immunoglobulin IgE, preoperative 4, antinuclear antibodies, cytokine 14, and electrocardiogram showed no significant abnormalities. Chest computed tomography (CT) showed viral pneumonia, with the lesion slightly absorbed compared to before. Due to renal failure, the patient received oral brivudine tablets of 125 mg/day for 1 week. Primary control of the lesions was obtained over the course of 1 week with this therapeutic agent. The erythema progressively darkened, the blisters gradually dried, partially crusted and scattered pigmentation as shown in Figure 2. The dermatitis showed significant progress toward resolution, and the symptoms of pain have been completely relieved.
VZV is a naturally occurring human herpes virus that causes chickenpox and herpes zoster. Chickenpox is caused by primary VZV infection. It is a common childhood disease that can cause fever and systemic rash after infection. VZV has a certain incubation period in the dorsal root ganglion cells of the spinal cord after the initial infection. Herpes zoster (HZ) is caused by the reactivation of VZV. It is a local, painful blister disease that can affect the skin of one or the corresponding ganglion. The incidence rate of herpes zoster increases with age or immunosuppression. Although most cases of herpes zoster occur in patients with normal immune function, immunosuppressed patients are 20 to 100 times more likely to have herpes zoster than their peers with normal immune function [1]. Chickenpox is more common in children, while herpes zoster is more common in adults. Both diseases can coincide in patients with a state of immune dysfunction [2].
Herpes zoster can be diagnosed clinically based on symptoms such as erythema, blisters, and herpetic neuralgia related to the distribution of skin ganglia on one side of the body. When the rash is atypical, diagnosis can be assisted by PCR or direct immunofluorescence [3, 4]. Chickenpox can manifest as itching and fever throughout the body, accompanied by symptoms such as erythema, papules, blisters, and scabs. Skin damage usually starts on the trunk or face, spreads outward to the scalp and limbs, and occasionally affects the palms and soles of the feet. The most concentrated areas of lesions are usually the trunk and proximal limbs [5]. DNA detection of VZV in blood and saliva is helpful for the diagnosis and prognosis of atypical chickenpox [6]. Clinical diagnosis could be established based on both the presentations and the patient’s medical history. Furthermore, the assessment of recovery is determined by observing changes in the skin lesions and the patient’s overall condition. The coexistence of herpes zoster and chickenpox is rare, and there have been occasional reports both domestically and internationally [7]. Its mechanism may be immune deficiency, such as human immunodeficiency virus infection, kidney transplantation, immune suppression, etc. [8].
For patients with underlying diseases or immune deficiency due to chemotherapy/radiation therapy for tumours, the likelihood of developing herpes zoster is higher than in the general population. This case is a kidney transplant patient who requires lifelong immunosuppression to prevent organ rejection. However, this intervention can decrease the patient’s cellular immunity, thereby increasing the risk of developing HZ again due to reactivation of the latent varicella zoster virus [9, 10]. In treating herpes zoster, oral brivudine tablets are as effective as intravenous acyclovir, providing more options for outpatient treatment of herpes zoster in patients with immune dysfunction. Brivudine tablets can control pain earlier and must be administered once a day only [11, 12].
Brivudine can be applied to children with chickenpox and even to children with chickenpox and cancer, and the toxic side effects of brivudine on bone marrow, liver, kidneys, and other organs have not been observed [13, 14]. All case was not suitable for treatment with acyclovir due to abnormal renal function, so brivudine was chosen for treatment, and it has good efficacy and safety [15]. There is no relevant research on the use of brivudine for the treatment of chickenpox, and this case provides a reference value for the treatment of chickenpox or chickenpox combined with herpes zoster with brivudine.