Introduction
Scabies is an infectious disease caused by Sarcoptes scabiei var. hominis which was previously described as “itch mite” [1]. Generalized pruritus, which worsens at night, is a cardinal symptom of scabies. Scabies presents with multiple morphologies, varying generalized papular classic rash to atypical nodules, urticaria, crusted plaques or bullous lesions [2, 3].
Recently released diagnostic criteria by the “International Alliance for the Control of Scabies (IACS)” group allows physicians to standardize diagnosis of scabies with three main groups: confirmed (Level A), clinical (Level B) and suspected (Level C) scabies with subgroups [4].
Bullous scabies (BS) was first described by Bean in 1974 and is an infrequent and atypical presentation of scabies, presenting as blister formation with or without burrows, pruritic plaques, and nodules of scabies [5, 6]. The mechanism of bullous formation remains unknown, possible pathogenesis of BS was considered including autoeczemation, superinfection, direct injury or secretion of lytic enzymes by scabies mites, and cross-reactivity of scabies protein with basement zone antigens [5, 7].
To date, nearly 50 cases with BS have been described and two-thirds of them are over 60 years old [5, 8–10]. One patient aged 90 years with haemorrhagic BS has been described so far [9]. No paediatric case with haemorrhagic BS has been described.
Aim
We herein report 5 paediatric BS cases, 2 with haemorrhagic bullae, successfully treated with 10% sulfur ointment, supporting superinfection pathogenesis with positive bacterial culture.
Material and methods
This is a retrospective study of paediatric BS cases seen at two tertiary care centres. Previously described bacterial culture, antibiogram and follow-up records were investigated retrospectively. Confirmed scabies cases, according to the “International Alliance for the Control of Scabies (IACS)” [11] with bullae were included. Informed consent was obtained from patients’ parents.
Results
Case 1
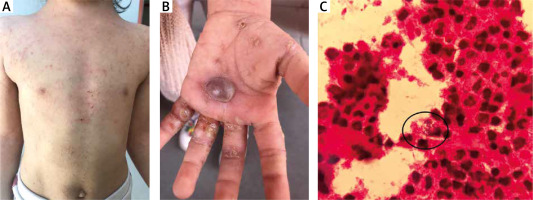
A previously healthy 4-year-old girl presented with a 1-month history of nocturnal and generalized pruritus with generalized rash and purple blistering on her left hand. All family members, including her twin brother, were suffering from the same signs and symptoms without blistering. Physical examination revealed generalized excoriated papules (Figure 1 A) with tense haemorrhagic bullae on her left palm, 3 × 3.2 cm in size (Figure 1 B). Nikolsky’s sign and mucosal involvement were negative. She also had burrows with mite, which was visualized by using dermoscopy and compatible with both confirmed (Level A3) and clinical scabies (Level B1, B3) diagnosis according to IACS diagnostic criteria. Aspiration culture and direct microscopy were performed, methicillin-sensitive staphylococcus aureus was identified (Figure 1 C). Laboratory tests including acute phase reactants were normal. The patient and family members were treated with topical 10% sulfur ointment alone, which resulted in rapid improvement on pruritus and bullae. No recurrence occurred during 2 years’ follow-up.
Case 2
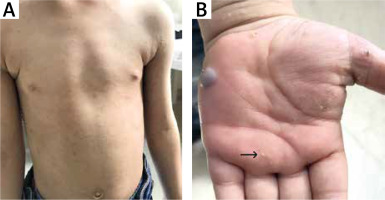
A previously healthy 4-year-old boy was referred to the dermatology department with a 2-week history of generalized pruritus and blistering on his left hand. All family members were suffering from pruritus for 1 month and his sister also had blistering. Physical examination revealed generalized excoriated papules (Figure 2 A), burrows on palms (Figure 2 B) and soles and tense haemorrhagic bullae on his left hand, 1.3 × 1.4 cm in size (Figure 2 B). Nikolsky’s sign and mucosal involvement were absent. He was also qualified for both confirmed and clinical scabies diagnosis (IACS Level A3, B1 and B3). Aspiration culture from bullae was performed, methicillin-sensitive staphylococcus aureus was identified. Laboratory evaluation revealed elevated inflammatory markers (leucocytosis 13.34 × 103/µl, neutrophilia 8.04 × 103/µl and C-reactive protein 6.05 mg/l). The patient was treated with topical 10% sulfur ointment with oral amoxicillin – clavulanic acid. Rapid improvement on both pruritus and bullae was achieved. No recurrence occurred during 5 months’ follow-up.
Case 3
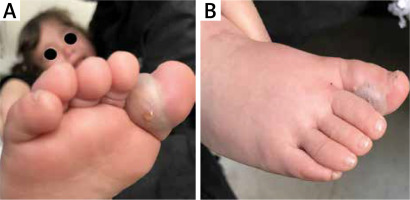
A previously healthy 2-year-old girl, sister of case 2, was referred to the dermatology department with a 1-month history of generalized rash and nocturnal pruritus. She also had a 1-week history of blistering on her left foot. Physical examination revealed generalized papular rash, burrows on palms and soles, and tense bullae on her right first toe, 2.4 × 1.9 cm in size (Figures 3 A, B). Nikolsky’s sign and mucosal involvement were negative. She was also qualified for confirmed and clinical scabies diagnosis (IACS Level A3, B1, and B3). Aspiration culture from bullae was performed, methicillin-sensitive staphylococcus aureus was identified. Laboratory evaluation revealed elevated inflammatory markers (leucocytosis 21.49 × 103/µl, neutrophilia 18.14 × 103/µl and C-reactive protein 60.01 mg/l). The patient was hospitalized and treated with topical 10% sulfur ointment with intravenous clindamycin. Rapid improvement on both pruritus and bullae was achieved. No recurrence occurred during 5 months’ follow-up.
Case 4
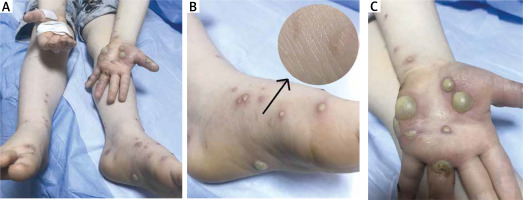
A 3.5-year-old boy with oculocutaneous albinism type IV presented with a 2-week history of generalized rash, nocturnal pruritus and blistering on both hands and feet. Physical examination revealed generalized papular rash, burrows on soles (Figure 4 B) and multiple bullae on palms and soles, varying in size (Figure 4 A–C). Nikolsky’s sign and mucosal involvement were absent. He was qualified for confirmed and clinical scabies diagnosis (Level A3, B1, and B3). Group-A beta haemolytic streptococcus was identified from bullae aspiration material. Laboratory evaluation revealed elevated inflammatory markers (leucocytosis 16.91 × 103/µl, neutrophilia 13.01 × 103/µl, C-reactive protein 132 mg/l, sedimentation 29 mm/h). The patient was hospitalized and treated with topical 10% sulfur ointment with intravenous amoxicillin – clavulanic acid. Rapid improvement on both pruritus and bullae was achieved. No recurrence occurred during 9 months’ follow-up.
Case 5
A previously healthy 4-year-old boy presented with a 2-month history of generalized rash, nocturnal pruritus and blistering on hands. Physical examination revealed generalized excoriated papules (Figures 5 A, B), burrows on palms and multiple pustules and bullae on hands, varying in size (Figure 5 C). Nikolsky’s sign and mucosal involvement were absent. Laboratory tests were normal. Culture from aspiration material was performed. Methicillin-sensitive staphylococcus aureus was identified. The patient was treated with 10% sulfur ointment alone, rapid improvement on both pruritus and blistering was achieved. No recurrence occurred during 1 month’s follow-up.
Discussion
BS is a rare subtype of scabies, with a predilection for elderly males [5]. The mechanism of BS is not fully understood; superinfection, friction due to pruritus, autoeczemation, direct injury from scabies mite’s lytic enzymes, cross-reactivity of scabies protein with basal membrane zone antigens are considered to be possible reasons [3, 5, 8, 10, 12–15].
Our cases had bacteria-positive bullae aspiration cultures, and mites and burrows were visualized on non-bullous areas accompanying classic scabies symptoms. They were in the paediatric age group and fulfilled the “International Alliance for the Control of Scabies” diagnostic criteria with visualized mites by dermoscopy with the classic “delta wing jet” sign. Therefore, no further diagnostic interventions, such as skin biopsy or scraping were performed. Cases 2, 3 and 4 were treated with a combination of topical anti-parasitic drugs and systemic antibiotics. Cases 1 and 5 were treated with 10% sulfur ointment alone, no antibiotic therapy was needed which might be because of the antibacterial effect of sulfur [16]. All cases achieved rapid clinical improvement on signs and symptoms including pruritus, generalized rash and bullae formation.
Published articles point out that scabies burrows and scybala contain both streptococci and staphylococci [17]. In addition, there is a clear link between scabies and acute post streptococcal glomerulonephritis and epidemiological links between scabies-associated pyoderma and acute rheumatic fever [18], which also supports superinfection pathogenesis of BS.
Reported cases over 60 years of age suggest a possible relationship between bullous pemphigoid (BP) and BS [19–21]. However, since BS is more common in the elderly like BP, this may be simultaneous occurrence of both diseases in a patient independently from each other, pruritus due to scabies may have triggered characteristic BP lesions via a Koebner phenomenon [3].
Apparently, the improving course of the disease with treatment and positive bacterial culture in our cases support the superinfection pathogenesis of paediatric BS, which has also been suggested in previously published articles. This neglected ancient disease can present in many different forms clinically, and bullous form may need antibiotic regimens in addition to anti-parasitic therapy especially with the treatments other than sulfur.