Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first described in Wuhan, China, in December 2019 and according to the World Health Organization, up to 24th March 2022, 472,816,657 confirmed cases of COVID-19 have been reported, including 6,099,380 deaths. Coronaviridae family members, including SARS-CoV-2, SARS-CoV and MERS-CoV, are enveloped viruses characterized by a positive single-stranded RNA genome of about 30 kb. Angiotensin converting enzyme 2 (ACE2) has been established as the main viral receptor for SARS-CoV and SARS-CoV-2 [1].
While SARS-CoV-2 is documented to cause substantial pulmonary disease, including pneumonia and acute respiratory distress syndrome (ARDS), many other extrapulmonary manifestations have been identified. Several mechanisms are involved in the pathophysiology of multisystem injury secondary to infection with SARS-CoV-2, such as direct viral toxicity, endothelial cell damage and thromboinflammation, and dysregulation of the immune and renin-angiotensin-aldosterone (RAAS) system [2].
Venous thromboembolic events, mainly pulmonary embolism [3], significantly contribute to morbidity and mortality in COVID-19 [4]. Several mechanisms have been proposed as possibly related to COVID-19 thrombotic events, including thrombosis triggered by cytokine storm, antiphospholipid antibody syndrome, macrophage activation syndrome, the complement cascade, and RAAS dysregulation [5].
As regards the vascular diseases of the liver in patients with COVID-19, only sparse data are currently available. There is evidence that microvascular thrombosis may induce liver dysfunction during the disease. Tsutsumi et al. [6] found that higher D-dimer level and white blood cells (WBC) count were independently associated with the elevation of alanine aminotransferase (ALT), suggesting that the potential coagulopathy might be associated with liver damage through microvascular thrombosis in addition to systemic inflammation.
Pioneering work by Sonzogni et al. [7] studied post-mortem wedge liver biopsies from 48 patients who died from severe pulmonary COVID-19 with respiratory failure. The histopathological findings were highly suggestive for marked derangement of the intra- hepatic blood vessel network secondary to systemic changes, induced by the virus that could target not only lung parenchyma but also the cardiovascular system, coagulation cascade and endothelial layer of blood vessels. In a more recent autopsy study from New York in 100 COVID-19 patients, venous outflow obstruction was evident in 45% of the livers, early organizing thrombi in portal venules in 40%, and in terminal hepatic venules in 22% [8].
In this review, we focus on and summarize the published experience with respect to the coagulation disorders in the vascular system of the liver in patients with COVID-19.
Material and methods
We searched all articles published up to April 22th, 2021, in the database of PubMed, as well as Google Scholar, using the search terms “COVID-19 AND vascular diseases of the liver”, “COVID-19 AND portal vein thrombosis”, “COVID-19 AND Budd-Chiari syndrome”, “COVID-19 AND hepatic vein thrombosis”, “COVID-19 AND splanchnic vein thrombosis” and “COVID-19 AND sinusoidal obstruction syndrome”.
Articles associated with our searches were reviewed, and relevant data were abstracted. All studies were written in English and refer to confirmed COVID-19 cases. As regards case reports and case series, we extracted the following data for each study: name of the author, gender and age of the patient, previously known medical history, signs and symptoms at presentation, radiology findings confirming the diagnosis, as well as the preferred treatment chosen for each case. Such detailed information was not available for cases found in cohort studies and studies where large numbers of patients were recorded.
Results
All case reports and one case series reporting thrombotic events in the liver in the context of COVID-19 are summarized in Table 1 [9-19].
Table 1
Overview of existing studies with vascular liver diseases in patients with COVID-19
| Author | Age (years) | Sex | Previous known medical history | Symptoms | Radiology findings | Treatment |
|---|---|---|---|---|---|---|
| Ofosu et al. [9] | 55 | Male | Unremarkable | Fever, dyspnea, confusion | Thrombi in the main anterior and posterior divisions of the right portal vein | Apixaban 5 mg BID |
| LaMura et al. [10] | 72 | Male | Parkinson’s disease, dementia, anxious depressive disorder | Fever, jaundice, periumbilical tenderness | Total occlusion of the left portal venous system and of secondary branches of the right portal vein | SC enoxaparin 100 IU BID |
| Jafari et al. [11] | 26 | Male | Asthma | Respiratory distress and right upper quadrant abdominal pain | Portal vein thrombosis | Continuous IV heparin infusion 1000 U/h |
| Low et al. [12] | 51 | Male | Unremarkable | Low extremity pain and DVT | Non-occlusive thrombus in the right and left portal vein | IV heparin |
| Franco-Moreno et al.[13] | 27 | Male | Unremarkable | Abdominal pain, fever | Non-enhancing filling defect in the right branch of the portal vein | SC enoxaparin 1 mg/kg BID |
| Borazjani et al. [14] | 23 | Male | Asthma, alcohol use | Abdominal pain, ascites | Filling defect in the right and left main portal vein | SC enoxaparin 1.5 IU/kg/d (60 IU BID) |
| De Barry et al. [15] | 79 | Female | Unremarkable | Fever, dyspnea, abdominal pain, diarrhea, ascites | Right portal vein occlusion, upper mesenteric vein thrombosis, jejunal artery occlusion | NR |
| Del Hoyo et al. [16] | 61 | Female | DMT2 | Abdominal pain, vomiting | Thrombosis in the right hepatic vein, thickening of the small bowel loops | NR |
| Abeysekera et al. [17] | 42 | Male | Chronic hepatitis B | Fever, cough | Portal and mid-superior mesenteric vein thrombosis | Apixaban 5 mg BID |
| Ignat et al.[18] | 28 | Female | Unremarkable | Abdominal pain, vomiting | Superior mesenteric and portal vein thrombosis | NR |
| Petters et al. [19] | 3 | Female | Liver transplant recipient with a history of Caroli disease | Fever, abdominal pain, diarrhea | Complete occlusion of extrahepatic portal vein | SC enoxaparin and re-cannulation of the main portal vein by interventional radiology |
A total of 11 cases were reported, 7 males and 4 females. The youngest patient was 3 years old and the oldest was 79 (mean age 45 years).
Amongst the 11 patients, seven had no past medical history of liver disease. One patient had a positive history for alcohol use, yet without previously documented liver disease, one patient had had fatty liver, and another patient had chronic hepatitis B (stage 2 fibrosis). The youngest, a 3-year-old patient, was diagnosed with Caroli disease and was a liver transplant recipient.
The clinical presentation included abdominal pain as the main symptom in seven cases. Three of them also had ascites, and one presented with jaundice. In 10 cases, the diagnosis of the thrombotic event was confirmed with a CT scan. In the pediatric patient, thrombosis was confirmed by an abdominal ultrasound scan.
In the cases described by Jafari et al. [11] and Petters et al. [19], the main portal vein was involved, while two of the patients had had occlusion of the right portal vein [9, 13]. Three cases were described where both the left and the right branch of the portal vein were occluded [10, 12, 14]. In one of the cases, described by de Barry et al. [15], the right portal vein, the upper mesenteric vein, and the jejunal artery were all occluded. Abeysekera et al. [17] described involvement of the main portal and mid superior mesenteric vein, while Ignat et al. [18] described a case where both the main portal and the main superior mesenteric vein were occluded. One patient was diagnosed with occlusion of the right hepatic vein [18].
With respect to the therapeutic approach, two patients were treated with apixaban 5 mg BID per os starting from the day of the diagnosis, while four were treated with subcutaneous (SC) injection of enoxaparin. One patient additionally underwent recanalization of the main portal vein by interventional radiology. Two patients received intravenous (IV) heparin, while in four cases the authors did not report the selected treatment.
In 5 patients, no association was found with inherited or acquired prothrombotic risk factors. One patient was diagnosed with JAK2 mutation, and another was diagnosed with essential thrombocythemia. In five cases, no thrombophilia screen was reported.
As regards the outcomes, seven of the cases improved and the patients were eventually discharged [9, 11, 13-15, 17, 18]. Three other patients improved, but no further information about their discharge was reported [10, 12, 19]. On the other hand, the cases described by de Barry et al. [15] and del Hoyo et al. [16] had a fatal outcome: the first patient was diagnosed with occlusion in the right portal vein, superior mesenteric vein and in the jejunal artery, and the second was diagnosed with occlusion in the right hepatic vein.
Furthermore, as shown in Table 2 [20-22], we found cases reported in large study groups and cohort studies where no particular information was given about demographics, clinical characteristics or imaging. In the study of Taquet et al. [20], 537,913 patients were included and 94 were found to have portal vein thrombosis. Kampouri et al. [21] and Rieder et al. [22] described one case of portal vein thrombosis each, in study groups of 443 and 49 patients respectively. Apart from the data presented in the aforementioned table, Bilaloglu et al. [23] also presented a study where among 3343 COVID-19 positive patients, 533 experienced thrombotic events and 32 of them were indistinctively categorized as having one of the following: acute limb ischemia, upper extremity arterial thrombosis, renal and splenic infarcts or portal vein thrombosis.
Table 2
Large studies with data for PVT in COVID-19 patients
| Author | Number of COVID-19 positive patients studid | Incident involving the vascular system of the liver | Total number of patients affected | Clinical course of patients | Outcome |
|---|---|---|---|---|---|
| Taquet et al. [20] | 537,913 | PVT | 211 | Not available. Data collected retrospectively through electronic database | 42 deaths |
| Kampouri et al. [21] | 443 | PVT | 1 | Not available. Patient studied through a cohort of patients with venous thromboembolism | Not available |
| Rieder et al. [22] | 49 | PVT | 1 | Hospitalized for 7 days, no need for ICU admission | Recovered |
Discussion
During the SARS-CoV-2 pandemic it was documented that critically ill patients may present a hypercoagulative state, leading to major thromboembolic events [24]. Endothelial cell damage, subsequent inflammation, and the generation of a prothrombotic environment are some proposed pathophysiological mechanisms of COVID-19.
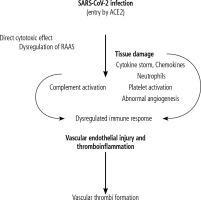
The presence of a hypercoagulative state triggered by multifaceted inflammatory responses to the virus has been called thromboinflammation, and the hallmark of this is microvascular thrombosis associated inflammation. SARS-CoV-2 can induce thrombotic phenomena with various mechanisms such as cytokine storm with activation of leukocytes (with a fundamental role of neutrophils), endothelial cell dysfunction and platelets’ activation (platelet activation is directly linked to arterial thromboses), resulting in generation of thrombin and the formation of fibrin, whereas at the same time fibrinolysis is limited. In this interplay, inflammation and coagulation act together to block the spread of the pathogen [25]. Another significant process involved in COVID-19 related thrombosis is excessive complement activation that favors tissue damage and intravascular thrombosis [26].
Infection-mediated endothelial injury (characterized by elevated levels of von-Willebrand factor elevation) and endothelialitis (characterized by the presence of activated neutrophils and macrophages) found in multiple vascular beds (lungs, heart, kidneys, liver, small intestine) in infected patients can trigger excessive thrombin production, inhibit fibrinolysis and activate complement pathways, thus initiating inflammation and thrombosis, and finally leading to microthrombosis and vascular dysfunction [2, 24].
Systemic inflammation is documented that leads to toll-like receptor and tissue factor pathway activation, platelet-leukocyte aggregation, as well as activation of macrophages, monocytes, endothelial cells, platelets and lymphocytes in response to a viral infection [1, 2]. The dysregulation of the immune response and cytokine-release syndrome, due to overactivation of innate immunity in the setting of T-lymphocyte depletion, is characteristic in severe COVID-19 [4]. Indeed COVID-19 infection can cause a massive inflammatory response with high levels of inflammatory cytokines (tumor necrosis factor α [TNF-α], interleukin 2, 6, 7) and chemokines, resulting in the cytokine storm. This inflammatory reaction is directly related to hypercoagulability [26]. An important confounding factor which is recently recognized is the pathological angiogenesis, as implied by the overexpression of proangiogenic factors (VEGF, FGF) in COVID-19 patients (Fig. 1).
Fig. 1
Pathophysiological aspects evaluating hypercoagulation and throm- bosis in COVID-19
ACE2 – angiotensin converting enzyme 2, RAAS – renin angiotensin aldosterone system
It is important to identify whether the liver involvement in COVID-19 affects a patient with or without pre-existing chronic liver disease. SARS-CoV-2 is reported that can be directly cytopathic, whereas the liver involvement could also be in the context of the abovementioned uncontrolled immune reaction, sepsis or drug-induced liver injury [27, 28]. Pre-existing chronic liver disease seems to be a risk factor for poor outcome; especially cirrhosis has been identified as a predictor for mortality [29], while in patients without such history the liver injury is mostly mild. In a large cohort of 745 chronic liver disease patients from an international registry with SARS-CoV-2 infection, mortality was 32% in cirrhotics vs. 8% in non-cirrhotics (p < 0.001). Baseline liver disease stage (Child-Pugh score) and alcoholic liver disease were independent risk factors for death from COVID-19 [30].
Hepatic dysfunction was significantly more frequent in critically ill patients and was associated with poor outcome [27]; a hepatocellular pattern of injury was identified in 14-53% of the patients, whereas cases with severe acute hepatitis have been reported [24, 25, 28]. In a systematic review, pooled prevalence of liver function test abnormalities was found to be 19%, and there was a relationship with disease severity, as there was with elevated bilirubin on admission. As regards cholestatic liver enzymes, it seems there is an elevation of ALP in 6% and γ-glutamyltranspeptidase (γ-GT) in 21% of COVID-19 patients. Moreover, the possible role of drug-induced liver injury (due to e.g. remdesivir, lopinavir, tocilizumab) should not be overlooked [31-34].
COVID-19 disease is associated with abnormal inflammatory and coagulation markers. In a retrospective cohort study of 138 patients undergoing imaging studies, 44 had evidence of venous thromboembolism; in the univariate analysis male sex, elevated CRP, and platelets on admission were associated with venous thromboembolism while only male sex was significant in multivariate analysis [35].
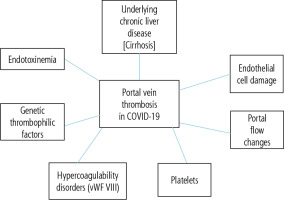
The incidence of thrombotic events in the vascular system of the liver and their subsequent impact on morbidity and mortality of the patients have not been thoroughly investigated. In our study we reviewed a limited number of reports (11 case reports and 1 case in a case series) in the literature that specifically focus on vascular liver diseases during the course of COVID-19. Moreover, we identified relevant data within larger COVID-19 patient cohorts, partly providing an estimate of the contribution of vascular liver diseases to the overall morbidity of this population. The most frequently encountered clinical event in our study was that of partial or complete portal vein thrombosis, and several underlying pathophysiological factors could be proposed for this (Fig. 2).
Fig. 2
Pathophysiological aspects in portal vein thrombosis in COVID-19
vWF-VIII – von Willebrand factor VIII
It is a weakness of our review that, despite the universal spread of the disease, there are either limited specific data from a small number of case reports or actually little information from larger cohorts, including significant heterogeneity in the available laboratory and histopathological data.
In conclusion, patients with COVID-19 seem to be at high risk for thrombotic complications, which significantly increase the morbidity and mortality. The involvement of the vascular system of the liver has been suggested by some reported cases, while possible long-term complications remain to be elucidated. A plethora of mechanisms has been proposed as the underlying pathophysiologic events triggering thrombosis, while their actual role and significance need further investigation. Pre-existing liver disease and especially cirrhosis are important risk factors for adverse outcomes in COVID-19. The abovementioned cases are the only reported cases of COVID-19 affecting the vascular system of the liver, and this limited experience highlights the importance of anticoagulation therapy, and emphasizes the need for greater awareness in cases where symptoms related to the gastrointestinal tract occur.






