Despite advancements in radiotherapy (RT) techniques radiation-induced dermatitis (RD) remains a prevalent side effect of RT. Acute radiation-induced dermatitis (ARD) usually occurs within days or even weeks after the start of RT [1]. In contrast, chronic radiation-induced dermatitis (CRD) often emerges months after RT [2]. In two prospective observational studies, we have described the dermoscopic features of ARD and CRD, without focusing on their progress [3, 4].
Here, we present two cases detailing the dermoscopic evolution of skin lesions from ARD to CRD.
Our study presents the clinical and dermoscopic evolution of RD (ARD into CRD) in two patients with head and neck cancer (HNC) undergoing radiochemotherapy. Clinical and dermatoscopic assessments for ARD and CRD were conducted during treatment in the Inpatient Department of Radiation and Clinical Oncology, Maria Sklodowska-Curie National Research Institute of Oncology (MSCNRIO) in Gliwice. Two patients were followed up for 3 and 6 months after completion of radiotherapy. Dermoscopic images were obtained using a DermLiteCam (3Gen, LLC, San Juan Capistrano, CA, USA), a digital dermoscopic camera with polarized light at 10× magnification. The control area consisted of skin areas of the same patient that were not exposed to radiotherapy (right and left lower part of the retroauricular area). Clinical grading followed the RTOG/EORTC classification [5]. Dermoscopic assessments of ARD and CRD were based on the consensus of the International Dermoscopy Society (IDS) [6].
In Case A, a 65-year-old man diagnosed with squamous cell carcinoma of the middle pharynx, surgical treatment was followed by radiochemotherapy (CHRT) with a total dose of 66 Gy in 33 fractions, and 5 cycles of chemotherapy with cisplatin at a dose of 40 mg/m2 administered simultaneously.
In Case B, a 57-year-old man diagnosed with squamous cell carcinoma of the larynx received 4 cycles of induction chemotherapy (cisplatin, 5-fluorouracil), radiotherapy a total dose of 70 Gy in 35 fractions with concurrent chemotherapy based on two cycles of carboplatin at a dose of 5 mg/AUC.
Both patients developed the same clinical grade (G) (G2 in ARD and G1 in CRD) (Figures 1 B, D, F; 2 B, D, F), with evolving dermoscopic features. Dermoscopic manifestations of ARD in both cases included linear vessels with branches, linear curved vessels, and patchy scale (Figures 1 A, 2 A) in different colours. In addition, clustered distribution of vessels and white structureless areas were observed in Case A (Figure 1 A) while reticular distribution of vessels, follicular plugs, perifollicular white colour and perifollicular pigmentation were prevalent in Case B (Figure 2 A).
Figure 1
Case A. Dermoscopic images of ARD (A) and CRD (C, E) described according to the International Dermoscopy Society [6] (IDS) by Errichetti et al. ARD (B) and CRD (D, F) on macroscopic images across grades (G) G1 to G2, assessed according to RTOG/EORTC [5] criteria. A – Linear vessels with branches and linear curved vessels in clustered distribution, white and yellow patchy scale, and white structureless areas; B – Bright erythema, epilation, dry desquamation, moderate oedema (G2); C – Dotted, linear vessels with branches and linear curved vessels in clustered and unspecific distribution, white patchy scale, white structureless areas, and white lines. D – Patchy atrophy, pigmentation change, total hair loss, and moderate telangiectasias (G1); E – Dotted, linear vessels with branches and linear curved vessels in unspecific distribution, white lines, white structureless areas, and brown dots or globules; F – Patchy atrophy, pigmentation change, total hair loss and moderate telangiectasias (G1)
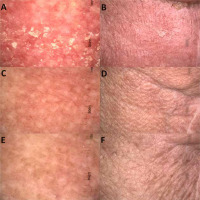
Figure 2
Case B. Dermoscopic images of ARD (A) and CRD (C, E) described according to the International Dermoscopy Society [6] (IDS) by Errichetti et al. ARD (B) and CRD (D, F) on macroscopic images across grades (G) G1 to G2, assessed according to RTOG/EORT criteria [5]. A – Linear vessels with branches and linear curved vessels in reticular distribution, brown patchy scale, follicular plugs, perifollicular white colour, and perifollicular pigmentation; B – Bright erythema, epilation, moist desquamation, and moderate oedema (G2); C – Dotted vessels in clustered distribution, white patchy scale, perifollicular white colour, white lines, and brown dots or globules. D – Patchy atrophy, pigmentation change, and total hair loss (G1); E – Dotted vessels in unspecific distribution, perifollicular white colour, white structureless areas, white lines, and brown dots or globules; F – Patchy atrophy, pigmentation change and total hair loss (G1)
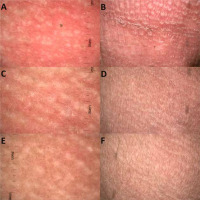
In the third month post-radiotherapy, dotted vessels in clustered distribution, white patchy scale and white lines emerged in both cases (Figures 1 C, 2 C). In Case A, linear vessels with branches, linear curved vessels and white structureless areas were still observed (Figure 1 C). In Case B perifollicular white colour was still observed, and brown dots or globules appeared (Figure 2 C).
In the sixth month post-radiotherapy, dotted vessels persisted in both cases, albeit in an unspecific distribution (Figures 1 E, 2 E). White structureless areas, white lines and brown dots or globules were also observed (Figures 1 E, 2 E). In addition, linear vessels with branches and linear curved vessels were still present in Case A (Figure 1 E) and perifollicular white colour persisted in Case B (Figure 2 E).
This study illustrates the dynamic dermoscopic evolution of radiation dermatitis. In both cases, linear vessels with branches and linear curved vessels and patchy scale were observed in ARD, dotted vessels with clustered distribution, white patchy scale, and white lines appeared in the 3rd month, and in the 6th month, dotted vessels persisted but the type of distribution changed to unspecific. Further research with a larger patient cohort is needed to elucidate the significance of dermoscopic features and their potential predictive role in the development or persistence of skin lesions in CRD.








