Melanonychia is the result of excessive melanin deposition in the nail bed area and appears as typical brown-black discolouration. The occurrence of these changes may be due to stimulation and overgrowth of the nail matrix, invasion of the nail plate by melanin-producing pathogens, subungual haemorrhage, and medications. Drug-induced melanonychia (DIM) typically affects multiple nails and presents as longitudinal or transverse bands ranging in colour from light brown to black [1, 2]. It can affect single or several fingernails or toenails at the same time. As dermoscopy of DIM is not extensively covered in the literature, the manifestation presented may serve as a critical reference point for clinicians who may encounter similar cases.
The aim is to present 2 patients with DIM in the course of polycythaemia vera (myelodysplastic syndrome) treated with hydroxycarbamide (HU).
Case 1: A 77-year-old female patient, diagnosed with polycythaemia vera in 2017, has been under the care of the Transplantation Outpatient Clinic of the National Research Institute of Oncology since 2019. Until 2019, she was treated with phlebotomies every 6 months and hydroxycarbamide at a dose of 2 × 500 mg or 3 × 500 mg depending on the haematocrit level, together with permanent anticoagulant therapy. Melanonychia occurred within 2 years of HU therapy (Figures 1 A–D).
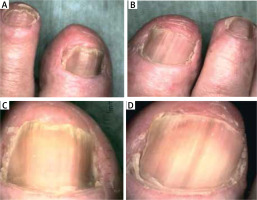
Figure 1
A, B – Clinical presentation of longitudinal drug-induced melanonychia in a 77-year-old patient. A – Nail plates of both hands showing characteristic linearly arranged bands with pseudo-Hutchinson sign. B – Nail plates of the second and third fingers of the right hand affected by melanonychia changes covering more than half of the total surface area. C, D – Dermoscopy shows the presence of linear regular streaks arranged in parallel, with dark brown and light brown pigmentation with a tendence to merge into homogeneous of the nail plate of the third finger of the patient’s right hand (C), and the nail plate of the second finger of the patient’s left hand (D)

Case 2: A 74-year-old female patient was diagnosed with polycythaemia vera in 1991. She was initially treated with phlebotomies and since 2005 with hydroxycarbamide. A trephine biopsy confirmed the diagnosis of polycythaemia vera. Hydroxycarbamide has been used in variable doses, currently at a dose of 2 × 500 mg, which induces melanonychia after 13 years (Figures 2 A–D).
Figure 2
A, B – Clinical examination proves the presence of linearly arranged bands symmetrically on all nail plates, accompanied by longitudinal ridging and roughness, with dark discoloration within the nail plates of the big toe and second toe of the patient’s left foot (A), and the nail plates of the big toe and second toe of the patient’s right foot (B). Dermoscopic presentation shows longitudinal bands of dark and light brown colour irregularly covering the entire width of the nail plate of the left toe (C) and the nail plate of the right toe (D)
Melanonychia can occur as a result of neoplastic and reactive processes and as a side effect of chemotherapy and systemic treatments. The incidence of melanonychia in patients receiving hydroxycarbamide therapy ranges from 4.3% to 55% [3]. Changes manifest within months of starting the drug and resolve within 6 to 8 weeks of discontinuing the drug [2, 4]. Drug-induced melanonychia typically presents as diffuse or complete longitudinal or transverse bands, the latter being almost exclusively drug-induced [2].
Hydroxycarbamide, a hydroxylated urea derivative used in myeloproliferative disorders, is a standard treatment for high-risk polycythaemia vera patients [5]. Nail changes appearing as brown to black streaks are rare but present a diagnostic challenge. Differential diagnosis includes subungual melanoma/nevus, subungual haematoma, ethnic predisposition, ectopic subungual hair and fungal melanonychia [2].
Dermoscopy is useful in examining these changes although malignancy can be difficult to diagnose. Early dermatological diagnosis is recommended when in doubt, taking into account non-melanocytic pigmentation and other factors causing nail plate changes.
In the cases presented, hydroxycarbamide-induced melanonychia presented as numerous brown bands of varying intensity that tended to coalesce into homogeneous areas over several fingers. It is important for clinicians to be aware of the association of melanonychia with certain drugs used in cytostatic therapy in order to avoid anxiety and improve the effectiveness of treatment in these patients without unnecessary complications.








