“Eruptive pruritic papular porokeratosis (EPPP)”, first proposed by Kanzaki in 1992 [1] and designated as “Inflammatory disseminated superficial porokeratosis (Inflammatory DSP)” by Tanaka in 1995 [2], is a special variant of porokeratosis. The typical clinical course consists of asymptomatic DSP for months to years, followed by the acute pruritic exacerbations, and then subsides spontaneously within 12 months [3]. Histopathological examination reveals the characteristic cornoid lamellae. This paper describes a typical case of EPPP in China and summarizes previously reported EPPP cases.
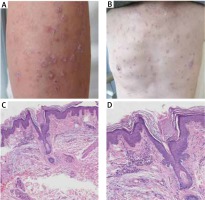
Herein we describe a typical case in China – a 68-year-old man with EPPP for 5 years. After the initial 3 years of asymptomatic DSP, typical eruptions such as annular lesions with a raised and sharply marginated keratotic border suddenly presented with recurrent multiple, pruritic, erythematous papules on his extremities and trunk. The lesions subsided in the winter and recurred in the summer. Physical examination revealed numerous nodular erythematous papules like prurigo nodularis lesions (Figure 1 A), and hyperpigmented brown macules on his trunk (Figure 1 B). The patient had a history of mild hypertension, no other relevant diseases and he was not on medication. Biopsy specimen of a reddish papule on his right upper limb did not show the granular layer and patchy parakeratosis of keratinocytes in the characteristic cornoid lamellae (Figure 1 C). Mild focal lymphocytes (without eosinophils) infiltrates around the blood vessels in upper dermis (Figure 1 D).
Based on the above symptoms, the patient was definitely diagnosed as EPPP. These pruritic papules did not respond well to topical steroids or oral antihistamines. Interestingly, as the winter progressed, the papules levelled off and the itching was reduced, leaving behind some brownish non-inflamed patches in the follow-up.
By analysing 17 cases of EPPP including the one reported here, we found that EPPP might be manifested with the following characteristics (Table 1 [1–14]): (1) history of pre-existing porokeratosis varied from months (> 2 months) to several years except 1 patient who had no pre-existing lesions and no tendency to spontaneous resolution in a 16-month follow-up [4]; (2) less than half of patients had other pre-existing diseases or suspicious triggering factors, including cardiovascular disease, medication history, autoimmune disease, cancer or others; (3) elderly males might be the susceptible population. The mean age of 17 patients was 71 years, including 13 males in contrast to 30–40 years at onset and the 1 : 3 ratio of male : female for the classic porokeratosis [11]; (4) the typical clinical case presents with sudden multiple erythematous papules, accompanied by strong itching, followed by asymptomatic porokeratosis skin lesions; (5) with the cornoid lamellae, histological examination revealed the presence of eosinophils infiltration in 9 patients, more than half of the cases; and (6) the eruptions could subside within 12 months spontaneously in the follow-up [3].
Table 1
Summary of previously reported cases of EPPP
| Case no. | Age of onset | Gender | Pre-existing asymptomatic porokeratosis | Period of pre-existing lesions | Period of significant regression | Other previous diseases/suspicious triggering factors | Tissue eosinophilia | Author |
|---|---|---|---|---|---|---|---|---|
| 1 | 71 | F | + | Several years | 5 months | – | + | Kanzaki et al. [1] |
| 2 | 60 | M | + | Nearly 10 years | NM | CVA/drugs | + | Kanzaki et al. [1] |
| 3 | 75 | M | + | Over 10 years | 6 months | Systemic steroids | - | Kanzaki et al. [1] |
| 4 | 78 | M | + | Several years | 3 months | – | - | Tanaka et al. [2] |
| 5 | 69 | M | - | – | 1 year | – | + | Stork et al. [4] |
| 6 | 77 | M | + | 20 years | 4 months | – | + | Ricci et al. [5] |
| 7 | 50 | M | + | 10 years | NM | – | - | Kang et al. [6] |
| 8 | 74 | M | + | 3 years | 2 months | Cerebral and myocardial infarction, diabetes, gout, and prostatic hypertrophy | + | Makino et al. [7] |
| 9 | 82 | M | + | 1 years | 6 months | – | – | Kanekura et al. [8] |
| 10 | 71 | F | + | 35 years | NM | – | + | Klein et al. [9] |
| 11 | 84 | M | + | 3 years | 1 month | Colon cancer | + | Choi et al. [10] |
| 12 | 68 | M | + | 4 months | 2 months | – | + | Wakatabi et al. [11] |
| 13 | 63 | M | + | Over 13 years | NM | – | – | Tee et al. [3] |
| 14 | 77 | F | + | Over 20 years | NM | – | + | Yamamoto et al. [12] |
| 15 | 80 | M | + | 2 years | NM | Hypertension and hyperuricemia | – | Inazawa et al. [13] |
| 16 | 63 | F | + | 3 years | 2 months+ | Basedow’s disease and oral thiamazole | – | Patrizi et al. [14] |
| 17 | 68 | M | + | 3 years | Up to now | Hypertension | – | Present case |
The reasons responsible for EPPP sudden appearance are still not clear. And the interventions for this particular type of porokeratosis are identical to the classic DSP. Some therapeutic options were used for acute phase lesions such as topical steroids, 5-fluorouracil, assisted freezing, and laser etc. [4, 5], but the efficacy is unsatisfied. Oral antihistamines can be effective against pruritus.
In conclusion, we reported a Chinese man with typical EPPP characteristics. In low temperatures, the eruption tends to resolve, which might be related to season, sunlight, humidity or sweat stimulation. Whereas, the mechanisms and characteristics of EPPP need to be further studied with more similar cases.