Basal cell carcinoma (BCC) with the size of the tumour exceeding 5 cm in diameter used to be called a “giant” variant of BCC [1]. Although BCC is a type of skin cancer widely spread among European population, the occurrence of giant basal cell carcinoma (GBCC) remains uncommon [2]. It has been suggested that GBCC accounts for about 1% of all BCC cases [3].
BCCs typically affect body areas exposed to sun radiation while GBCC shows higher predilection to the trunk [4]. Often GBCC is an invasive tumour linked with heavy tissue destruction, yet it can also appear as a superficial subtype mimicking psoriasis or mushroom-like exophytic tumours [5–7]. Also, GBCCs are characterized by a history of skin lesions that develop over years as the disease rarely causes any subjective symptoms [8]. In addition, due to a larger size, deeper invasion and more frequent metastases GBCC usually has worse prognosis compared to BCC (greater skin removal needs and worse aesthetic results) [9].
This article presents the case of a GBCC located in the left temporal region (with the absence of metastasis) successfully treated with the surgery.
A 63-year-old Caucasian female was admitted to the Department of Dermatology in August 2022 with a large tumour on a left temporal area of the head. According to the history, the lesion had been growing slowly for almost 10 years. The lesion temporarily caused itchiness.
The lesion had been neglected for several years, until it reached the size of 3 cm in diameter in 2019, when the patient decided to seek medical care for the first time. She was referred to the surgical ward for an extensive investigation. Unfortunately, the admission took place at the beginning of COVID-19 pandemic. The patient refused to be admitted due to fear of COVID-19 infection.
After over 2.5 years, the patient decided to visit an oncologist in July 2022, who suspected a malignant melanoma based on assumed quick growth of the tumour – the size of the GBCC was 6 cm at the time (from 3 cm in 2019) with the patient confirming that the growth took place during last 2 years (COVID-19 pandemic duration). The patient was transferred to the Department of Dermatology in August 2022 in order to have full diagnostic and treatment procedures performed.
Medical history revealed several comorbidities including multiple sclerosis, depression, chronic obstructive pulmonary disease, hypertension, obesity (BMI = 29 kg/m2). Also, the patient reported a 40-pack-year history of smoking, no use of any sun protection yet denied chronic UV exposure or sunburn. Additionally, there was no history of prior radiotherapy or exposure to any toxic substances. The family history of skin cancers was negative.
Physical examination revealed exophytic, well-marginated, brown, round-shaped tumour, measuring about 6.5 cm × 6.5 cm. The surface of the lesion was covered with hair glued to the top by a serosanguineous secretion (Figure 1 A). Moreover, there was a purulent secretion coming from the tumour. On palpation the lesion was firm and painless. No lymphadenopathy was observed during clinical examination and USG of the lymph nodes.
Figure 1
Clinical presentation of the tumour: A – pre-operation, B – after the excision, C – the niche covered by a skin graft, D – the wound after healing

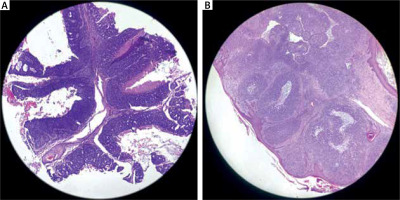
The lesion was biopsied with histopathologic examination showing a nodulocystic type of GBCC (Figure 2 A). The removal of the GBCC via surgical operation was suggested. There were no operation contraindications and the patient agreed to the operation.
Figure 2
Images from histological samples: A – punch biopsy sample at 100× magnification; B – part of the tumour after excision at 40× magnification
Wide local excision with skin-graft and local anaesthesia was performed (Figure 1 B). The tumour was successfully removed with a healthy skin margin. GBCC was shallow and did not infiltrate any deeper tissues. A large post-operation skin niche was closed using a split-thickness graft obtained from the inner side of a patient’s right arm (Figure 1 C). No complications after the surgery were observed. A tie-over dressing was removed on day 5, sutures on the head on day 7 and on the arm on day 14. Post-operation observation revealed that the wounds were healing well (Figure 1 D).
The histological examination of the excised lesion confirmed the initial diagnosis based on the punch biopsy and the excised margins did not contain neoplastic cells (Figure 2 B). No recurrence of the tumour was observed during 1-year follow-up.
BCC is a slow-growing, most common globally non-melanoma skin cancer. Despite its high prevalence, the estimated incidence of metastatic BCC stands at 0.003–0.5%. However, with a long course of the disease and large size of the tumour, BCC has the ability to infiltrate, destroy tissues, and metastasize. Despite the diameter of the tumour exceeding 5 cm, no metastases were observed in the above-reported case.
Excessive exposure to ultraviolet radiation, elderly age, low/fair skin phenotype, exposure to arsenic or ionizing radiation are common risk factors for basal cell carcinoma. Several studies indicate that self-negligence is a key factor leading to the development of a giant BCC. Next, smoking was associated with an increased prevalence of GBCC [10]. In our case, the patient was of Caucasian race, advanced in years, an active smoker, and the tumour was located in the sun-exposed area. In addition, the long period of the patient’s negligence and lack of proper medical care led to the development of the giant version of BCC.
Surgical excision is the gold standard in the treatment of GBCC. The alternative non-surgical methods of GBCC treatment have been reported in the literature including radiotherapy [11], chemoradiotherapy [12], vismodegib [13], imiquimod [14], imiquimod-cryosurgery combination and acitretin-imiquimod combination [15]. The literature points to several options for GBCC non-operation treatments yet with limited structured recommendations; we see space for the medical society to further examine next-best GBCC non-surgical options and provide formal guidelines for dealing with GBCC when the operation is excluded.
While this paper does not dispute (yet acknowledges) the extensive impact COVID-19 had on the healthcare systems, this reported case was influenced by the pandemic. In our case, the patient denied the presence of the tumour for several years and then fearing SARS-CoV-2 infection in health centres avoided treatment for 2–3 years, which resulted in the large size of the tumour and the need for an advanced surgical procedure to cure the disease.








