Extramammary Paget’s disease (EMPD) is an infrequent tumour that is characterised by a chronic eczema-like rash around the anogenital region. The most common symptom of extramammary Paget’s disease is mild or intense itching around the lumbar, genital, perineal, or perianal regions. Pain and bleeding may result from potential injuries. The thick plaques can be red, squamous, and rough. The first symptoms are itching and burning from one or more persistent plaques. Due to the rarity of the disease, it is difficult to find a specialist. Differential diagnosis is complicated by the fact that EMPD symptoms can mimic those of other diseases [1]. The diagnostic process should include physical, microscopic, immunohistochemical, and interdisciplinary examinations. EMPD is usually treated surgically by removing the skin lesion [2–4]. In some cases, treatment can be effective, such as photodynamic and imiquimod treatment, radiotherapy, chemotherapy, androgen therapy, and CO2 laser ablation [5–7].
Male patients use the term “jock itch” for the symptoms. In some cases, there is mild sensitivity or there are no symptoms in the affected region. The disease most often occurs between the ages of 50 and 70 years, but it can also appear earlier [8]. The disease is infrequent, and usually the progress is slow. If the disease is diagnosed early, the prognosis is good [9]. EMPD can also be aggressive and invade the dermis and subcutaneous tissues. As a consequence, invasive carcinoma and metastases can develop. This is the reason why physical examinations are very important in the following regions: axillary, genital, and anal [10]. The most commonly affected areas among women are the vulva or the anus, but the disease can affect the mons pubis, vagina, and thighs. The most commonly affected areas among men are the genital organs (scrotum, penis), anal, perianal, lumbar regions, and thighs. Tumours that invade the eyelids, scalp, nose, and acoustic meatus are extremely rare. EMPD is located on the apocrine gland-rich areas: axilla, inguinal area, scrotum, vulva, retroauricular region, and sweat glands [11]. For surgical treatment, it is important to determine the extension of the tumour [12]. When EMPD is suspected, the diagnosis is typically confirmed via a skin biopsy of the lesion. The location of extramammary Paget’s disease is useful in predicting the risk of associated cancer. In some cases, EMPD appears 10–15 years before invasive carcinoma and metastases. Approximately 25–35% of EMPD cases around the anal region are associated with underlying colorectal cancer. The mortality of the disease is low. The prognosis depends on the association with an underlying cancer.
A 62-year-old man had had an inflamed and eczema-like lesion in the right inguinal and scrotal regions since 2011. He had visited several dermatologists for 6 years. Antimicrobial, antifungal, and local treatments were not successful. In 2015, the disease invaded the left scrotal region. Because of the disease’s long-standing nature and resistance to treatment, a skin biopsy was performed in September 2017. The biopsy result was extramammary Paget’s disease. The laboratory, medical, urological, and radiological (chest X-ray, abdominal US, abdominal + pelvic MR/CT) examinations were negative. An uro-oncology and radiotherapy consultation suggested irradiation because of the tumour’s wide extension and its locations (Figures 1 A–C). Between October 30 and November 30, 2017 the patient received 20 × 2 Gy half-deep X-ray irradiations [13].
Macroscopic description: the histological sample was a 10 × 3 mm part of the skin with a 5 mm brownish and off-white papule on the surface.
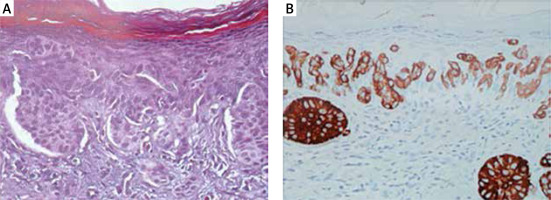
Microscopic description: the biopsy was taken from the lumbar lesion that had existed for 6 years. The surface of the biopsy was hyperkeratotic and covered by slightly expanded, multilayer keratinised epithelium [14, 15]. At the basal part of the epithelium, atypical cells with wide, pale cytoplasm were recognised in variable-sized nests (Figures 2 A, B). The nuclei were large and variable-sized with a loose chromatin structure and prominent nucleoli. Similar cells in smaller nests or individually infiltrating the full thickness of the epithelium were observed, and in some parts, the granular and keratinised layers were also affected. Similar cells either individually or in small groups were recognised in the epithelium of the skin tag, dermis, and deeper part of the reticular dermis. The lesion reached the edge of the biopsy excision. The immunohistochemical examination showed cytokeratin positivity and partial positivity for cytokeratin-7 protein. Regarding cytokeratin-20, the sample was negative [11, 15]. The sample was negative for oestrogen receptor, PSA, and S-100 protein.
Figure 2
Histopathologic examination. The thickness of the sample is 2 μm. A – Haematoxylin-eosin (HE) staining. B – Immunohistochemical (IH) reaction with cytokeratin-7 (CK7) positivity (CK+)
Diagnosis: extramammary Paget’s disease with dermal infiltration.
After completing radiotherapy, we followed up the patient every 3 months. After 1 year, in November 2018, all the above-mentioned examinations were performed again. The examinations did not show any tumour recurrences or metastases.
When chronic inflammation exists for several years, we should consider systemic diseases and malignant lesions. In many cases, histological examinations are needed for the correct diagnosis. EMPD is a complex disease, so interdisciplinary collaboration with several doctors is needed for a cure. Depending on the location of the disease, the therapist can be a dermatologist, general surgeon, plastic surgeon, colorectal surgeon, oncologist, urologist, or gynaecologist.









