Linear IgA bullous dermatosis (LABD) is a rare, acquired autoimmune disease which is characterized by itchy, clustered, subepidermal bullae with linear IgA deposits at the dermo-epidermal junction in direct immunofluorescence assay (DIF). In 1979, Chorzelski and Jabłońska distinguished LABD as a separate entity from bullous pemphigoid. Occurrence of LABD in Europe is around 0.2–0.5 cases for 1 million people per year [1, 2].
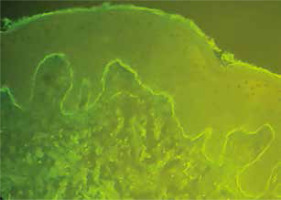
We present the case of a 41-year-old female, after a liver transplant due to autoimmune complications of hepatitis, in whom bullous lesions appeared. First skin lesions appeared as tiny, itchy papules, vesicles and bullae on the abdominal skin. Appearance of lesions was not accompanied by fever or prodromal symptoms. The patient claimed that she was not taking new medications or dietary supplements. At the beginning, varicella due to immunosuppression was suspected because the patient has taken tacrolimus for 7 years. Acyclovir was used orally with no result. After a week the patient was admitted to the Department of Dermatology at the University Hospital. Based on the clinical picture, LABD was suspected and diagnostic tests of autoimmune bullous disease were performed. Within 2 days after admittance, significant progression of skin lesions occurred. Multiple tense bullae developed on the trunk and the extremities, often in the form of a cluster of jewels (Figure 1). Additionally, new lesions appeared on the oral mucous membranes, scalp and skin around lips and ears. The first direct immunofluorescence (DIF) test of a biopsy from perilesional skin was negative. In a histological examination subepidermal blister associated with dermal infiltrate of neutrophils was revealed. In indirect immunofluorescence (IIF) there were no circulating antibodies IgG against desmoglein 1 and 3, and against antigen BP180. It was decided to perform another biopsy from the perilesional skin to the fresh bullae on the trunk in order to perform the second DIF. This DIF showed linear IgA deposits along the epidermal basement membrane which allowed for the final diagnosis of linear IgA bullous dermatosis (again there were no deposits of IgG and IgM antibodies as well as complement system components C1q and C3c) (Figure 2). It is interesting that the patient showed monomorphic blisters and bullae in the location of previous needle inserts and a previous scratch mark (Figure 3). The needle inserts were made 4 and 9 days prior to the appearance of lesions in order to take blood for laboratory tests. Orally administered dapsone, 100 mg/day, was started. Due the elevation of liver enzymes activity, after 7 days, the dosage was lowered to 50 mg/day and prednisone was added (30 mg/day). After 6 days of treatment no new lesions appeared and slow resolution of skin lesions was observed. The patient was discharged and after 2 months follow-up, full remission was observed.
The main etiological factor of LABD is circulating IgA antibodies reacting with 97 kDa protein of the BPAG2 fragment of lamina lucida. Multiple connections between the disease and administered drugs, infections, cancer or autoimmune diseases were pointed out [3]. There are only few LABD case descriptions in patients with immunosuppression after an organ transplant or autoimmune liver diseases [4–7]. In 1990, Petit et al. [4] described a case of a female patient, where LABD appeared 14 months after a heart transplant while taking prednisone, cyclosporine, allopurinol and dipyridamole. Schultewolter et al. [5] and Yhim et al. [6] reported patients after a bone marrow transplantation with LABD. In 2016, Bacharewicz-Szczerbicka et al. [7] described co-occurrence of linear IgA bullous dermatosis with primary biliary cholangitis. Koebner phenomenon is characterized by occurrence of monomorphic lesions on the areas of previous trauma within several days. The mechanism of this phenomenon has not been fully explained. There are 4 main categories of the Koebner phenomenon: true koebnerization, pseudo-koebnerization, occasional lesions, and questionable trauma-induced processes [8, 9]. In 2008, Rashid and Raza [10] described the case of a 30-year-old female patient with a drug-induced LABD, where bullae appeared in the areas of previous linear scratches of the trunk and the place of subcutaneous insulin injection. In 2010, McDonald et al. [11] described the case of a 32-year-old female patient with LABD, where Koebner phenomenon occurred at the sites of adhesive placement (the patient was treated at ICU due to a motor vehicle accident). In diagnostics of LABD the most important test is direct immunofluorescence which shows linear IgA deposits at the dermo-epidermal junction. Less often, one can show C3 complement system component deposits (in 50% of the cases) and additionally IgG antibodies (in 30% of the cases). Linear IgA deposits are the defining phenomenon for LABD and without it LABD is excluded. Deposits in dermo-epidermal junction are almost exclusively class IgA1 antibodies and are located mainly in the lamina lucida of the basement membrane [1, 2]. In the literature, only few cases of negative results of DIF tests in LABD were described. In 1992, Collier and Wojnarowska [12] published a paper, in which the DIF result from the volar forearm was negative in 2 out of 17 patients but in other localizations DIFs were positive. Due to this fact, the DIF test needs to be repeated, ideally on the skin from a different localization. In the literature there is also a case of a negative DIF result in the patient with vancomycin induced LABD, where second biopsy confirmed the diagnosis [13]. IgA circulating antibodies can be shown in low titres in almost 30% of adult patients. Using a skin split makes the technique more sensitive. In indirect immunofluorescent assay (IIF), class IgA antibodies against antigen 97 kDa/120 kDa, which is a fragment of BP180, or against type VII collagen are shown [1, 2]. Histological examination reveals subepidermal blisters associated with dermal infiltrate of neutrophils and low number of eosinophils, microabscesses in papillae. However, it is not pathognomonic and can be concurrent with other bullous diseases, e.g. pemphigoid group diseases [1]. It is necessary to remove the inducing drug, if it was identified. The first-line treatment of LABD is dapsone, usually 50–200 mg daily. It can be used in monotherapy as well as with other drugs. Dapsone effectiveness according to the literature data goes up to 45% in adults and 42% in adolescents with LABD. Second-line treatment option is systemic glucocorticosteroids which show less effectiveness here than in IgG-dependent bullous diseases like pemphigus or pemphigoid. Other drugs used in LABD treatment include: mycophenolate mofetil, intravenous immunoglobulins, colchicine, cyclosporine, tetracycline (as monotherapy or with nicotinamide), erythromycin, and biological drugs such as omalizumab or rituximab [3, 14, 15].