Introduction
Allergen-specific immunoglobulin E (sIgE) detection is the fundamental laboratory assessment used in allergy diagnosis. This test may be conducted in patients of any age and those with diminished skin reactivity; moreover – most importantly – it does not require discontinuation of anti-allergy treatment, including that with antihistamines. The currently used in vitro methods of measuring sIgE levels differ primarily in terms of the types of solid phases, coupled allergens, the limits of detection, the degree of automation, and the time it takes to obtain the result. From the perspective of laboratory testing, sIgE is an extraordinarily stable biomarker. Long-term storage, sometimes for up to several years, of frozen samples at –20°C does not affect test result reliability. Moreover, neither icteric, nor lipemic or haemolysed sera affect the quality of the results. IgE may be detected not only in blood serum but also in heparinized, citrated plasma (except EDTA). IgE may be also identified in bronchoalveolar and nasal lavage fluids [1, 2]. In the nasal mucosa sIgE plays a physiological function and mediates the presentation of CD23-dependent IgE allergens to B- and T-cells. Moreover, the inhibitory responses to nasal lavage fluid and serum observed in IgE-facilitated allergen binding (FAB) assays were shown to be related to the duration of subcutaneous immunotherapy (SCIT). A more pronounced inhibition of the allergen-IgE complex binding to B-cells was observed in the presence of the nasal lavage fluid, not serum, which is likely due to higher levels of sIgG4 antibodies and a high IgG4-to-IgE ratio [3]. The current approaches involve the use of natural allergen extracts, which poses two analytical problems. One problem is low test accuracy, which is due to poor standardization of the allergen extracts commonly used in diagnostics. These extracts may differ in terms of their allergen content, which is a result of the diversity of source materials from which they are obtained. The other problem is associated with the inability to differentiate between a primary allergy and immunologic cross-reactivity. The ability to make a distinction between these two mechanisms is important, because it is necessary to select the right allergen for specific immunotherapy. This is particularly important in potentially life-threatening allergies, such as those to insect venom. The limitations posed by such imperfections of natural allergen extracts make it difficult to interpret test results and thus make the subsequent therapeutic decisions [4]. These problems inspired the concept of using genetic engineering techniques to produce recombinant allergens or to obtain highly purified allergen components. This gave rise to developing molecular allergy diagnostics, which involves detecting IgE, which are specific to individual allergen components – which brings a new level of quality to allergy diagnostics.
Methods
The main purpose of this study was a review of the literature concerning the use of sIgE detection in the nasal lavage fluid, by searching through the PubMed, Medline, Scopus, and Google Scholar databases. We used five phrases/topics in our search: “local production of specific immunoglobulin E (sIgE)”, “sIgE in nasal lavage”, “evaluation for nasal sIgE”, “biomarkers for diagnosis of allergic rhinitis”, and “sIgE” with “nasal allergen provocation test”. Our PubMed database search returned 23 results in response to the query “local production of specific immunoglobulin E (sIgE)”, 18 of which met the thematic criteria; 15 results to “sIgE in nasal lavage”, 8 of which met the criteria; 54 results to “evaluation for nasal sIgE”, 21 of which met the criteria; 823 results to “biomarkers for diagnosis of allergic rhinitis”, 120 of which met the criteria, and 800 results to “sIgE and nasal allergen provocation test”, 157 of which met the thematic criteria. Our search of the Scopus database returned 38 articles containing the phrase “local production of specific immunoglobulin E (sIgE)”, 16 of which met our criteria; 17 articles in response to the “sIgE in nasal lavage” query, 12 of which met the criteria; 13 articles containing “evaluation for nasal sIgE”, 11 of which met the criteria; 152 articles containing “biomarkers for diagnosis of allergic rhinitis”, 125 of which met the criteria; and 58 articles containing “sIgE and nasal allergen provocation test”, 51 of which were acceptable in terms of the search parameters. Our analysis of Medline yielded 505 matches to “local production of specific immunoglobulin E (sIgE)”, 85 of which met our criteria; 69 articles containing “sIgE in nasal lavage”, 42 of which met the criteria; 603 matches to the “evaluation for nasal sIgE” query, 35 of which met the criteria; 43 matches to “biomarkers for diagnosis of allergic rhinitis”, 11 of which met the criteria; 87 matches to the terms “sIgE” and “nasal allergen provocation test”, 73 of which met the criteria. Our search of the Google Scholar database returned 33,800 matches to “local production of specific immunoglobulin E (sIgE)”, 158 of which met our search criteria; 2,180 articles with the term “sIgE in nasal lavage”, 120 of which met our criteria; 10,500 articles with the term “evaluation for nasal sIgE”, 105 of which met our criteria; 23,200 articles containing “biomarkers for diagnosis of allergic rhinitis”, 127 of which met the criteria; and 26,000 matches to the query “sIgE” and “nasal allergen provocation test”, 158 of which met the criteria of our search.
Results
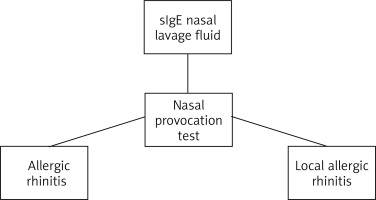
The analytical methods used in molecular techniques for allergy diagnostics are characterized by (1) high sensitivity (analytic sensitivity), particularly when important allergens are inadequately represented in, or entirely absent from, the extract; (2) high test selectivity (analytic specificity), which provides additional information on (a) the potential risk, (b) possible cross-reactivity, or (c) primary (species-specific) allergy. Nonetheless, the pertinent indications for testing for the IgE specific to individual allergen components can be established only based on individual patient characteristics (clinical presentation and past medical history, Figure 1) and the characteristics of the specific allergen (the source of the allergen and the individual allergen components that are available), but not in a standardized way [5]. There are also patients who – despite a past medical history positive for allergic conditions – do not have elevated serum sIgE levels [6]. A number of studies demonstrated the importance of localized immune responses rather than systemic immunity in the pathogenesis of allergic rhinitis. Indeed, B-cells expressing antigen-specific immunoglobulins can shift to expressing IgE in situ. However, the relative in situ contribution to the production of the IgE detected in the serum remains unclear. Yoshida et al. made quantitative assessments of local and systemic sIgE levels. That study was conducted in a group of 59 patients (aged 7–56 years) with seasonal allergic rhinitis induced by cedar pollen. These quantitative assessments of the IgE, IgA, and IgG specific to Japanese cedar pollen (JCP) were conducted in nasal lavage fluid (NLF) and serum with immunofluorescence assays. Nasal lavage fluid was collected following a modified Svensson’s protocol [7], which involves instilling 5 ml of isotonic saline solution (0–9%) into the right nostril with a pipette in a patient whose head is slightly tilted backward. The patient must maintain this position for several seconds without swallowing and then bend the head forward and let the nasal lavage fluid out into a collection vessel. The obtained nasal lavage fluid and serum samples were stored at –30°C until the time of their analysis. All samples were collected between 9:00 am and 11:30 am. The levels of sIgE in nasal lavage fluid from most patients were shown to be considerably higher (13.2-fold on average) than those in the serum, which was definitively consistent with a predominantly local (in situ) sIgE production and the subsequent dilution of the produced immunoglobulins in the circulation. Therefore, those authors confirmed local sIgE synthesis, which may encourage local allergy treatments and the use of nasal lavage fluid as a biological specimen for diagnosing allergic rhinitis [7].
The methods of obtaining nasal lavage fluid in order to determine sIgE levels require intranasal administration of a large volume of saline, which is quite problematic in children. Ahn et al. designed two methods (a spray method and a swab method), which are easy to use in paediatric patients [8]. The spray method involves slowly spraying 5 ml of isotonic saline in the form of a fine mist into each nostril with an electronic nasal spray device called New Coclean (WelbuTech, Incheon, Korea) and collecting the diluted nasal secretions. The swab method, on the other hand, involves inserting a cotton swab until resistance is met at the turbinates, then rotating the swab several times against the nasal wall, and finally washing the cotton swab tip with 1.25 ml of isotonic saline in a test tube. The nasal fluid samples obtained in one of these ways and serum samples were analysed for IgE specific for Dermatophagoides farinae, Dermatophagoides pteronyssinus, Alternaria tenuis, birch, and weed mix. The study involved 82 paediatric patients with rhinitis symptoms. The spray method was used in 30 patients, and the swab method in 52 patients. Antigen-specific IgE were detected via an ImmunoCAP radioallergosorbent technique (Uni-CAP; Pharmacia, Uppsala, Sweden). The obtained results showed 30 patients with nasal sIgE levels of ≥ 0.35 kIU/l. There was a positive correlation between nasal-specific IgE and serum-specific IgE to Dermatophagoides farinae and Dermatophagoides pteronyssinus (r = 0.548, p < 0.001; r = 0.656, p < 0.001). Based on the positivity of skin prick test results for the individual allergens, the authors established the cutoff point of nasal-specific IgE to Dermatophagoides farinae at 0.11 kIU/l and to Dermatophagoides pteronyssinus at 0.12 kIU/l. Based on these cutoff points, five of the evaluated patients were diagnosed with local allergic rhinitis (LAR). Moreover, both the spray method and the swab method showed a relatively high positivity for nasal-specific IgE, which was also reflected by the IgE levels in the serum. Therefore, the authors concluded that these methods of nasal secretion collection can be considered in diagnosing LAR in children [8]. A similar conclusion was reported by Colavita et al., who assessed IgE in nasal lavage fluid as a biomarker of LAR in children [9]. A total of 54 paediatric patients aged between 4 and 12 years were included in the study and divided into three groups: a study group of 26 children with symptomatic rhinitis but no evidence of systemic atopy; an allergic rhinitis group of 15 children; and a control group of 13 healthy children. Each child underwent nasal lavage with the use of 2 ml of physiological saline per nostril. IgE levels in nasal lavage fluid were measured with the ImmunoCAP technique. The results showed higher IgE levels in the nasal lavage fluid samples (mean: 6.005 UI/ml; range: 4.47–7.74 UI/ml) from 16 out of the 26 patients from the study group, who could ultimately be diagnosed with LAR. Moreover, the authors reported a significant difference (p < 0.0001) between both the non-allergic rhinitis and LAR groups and the control group, which helped establish the cutoff point at 3.85 UI/ml. The authors achieved better responses to an earlier allergic rhinitis therapy in the LAR group than in the children with non-allergic rhinitis. Thus, the study by Colavita et al. indicates that a high proportion of the paediatric patients who are initially classified as part of the non-allergic rhinitis population, in fact have LAR. As a consequence, nasal lavage fluid IgE levels can be considered as a method of diagnosing LAR in children that is both easy and rapid. Moreover, patients diagnosed with LAR show a better response to classic allergic rhinitis treatment [9].
Completely opposite results and conclusions were reported by Eckrich et al., whose studies assessed the rates of a potential “local allergic rhinitis” in patients with non-allergic rhinitis from a non-selected group of young adults. A total of 131 students (aged 25.0 ±5.1 years) with a possible allergic rhinitis formed the study group and 25 healthy individuals (aged 22.0 ±2.0 years) with ruled out symptoms of allergic rhinitis formed the control group. Ninety-seven out of the 131 students from the study group were found to have a positive result (≥ 3 mm) of a skin prick test with house dust mite allergens. Both groups also underwent a nasal provocation test with house dust mite allergens. The authors reported that total IgE and house dust mite-specific IgE levels obtained in the serum and in nasal secretions differed significantly between the individuals who tested positive for house dust mite allergens and those from the control group. However, there were no quantifiable differences between non-allergic and control individuals. Neither the nasal provocation test nor nasal-specific IgE to dust mite allergens showed a quantifiable positive response in any of the non-allergic rhinitis or healthy individuals, whereas 13 individuals with a house-dust-mite allergy tested positive. Based on their results, the authors concluded that nasal IgE is present in individuals with an allergy to house dust mites but not in individuals with non-allergic rhinitis. According to the authors, the study population of non-selected individuals showed no exclusively local IgE synthesis. Therefore, the results of their study undermine the emerging concept of LAR [10].
As part of our search through the relevant literature we also focused on assessing the specificity and sensitivity of this technique [11]. Berings et al. evaluated house dust mite-specific IgE levels with an ImmunoCAP assay in a group of 30 adult patients with allergic rhinitis to this allergen (confirmed by a serological test) and 29 individuals in the control group. The authors showed that the specificity of sIgE detection in nasal lavage fluid was 100%, whereas the sensitivity of this test was 70% with respect to the results obtained with blood serum [12]. A somewhat lower sensitivity (of 40%) was reported by Castelli et al. in their 2019 study conducted in 161 individuals with seasonal allergic rhinitis, whereas the specificity was found to be comparable with that reported by Berings (in comparison to IgE levels in blood serum). The authors concluded that the measurement of sIgE in nasal lavage fluid reflects the patients’ systemic allergy profiles and helps predict (with a high degree of probability) the presence of these immunoglobulins in blood serum. Nonetheless, the authors pointed out that the low sensitivity of this method requires high analytical sensitivity and a suitable method of obtaining the samples (so that they are diluted as little as possible) in order for this procedure to become an alternative to measuring sIgE levels in the serum [13].
In 2019, Meng et al. proposed a hypothesis that local sIgE levels measured in nasal secretions may be used instead of nasal allergen provocation testing. A total of 212 patients with symptoms of rhinitis (nasal congestion, nasal discharge, sneezing, and itching) were screened, with 73 patients eventually recruited. These patients were characterized by the presence of eosinophils in nasal secretions and negative serum sIgE test result. A group of 10 healthy individuals served as controls. UniCAP (Uppsala, Sweden) helped detect sIgE in the nasal secretions of 14 out of the 73 individuals, whereas the nasal allergen provocation test was positive in 12 of the 14 individuals, thus confirming their diagnosis of LAR. As many as 11 individuals out of those who tested positive in a nasal allergen provocation test tested positive for sIgE in their nasal secretions. That study demonstrated both high sensitivity (91.7%) and specificity (95.1%) and a high positive predictive value and negative predictive value of the results at 78.6% and 98.3%, respectively. The diagnostic accuracy of sIgE measurements in nasal secretions in this group of patients was 94.5%. These results supported the initial hypothesis that measuring local sIgE levels may replace nasal allergen provocation testing as a tool in diagnosing LAR. However, the authors emphasized that this should be confirmed in studies involving larger patient populations [14]. Ryabowa et al. attempted to assess the role of secretory IgE in the differential diagnosis of rhinitis in pregnant women. The study included 97 pregnant women with symptoms of rhinitis, out of whom 37 had already been diagnosed with allergic rhinitis (group I), 30 were suspected of allergic rhinitis (group II), and 30 had pregnancy rhinitis. The control group comprised 23 healthy pregnant women with no symptoms of this condition. IgE levels in nasal secretions were 2.9 ±0.7 kE/l in group I and 5.5 ±2.6 kE/L in group II, which exceeded the levels measured in the control group (1.2 ±0.6 kE/l; p < 0.05). IgE levels in nasal secretions in the pregnancy rhinitis group did not differ significantly from those in the control group (1.9 ±0.3 and 1.2 ±0.6 kE/l, respectively; p < 0.05). This study showed that measuring IgE levels in nasal secretions can be useful in differential diagnosis of rhinitis in pregnant women [15].
Molecular diagnostic techniques became an important milestone in allergy diagnosis, since they allow for determining the serum levels of sIgE against individual allergen proteins. Some of these proteins may be poorly represented in or even completely absent from allergen extracts, for instance due to their destruction during processing the allergen for testing. Therefore, despite a clinically apparent allergy to a given allergen protein, the fact that this protein is insufficiently represented in the test extract may cause some patients to test negative both in serum tests and skin prick tests. This problem has been observed for many inhaled allergens, for example via nasal allergen provocation testing, which showed that the patients allergic to a very small (9 kDa) molecule (Der p 23) may fail to be diagnosed with either sIgE detection or skin prick testing. There is a similar problem in the case of food allergens, such as the water-insoluble proteins called oleosins. The hydrophobic nature of these molecules is the reason why they are underrepresented in the aqueous extracts used for skin prick testing or sIgE level detection. This fact was unknown until relatively recently, hence we can literally witness the way molecular techniques are revolutionizing the diagnosis of allergic conditions. Moreover, it has now become possible to analyse several hundred molecules simultaneously, even with small serum sample volumes [16]. The first of such tests was the ImmunoCAP Immuno-Solid-phase Allergen Chip (ISAC) microarray, which was developed and introduced by VBC Genomics from Vienna in 2001, and from the year 2009 onward, was developed, manufactured, and distributed by Phadia, Thermo Fisher Scientific, Uppsala, Sweden [17]. Recent years saw the emergence of tests assessing sIgE with the use of nanotechnology; these include the ALEX text (Macro Array Diagnostics, Vienna, Austria) that helps detect sIgE with the use of considerably lower amounts of the allergen. While the established microarray techniques require approximately 100 picograms (picogram = 0.000000001 mg) of the evaluated allergen, the new nanotechnology-based tests work with the amounts that are 100–1,000 times smaller [18, 19]. The ImmunoCAP ISAC test, which is semiquantitative and based on microarray technology, could analyse anywhere from 29 to 112 molecules derived from 51 allergen sources. Testing requires a 30 μl sample of serum, plasma, or capillary blood. The material is transferred onto a glass plate with areas of immobilized allergens dedicated for 4 patients. Therefore, it is optimal to test 4 serum samples at a time. The results are obtained after approximately 4 h. The limit of detection is 0.3 ISAC standardized units for specific IgE (ISU-E) [20, 21]. ALEX (Allergy explorer) is a quantitative multiplex test based on nanotechnology. First marketed in 2017, it measured sIgE against 126 allergen molecules and 156 allergen extracts. Test composition evolved in 2019, with the new version – ALEX2 – capable of measuring total IgE and sIgE against 178 allergen molecules and 117 allergen extracts (from inhaled and food allergens). ALEX2 is a quantitative test for the measurement of sIgE and a semiquantitative test for the measurement of total IgE. Testing requires a 100 μl sample of serum or plasma (except EDTA plasma). Results are obtained within approximately 3.5 h [20]. The limit of detection is 0.1 kUA/l for sIgE and 1 kU/l for total IgE [22]. Both tests have been repeatedly studied to assess their sensitivity and specificity for sIgE in blood serum. These studies demonstrated that both the sensitivity and specificity of these tests are greater than those achieved via determining sIgE levels with the use of allergen extracts. This is because these new tests can measure sIgE against proteins that may be completely absent from the extract or present in quantities insufficient to yield a positive result, while in many cases actually being the cause of the patient’s symptoms. In light of the fact that molecular diagnostics dramatically improves the diagnostic value of sIgE serum levels, questions arise whether these modern tests can be used to measure sIgE levels in nasal secretions and whether these tests can be more useful than the methods of measuring sIgE in nasal secretions with the use of allergen extracts and nasal allergen provocation testing. Berings et al. attempted to answer these questions in their study from 2017. They analysed the presence of sIgE against 15 house dust mite molecules, including 13 Dermatophagoides pteronyssinus molecules, i.e. nDer p 1, rDer p 2, rDer p 4, rDer p 5, rDer p 7, rDer p 10, rDer p 11, rDer p 14, rDer p 15, rDer p 18, rDer p 21, rDer p 23, clone 16, and 2 Dermatophagoides farinae molecules, i.e. nDer f 1 and rDer f 2 with the use of ImmunoCAP ISAC (cutoff ≥ 0.10 IU/ml). Those authors demonstrated that the presence of nasal sIgE against at least one of the major house-dust-mite-allergen molecules (nDer p 1, nDer f 1, rDer p 2, rDer f 2, rDer p23) helped predict both the patient’s allergic status and blood serum sIgE levels with a high sensitivity and specificity (90% and 100%, respectively). The sensitivity of measuring the levels of sIgE against molecules (when at least one of those molecules was positive) was greater than that achieved with an allergen extract (90% vs. 70%, respectively), whereas the specificity was 100% for each of the two evaluated nasal secretion collection techniques [12]. A 2020 study by Gökkaya et al. involved measurements of nasal secretion and blood serum sIgE levels against the following allergens: Ara h 8 (peanut), Act d 8 (kiwi), Aln g 1 (European alder), Bet v 1 (birch), Cor a 1.0101 (hazel pollen), Cor a 1.0401 (hazelnut), Mal d 1 (apple), Pru p 1 (peach), Cyn d 1 (Bermuda grass), Phl p 1, Phl p 2, Phl p 5, Phl p 6 (Timothy grass), Der f 1, Der f 2 (D. farinae), Der p 1, Der p 2 (D. pteronyssinus) with the ImmunoCap ISAC test in a group of 47 subjects allergic to one or more of those aeroallergens and in 2 non-sensitized control subjects. The authors demonstrated a specificity comparable to, and a sensitivity higher than, that of the ImmunoCap ISAC test for the measurements conducted in the serum than in those conducted in nasal lavage fluid (0.95 vs. 0.96; 0.94 vs. 0.85, respectively). The positive predictive value of nasal sIgE was 0.97 and that of serum sIgE was 0.96, whereas the negative predictive values were 0.82 and 0.92, respectively. As a possible cause of this lower sensitivity, the authors suggested the lack of manufacturers’ instructions in terms of the optimal use of microarrays for nasal secretion specimens [23].
Measurements of sIgE in nasal lavage fluid may, possibly, be used in diagnosing allergic rhinitis. However, currently there is no standardization of nasal secretion collection methods or the methods of validating sIgE measurement results from this type of specimen [24]. Although allergen extract-based sIgE measurements have demonstrated a high specificity, their sensitivity has varied (22–70%) depending on the method of collecting nasal secretions [12, 25]. The nasal secretion sIgE measurement techniques that use allergen molecules increase test sensitivity up to 90% [25]. Local nasal secretion sIgE measurement techniques that use allergen extracts seem to be a reliable and clinically effective tool for diagnosing LAR. Nonetheless, the number of studies assessing nasal secretion sIgE against allergen molecules is still too low, and the findings of these few studies require further confirmation in much larger cohorts, multicentre studies, and diverse populations. Therefore, the nearest future is likely to bring many new reports on this topic and will, perhaps, revolutionize LAR diagnostics. As studies with serum sIgE have shown, the modern tests for detecting this type of immunoglobulins against several hundred allergen molecules simultaneously have altered the nature of allergy diagnostics. This is in part due to their shorter time to establishing the diagnosis and also their helping us better understand many allergy-related phenomena that had been observed but remained unexplained. Thus, molecular diagnostics offers vast new possibilities in diagnosing allergic conditions, including allergic rhinitis. The search for local sIgE production is not limited only to analysing nasal secretions, though. Microarray technology has been also used in attempts to measure sIgE levels in tears. Such attempts were reported, for example, by Leonardi et al., whose study was conducted in 10 individuals with active vernal keratoconjunctivitis (VKC) and 10 healthy individuals comprising the control group. Those authors successfully detected sIgE in the serum and/or tears of 6 patients with VKC with the use of the ImmunoCAP test. Three of these 6 individuals had only tear sIgE against the allergens of grasses, trees, dust mites, animals, and foods. The conjunctival allergen provocation test conducted outside the exposure period confirmed a local specific conjunctival reactivity. No IgE was detected in the control group in either of the tested sample types. The presence of sIgE only in the tears of patients who exhibited exclusively ocular symptoms supports the hypothesis of the existence of local allergies [26]. The use of microarray technology in measuring sIgE levels in specimens other than serum may lead to new possibilities and new directions of research. The need to use additional diagnostic methods is due to the fact that allergic rhinitis may be present in individuals without systemic atopy. In such cases, the diagnosis is possible only via nasal allergen provocation testing. However, measuring sIgE levels in nasal secretions or tears thus far remains confined exclusively to research, not having reached the level of clinical application [27].
Conclusions
Undoubtedly, measuring sIgE in nasal lavage fluid plays an important role in the differential diagnosis of allergic rhinitis. The prospect of further studies in the field of standardization and gaining a deeper understanding of that which is still unknown through the use of molecular diagnostics fills us with optimism.