INTRODUCTION
Rhinophyma is a progressive and disfiguring condition of the nose, characterized by the enlargement of sebaceous glands and the proliferation of blood vessels and connective tissue [1]. It is commonly associated with chronic rosacea and has historically been regarded as the advanced or end stage of this condition, although its precise pathogenesis remains unclear [2].
The disorder primarily affects the lower two-thirds of the nose, though similar changes can sometimes involve the chin (gnathophyma), forehead (metophyma), or ears (otophyma) [1]. Clinically, rhinophyma presents as a painless hypertrophy of the distal nose, leading to significant nasal deformity. This condition can have a profound impact on both physical appearance and quality of life [2]. Many individuals with rosacea lose self-confidence and feel embarrassed in social or work situations. Many individuals with rosacea experience a loss of self-confidence and feel uncomfortable in social or professional settings. For patients with rhinophyma, the appearance of the nose adversely affects their daily functioning and participation in social life.
CASE REPORT
A 66-year-old patient presented with concerns about the unsightly appearance of his nose and reported a 4-year history of a progressively enlarging mass on the nasal area. The lesions initially appeared as a small nodule on the tip of the nose and gradually extended to involve the entire nose, resulting in significant cosmetic disfigurement and psychological distress. The patient reported no nasal obstruction or dyspnoea and denied any history of trauma, physical manipulation, prior use of topical medications or previous occurrences of similar lesions.
Visible changes consistent with rosacea were noted on the forehead, with less pronounced involvement of the cheeks and chin (fig. 1).
Figure 1
Images of the patient’s condition before CO2 laser therapy: A – front view; B – bottom view; C, D – right side view; E, F – left side view
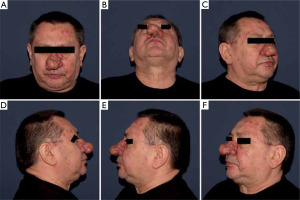
Clinical examination revealed a soft, lobulated, skin-coloured nodule on the nasal tip, accompanied by thickened skin and irregular surface nodularities across the rest of the nose. The lesions consisted of transient facial redness and papules, accompanied by telangiectasias and pustules on the forehead and cheeks. They were non-pruritic and showed no signs of malignant transformation. Based on the clinical findings, a diagnosis of rhinophyma associated with rosacea was made.
The patient underwent treatment using an Ultra Plus CO2 laser with a PreciseFX 2.0mm tip with a wavelength of 10,600 nm (constant pulse, defocusing mode with multiple passes, laser frequency: 150 Hz and power: 15 Watts) under local anaesthesia with 2% lignocaine hydrochloride. The end-point for adequate ablation is the visible expression of the contents of the dilated glands. The treatment consisted of two sessions, spaced 4 weeks apart. Post-treatment, mild local pain, swelling, redness and oozing were observed, which resolved within 7 days (fig. 2).
Figure 2
Post-procedure reaction occurring at the site treated with the laser: swelling, redness, oozing, and tissue charring were observed. A – Front view; B – bottom view; C, D – right side view; E, F – left side view
Following each session, a close dressing was applied to the affected area after using argosulfan cream, which was removed after 24 hours. Oral analgesics were prescribed for seven days on an as-needed basis and argosulfan 1% cream was recommended topically for 8–10 days. Normal nasal appearance without nodules was achieved within seven days post-treatment.
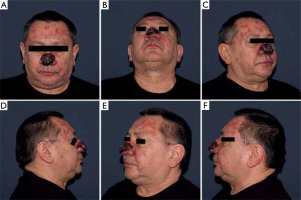
After completing laser therapy, oral isotretinoin at a dose of 10 mg/day was initiated for a specified period. The final effect after completed laser therapy and isotretinoin treatment is shown in figure 3.
Figure 3
The final effect after completed laser therapy and isotretinoin treatment. A – Front view; B – bottom view; C, D – right side view; E, F – left side view

During a 1-year follow-up, no recurrence of the lesions was observed.
DISCUSSION
Rosacea is a chronic inflammatory skin condition that predominantly affects the central facial region. The most commonly involved areas are the skin of the cheeks, chin, nose, and forehead [3]. The primary symptoms include erythema, flushing, telangiectasia, phymatous changes, and inflammatory papules and pustules. Rosacea can also involve the eyes, leading to conditions such as blepharitis, conjunctivitis, keratitis, or lid margin telangiectasia. The global prevalence of rosacea is estimated at approximately 5.5% in the adult population. Women are slightly more affected than men, with an incidence rate of 5.41 per 100 women compared to 3.90 per 100 men [4]. Rosacea occurs most frequently in individuals of Caucasian descent; however, its prevalence in Asian and African populations may be underestimated due to the difficulty in identifying features like erythema and telangiectasia, which are less noticeable on darker skin tones [5].
In cases of prolonged disease, yellow-orange plaques known as phymas may form as a result of sebaceous gland hyperplasia, with the nose (rhinophyma) being the most commonly affected site [6]. Early stages of phymatous rosacea are characterized by enlarged follicular pores or dilated follicles accompanied by mild swelling. In advanced stages, the condition progresses to marked thickening of hyperaemic skin, irregular nodular surfaces caused by sebaceous gland hypertrophy, and eventual deformation of the nasal surface structure [7]. This manifestation is significantly more common in men, occurring 5 to 30 times more frequently than in women [8].
Rhinophyma has been categorized into four distinct variants – glandular, fibrous, fibroangiomatous and actinic [9].
The precise pathogenesis of rosacea and rhinophyma remains unclear, but it is believed to result from a combination of various factors that contribute to vascular alterations and activation of the innate immune system. Research has demonstrated an elevation in numerous vascular growth factors and receptors in affected skin, leading to abnormal vascular reactivity. Notably, levels of vascular endothelial growth factor (VEGF), VEGF receptors, the lymphatic endothelium marker D2-40, and CD31 expression are increased, promoting the proliferation of vascular and lymphatic endothelial cells [10].
The primary treatment options for papulopustular rosacea currently include topical agents such as azelaic acid and ivermectin, as well as oral medications like metronidazole, doxycycline, tamoxifen, and isotretinoin [11, 12]. Inflamed rhinophyma is typically managed with oral doxycycline or isotretinoin (13-cisretinoic acid), while topical treatments are generally not advised. Isotretinoin has been shown to effectively improve rhinophyma; however, disease recurrence within a year is possible [11, 12].
Due to the limited efficacy of oral treatments for rhinophyma and the low likelihood of spontaneous remission, surgery remains the primary treatment approach. The main reasons for surgical intervention are to improve aesthetic appearance and address secondary nasal airway obstruction. Several surgical techniques are available, including dermabrasion, electrocautery, electrosurgery/radiofrequency, cryosurgery, cold knife excision, the Shaw scalpel, and the subunit method, which is specifically used for severe cases [13]. The carbon dioxide laser is particularly beneficial, offering precise tissue removal, controlled bleeding, and a nearly bloodless surgical field [14, 15]. One notable advantage is its ability to penetrate deeply through the epidermis and superficial dermis; however, this can lead to thermal damage to the underlying dermis and adnexal structures. The procedure is more costly, takes longer to perform compared to techniques like scalpel excision or electrosurgery, and does not allow for the collection of specimens for histopathological analysis [13]. The selection of treatments seems to depend more on the preferences and expertise of the surgeon or practitioner rather than the severity of the disease.
This case report provides valuable educational insight into the multidisciplinary management of advanced rhinophyma, combining laser ablation with systemic isotretinoin therapy. The presented approach demonstrates how CO2 laser treatment followed by oral isotretinoin can achieve excellent cosmetic outcomes with minimal downtime and without recurrence after one year. This case highlights a structured, well-tolerated treatment plan that may be especially beneficial for patients who refuse or are not candidates for more invasive surgical options.
What makes this case unique is the use of a dualmodality protocol – CO2 laser followed by low-dose isotretinoin – in a patient with disfiguring but nonobstructive rhinophyma. The addition of isotretinoin as a post-laser maintenance strategy may contribute to long-term stabilization and prevention of recurrence, a concept that remains underrepresented in the literature. Moreover, the detailed laser settings and post-procedural care protocol provide practical guidance that can be replicated by clinicians managing similar patients.
CONCLUSIONS
Rhinophyma management is challenging due to its varying severity and the numerous treatment options available. Treatment methods range from minimally invasive to more aggressive, with their effectiveness depending on the disease’s severity and treatment objectives. Common approaches include excisional and laser techniques. The subunit surgical method is typically reserved for the most severe cases, which involve functional nasal issues, and it helps improve both support and structure. CO2 laser therapy, performed by an experienced doctor, yields significant and lasting results in a relatively short period of time. By documenting the specific laser parameters, post-treatment regimen, and long-term follow-up results, this report may serve as a reference for practitioners seeking evidence-based, patient-centred approaches to managing severe rhinophyma with both functional and aesthetic considerations in mind.








