Introduction
Acne is a common chronic inflammatory disease of the pilosebaceous unit [1]. It predominantly affects adolescents and young adults, however it may also occur in adults [2]. The prevalence of acne varies between studies; acne has been reported in up to 90% of adolescents [2–4]. This makes acne the most frequent skin disease in this age group. Although more than 80% of adolescents consider acne as an unavailable part of their childhood [5], acne is associated with significant physical and psychosocial morbidity [6]. Acne can have a negative impact on patients’ mood, self-esteem and quality of life (QoL) [7, 8]. Most probably the severity of acne may influence the psychosocial status of patients, however the studies dealing with this topic are limited [9]. Facial acne is the most common clinical manifestation of the disease [1]. This is due to more numerous and larger sebaceous glands in the face in comparison with other regions of the skin. Face, which is the first recognized area in interactions with other people is considered crucial for the psychosocial effect of acne [10].
Aim
This study was undertaken to assess the prevalence of facial acne among adolescents and to evaluate how acne of different clinical severity influences QoL in this age group.
Material and methods
Study design, participants and assessments
This cross-sectional study was performed in two randomly selected high schools in Wroclaw (the city located in south-west Poland with a population of almost 650 000 inhabitants) and in one school in Sieradz (a smaller town of central Poland with a population of nearly 43 000 inhabitants). The representative sample size for high school students in Poland was calculated as 384 (95% confidence interval with a margin error of 5%).
The study was approved by the Ethics Committee of the Wroclaw Medical University (KB-750/2021). The directors of all the included schools, after detailed explanation of the study purpose, gave their consent to run the project at their schools. The participation in the study was voluntary. All adult students gave their agreement to be included in the project. The students under the age of 18 years were taken into consideration only if they parents gave the written consent to include them in the study. Data were collected during the classes followed by detailed explanation by one of the investigators. All data were collected between 10th September and 10th November 2021.
All students were asked to fill in the questionnaire with the demographic details. They were also asked several questions related to their acne itself and the presence of acne lesions at the time of filling the questionnaire as well as in the past, presence of acne in siblings, past and current acne treatment as well as chronic comorbidities. Additionally, all participants assessed the severity of their facial acne using the provided standardized photographs [11] according to the Investigator’s Global Assessment (IGA) [12]. The scale included 5 illustrations with no acne (normal skin), minimal acne (almost clear skin), mild acne, moderate acne and severe acne [11]. Moreover, subjects who reported acne filled in the validated Polish language version of Dermatology Life Quality Index (DLQI) [13]. DLQI is a simple, dermatology-specific instrument widely used to evaluate the quality of life in various dermatoses. It is a 10-item questionnaire, the participant grades his/her answer on a 4-point scale (0 – not all, 3 – very much). The maximal number of points is 30; the higher number indicates greater QoL impairment [14]. The cut-off points for the DLQI were proposed as follows: 0–1 point - no effect at all, 2–5 points – small effect, 6–10 points – moderate effect, 11–20 points – very large effect and 21–30 points - extremely large effect [15].
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics v. 26 (SPSS INC., Chicago, IL, USA) software. Parametric and nonparametric distribution of the data was considered. The minimum, maximum, mean, and standard deviation were calculated. The Mann-Whitney U test, the χ2 test and Spearman’s correlation test were used where appropriate. All analyses were performed as two-sided tests; p-values less than 0.05 were considered significant.
Results
Out of 738 students who were asked to participate in the study, 730 completed the study questionnaires (98.9% response rate). There were 446 (61.1%) girls and 284 (38.9%) boys. Their mean age of the study group was 17.05 ±1.18 years (age range: 15–19 years) with no difference between girls and boys (Table 1).
Table 1
Group characteristics
Acne, based on the evaluation of photographs provided, was reported by 547 (74.9%) respondents. Interestingly, 71 subjects of all acne group (13.0%), marking the photograph with minimal acne (almost clear skin), did not consider that they suffered from acne. There was no significant difference in acne prevalence in females (75.1%) and males (74.6%). Five hundred and eleven (70.0%) students declared presence of acne lesions also in the past (Table 1). Acne was found in 58.5% of participants’ siblings. 37.5% of acne subjects were currently on anti-acne therapy, the acne treatment was administered to 62.5% of students in the past. No significant differences in the above-mentioned parameters were found between girls and boys (Table 1). One hundred and fourteen subjects with acne (16.3%) reported chronic comorbidities with a significantly higher prevalence (p < 0.046) in females (21.4%) than males (9.5%).
The majority of subjects – 323 (59.1%) students assessed their acne as minimal one (almost clear skin). Mild acne was demonstrated in 31.8% and moderate acne in 7.3% of the studied acne group. Only 1.8% of students considered their acne as severe one. Although there was a visible trend for the higher prevalence of mild acne in females (34.6% vs. 27.4%) and for more common severe acne in males (2.8% vs. 1.2%), the significant difference in acne severity between both gender groups was not found (Table 2).
Table 2
Acne severity among high school students
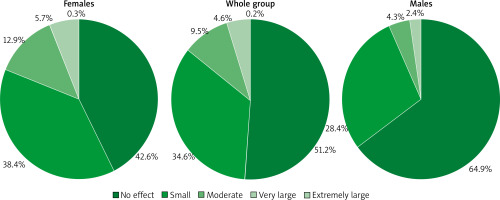
The mean DLQI scores in the acne group were calculated as 2.8 ±3.6 points, indicating a small effect of acne on subjects’ QoL. Females reported significantly higher QoL impairment than males (3.17 ±3.74 and 1.76 ±2.69 points, respectively). Considering the cut-off points for the DLQI scores it appeared that acne impaired QoL in 48.8% of students, in the remaining ones (51.2%) acne did not influence their well-being. Among the whole acne subjects 34.6% reported a small effect of their acne on QoL impairment, followed by a moderate effect (9.5%) and a very large effect (4.6%). Only 0.2% of students indicated that acne had an extremely large effect limiting their QoL (Figure 1). The gender difference was also seen when the degree of QoL impairment was analysed. More females than males reported small effects on QoL (38.4% and 28.4%, respectively; p = 0.02) as well as a moderate effect (12.9% and 4.3%, respectively; p < 0.001). In contrast, more males stated that acne did not influence their QoL at all (64.9% and 42.6%, respectively; p < 0.001) (Figure 1).
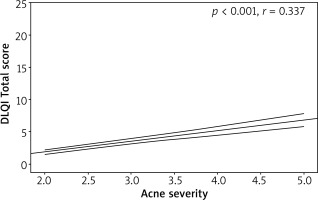
Acne severity markedly influenced QoL. The mean DLQI scores for the acne severity groups were as follows: minimal acne – 1.8 ±2.56 points, mild acne – 3.43 ±3.75 points, moderate acne – 5.05 ±5.33 points and severe acne – 6.67 ±5.52 points (Table 3). This means that only in patients with severe acne, the face skin lesions had a moderate effect on students’ QoL impairment, in remaining ones with minimal to moderate acne this influence was assessed as small. The gender difference was noticed in QoL assessment for the acne severity groups. Females scored significantly higher than males in DLQI when having minimal acne (p = 0.001), mild acne (p < 0.010) and moderate acne (p = 0.004). Only in the group with severe acne there was no significant difference between females and males in DLQI scores (Table 3). Moreover, the significant positive correlation between QoL impairment and acne severity was demonstrated (r = 0.337, p < 0.001) (Figure 2). This significant relationship was documented both in females (r = 0.382, p < 0.001) and males (r = 0.247, p < 0.001).
Table 3
DLQI total score (mean ± SD) according to acne severity
Discussion
Acne is regarded as very common skin disease [2, 4]. It can cause severe repercussion on self-esteem and quality of life [7, 8]. In our study, involving 730 students, aged 15–19 years, from three selected high schools in Poland, we measured prevalence, severity, and quality of life of self-reported facial acne. Almost 75% of students suffered from acne. This percentage considers females as well as males in between whom there was no significant difference in acne prevalence (females 75.1%; males 74.6%). Several previous studies indicated different acne frequency among adolescents. White et al. [16] showed that 85% of people aged 12–24 years presented with acne. However, recent research conducted in 7 European countries reported a prevalence of acne in approximately 58% of adolescents and young people [3, 17]. In Australia, a huge number of respondents among 16–18-year-olds – 93.3% reported presence of acne [18]. In contrast, the overall prevalence of acne in middle schools in Arar city in Saudi Arabia was only 14.3% [19]. In China, approximately 47% of 19-year-olds suffered from this disease [20], whereas a study carried out in Nottingham, UK, demonstrated acne in 50% of examined adolescents [9]. This is consistent with the results from other survey run on 500 students from four randomly selected public secondary schools in Podgorica, Montenegro, which showed that 49.8% of them had acne [8]. The differences between the above-mentioned studies might by related to variation of examined ethnic groups, as well as could be due to different methodology employed to diagnose acne. The majority of studies were based on acne self-reported surveys [1] as our study was, however in some projects the diagnosis was confirmed by physicians [9]. As mentioned above, we have not managed to demonstrate any difference in acne prevalence between females and males. This is in agreement with previously published data demonstrating a similar percentage of acne patients in both genders [3, 18, 19].
It is of interest that the majority of our students had minimal and mild acne, only slightly less than 10% self-reported moderate to severe acne. Most probably this is the reason that some of them did not even consider themselves as acne patients. The community-based study performed in the UK showed similar results [9]. They found only 11% of adolescents with moderate to severe acne, the remaining ones suffering from mild disease. However, the others noted a much higher percentage of more severe disease; 55% of their facial acne patients had moderate to severe disease [1]. The severity of acne seems to be similar in both genders. We, as others [1, 20, 21], were not able to see the difference in acne severity between female and male subjects. In the current project we also concentrated on the assessment of QoL among the group of students suffering from acne. Our study showed that 48.8% of them reported affection of their well-being due to this condition. The mean DLQI score in this group was 2.8 ±3.6 points, indicating a mild decrease in QoL. The impairment was significantly higher in females than in males (3.17 ±3.74 and 1.76 ±2.69 points, respectively). Slightly higher scores were obtained by Alsulaimani et al. [12] who showed, on the group of young adults, mean DLQI of 3.78 points. Japanese investigators revealed the mean DLQI score of 3.99 points among the group consisting of Japanese students from the elementary school through university [22], while in a study by Finlay and Khan [14], DLQI scored 4.3 points among acne patients. The above-mentioned data were more or less consistent with those obtained by our group. However, some research demonstrated bigger QoL impairment in their cohorts of acne subjects. In the study by Alanazi et al. [19] performed on female secondary school students in three randomly selected schools, in Arar city (Saudi Arabia), the mean DLQI was assessed as 5.26 points [19], while the Iranian study showed DLQI of 6.42 points [23]. On the other hand, an international team focused their study on a group of patients with more severe acne and showed mean DLQI score of 10.78 points, suggesting at least a moderate effect of acne on QoL [1]. The differences in DLQI scores among acne subjects are most probably related to different severity of acne in various studied groups. In our study demonstrating a small acne effect on QoL, the vast majority of students suffered from minimal and mild acne (90.9%), while in the group analysed by Tan et al. [1], more than a half of subjects were diagnosed with moderate to severe acne. The relationship between acne severity and degree of QoL impairment was also confirmed in the current study showing the significant positive correlation between the DLQI scores and acne severity. The same relationships were found among Indian and Pakistani acne patients [7, 21]. Our acne female subjects showed greater QoL impairment in comparison to males. The same was observed by Naveed et al. [7], however others did not see that female acne patients are suffering more [24].