Introduction
Atopic dermatitis (AD) is a common chronic inflammatory skin disease characterized by inflammation, intense pruritus, recurrent eczematous lesions and a fluctuating course [1]. The prevalence of AD is as high as 15–20% in children in some high-income countries and continues to increase, especially in young children and in low-income countries [2, 3]. The first manifestations of AD usually appear early in life and often precede other atopic diseases such as asthma or allergic rhinitis [1]. Similar to psoriasis, AD has a significant impact on quality of life (QoL), work productivity, and everyday life [4]. AD also places a great financial burden on patients, their families, and society as a whole through direct and indirect costs [5].
Many studies showed that AD has profound effects on the lives of affected infants and children, and major secondary effects on their families [6–9]. However, little is known about the impact of AD on QoL of both afflicted children and their families in Montenegro, the upper middle-income country in South-eastern Europe.
Aim
The aim of this study was to assess the impact of AD on QoL in Montenegrin infants and their families, and to identify predictors affecting their QoL.
Material and methods
Study design and patients
This cross-sectional study was undertaken at the Clinic of Dermatology and Venereology, Clinical Centre of Montenegro (CCM), Podgorica, Montenegro, an upper middle-income country located in South-eastern Europe. The study was conducted between August 2017 and July 2018 and included infants with AD aged 0 to 4 years. The Hanifin and Rajka diagnostic criteria for AD were used [10].
The study was approved by the Ethics Committee of the CCM. Written informed consent was obtained from parents.
Assessment tools
Disease severity was assessed by the Three Item Severity (TIS) score, which corresponds well with the more detailed objective SCORAD (SCORing Atopic Dermatitis) index. It is a simple scoring system which uses three of the intensity items of the SCORAD index: erythema (0–3), oedema (0–3), and excoriations (0–3) in one or several different representative areas with a maximum score of 9. Based on the TIS, the severity of AD can be classified into mild (< 3), moderate (3–5) and severe (≥ 6) [11, 12].
The following instruments were used to measure QoL: The Infant’s Dermatitis Quality of Life Index (IDQOL) and the Dermatitis Family Impact (DFI) questionnaire, both linguistically validated and culturally adapted for use in Serbian speaking countries [13, 14]. The IDQOL is designed for use in infants with AD below the age of 4 years [15]. It comprises 10 questions about itching, child’s mood and sleep disturbances, difficulties in taking part in playing and family activities, problems during mealtime, when dressing and bathing, and problems caused by the treatment of the disease (further called “problems from treatment”). The IDQOL is calculated by summing the score of each question (0–3) resulting in a maximum of 30 and a minimum of 0. The higher the score the more QoL is impaired. There is an additional question which is scored separately, asking for the parents’ assessment of dermatitis severity, giving a choice from none to extremely severe (0–4). The DFI is designed to assess the effects of AD on family life domains. It also comprises 10 questions about housework, food preparation and feeding, sleep disturbances, family leisure activities, time spent on shopping, expenditure related to treatment, tiredness, emotional distress and family relationships within the last week. Each question is scored from 0 to 3. The minimum DFI score is 0 (no impact on family QoL) and the maximum DFI score is 30 (maximum effect on family QoL). That is, the higher the score, the poorer the QoL for the family [16]. Both the IDQOL and DFI questionnaires are designed to be completed in a 1-week recall period. Data on the child’s age, sex, concomitant atopic disease, family history of atopy, and parent’s age and education were also collected. The questionnaires were completed by one of the child’s parents, most frequently by the mother.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables through frequency and percentage. To assess differences between variables, Student’s t-test, and one way ANOVA with Tukey post hoc test, where appropriate. Pearson’s correlation and Spearman’s correlation coefficients were computed as measures of association. Two multiple linear regression models were used to determine whether IDQOL and DFI scores were related to sociodemographic and clinical characteristics of patients. Cronbach’s α was applied to assess the reliability of IDQOL and DFI scales. A two-tailed probability value of 0.05 or less was considered significant. All statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS), version 20.0 for Windows (SPSS Inc., Chicago, IL, USA) and STATA 13 program for graphical presentation.
Results
We recruited 186 children with AD for the study, 72 (38.7%) boys and 114 (61.3%) girls. The mean age was 2.35 ±1.01 years. Three quarters of infants (75.3%) had moderate disease severity, 17.2% had severe disease, and 7.5% had mild disease. The mean overall IDQOL score was 14.72 ±6.66, and the mean total DFI score was 17.78 ±6.11. There were no differences between boys and girls, either in the IDQOL or in the DIF overall scores (Table 1). However, both the IDQOL and DFI scores were higher among infants with the concomitant atopic disease (asthma, allergic rhinitis, and allergic conjunctivitis) in comparison to AD alone, and in those with a family history of atopic disease. Also, there were significant differences in QoL between mild, moderate and severe AD. More severe AD was categorized with higher IDQOL and DFI scores. Education of parents did not have any impact on infant’s and family QoL (Table 1).
Table 1
The Infants’ Dermatitis Quality of Life Index (IDQOL) and Dermatitis Family Impact questionnaire (DFI) scores related to the characteristics of the infants with AD (n = 186)
| Characteristic | Number (%) | IDQOL Mean ± SD | P-value | DFI Mean ± SD | P-value |
|---|---|---|---|---|---|
| All | 186 (100) | 14.72 ±6.66 | 17.78 ±6.11 | ||
| Sex: | |||||
| Boys | 72 (38.7) | 15.03 ±5.98 | 0.618* | 18.06 ±5.74 | 0.633* |
| Girls | 114 (61.3) | 14.53 ±7.07 | 17.61 ±6.35 | ||
| Age, mean ± SD | 2.35 ±1.01 | ||||
| Atopy: | |||||
| AD alone | 134 (72) | 13.64 ±6.59 | < 0.001* | 16.97 ±6.17 | 0.003* |
| Concomitant atopic diseases | 52 (28) | 17.50 ±6.06 | 19.88 ±5.48 | ||
| TIS score: | |||||
| Mild (TIS = 0–2), n (%) | 14 (7.5) | 8.57 ±3.80 | < 0.001† | 10.86 ±3.74 | < 0.001† |
| Moderate (TIS = 3–5), n (%) | 140 (75.3) | 13.81 ±5.45 | 17.10 ±5.47 | ||
| Severe (TIS ≥ 6), n (%) | 32 (17.2) | 21.38 ±7.67 | 23.81 ±4.63 | ||
| TIS, mean ± SD | 4.58 ±1.59 | ||||
| Family history of atopy: | |||||
| Yes | 107 (57.5) | 16.09 ±6.92 | < 0.001* | 19.25 ±5.82 | < 0.001* |
| No | 79 (42.5) | 12.86 ±5.82 | 14.92 ±5.67 | ||
| Education of parents: | |||||
| Low to middle | 78 (41.9) | 15.03 ±7.14 | 0.332† | 17.87 ±6.17 | 0.237† |
| High (college) | 24 (12.9) | 16.17 ±5.53 | 19.58 ±6.02 | ||
| High (university) | 84 (45.2) | 14.02 ±6.47 | 17.19 ±6.05 |
The 10 item scores of IDQOL and DFI, according to sex are presented in Table 2.
Table 2
The infants’ Dermatitis Quality of Life Index (IDQOL) and Dermatitis Family Impact questionnaire (DFI) scores according to sex
| Questionnaire | All (n = 186) | Boys (n = 72) | Girls (n = 114) | P-value* |
|---|---|---|---|---|
| IDQOL, mean ± SD: | ||||
| Total score | 14.72 ±6.66 | 15.03 ±5.98 | 14.53 ±7.07 | 0.618 |
| Itching and scratching | 1.80 ±0.74 | 1.78 ±0.75 | 1.81 ±0.74 | 0.795 |
| Mood | 1.83 ±0.80 | 1.86 ±0.76 | 1.81 ±0.83 | 0.655 |
| Time to get to sleep | 1.20 ±0.91 | 1.25 ±0.90 | 1.17 ±0.92 | 0.589 |
| Sleep disturbances | 1.03 ±0.86 | 1.03 ±0.84 | 1.03 ±0.88 | 0.955 |
| Disturbed playing | 1.42 ±0.84 | 1.61 ±0.76 | 1.30 ±0.86 | 0.013 |
| Disturbed family activities | 1.46 ±0.89 | 1.44 ±0.84 | 1.47 ±0.92 | 0.828 |
| Problems during mealtimes | 1.42 ±0.85 | 1.50 ±0.73 | 1.37 ±0.91 | 0.304 |
| Problems from treatment | 1.72 ±0.84 | 1.83 ±0.77 | 1.65 ±0.87 | 0.133 |
| Dressing problems | 1.38 ±0.84 | 1.28 ±0.73 | 1.44 ±0.90 | 0.186 |
| Problems at bath time | 1.46 ±0.90 | 1.44 ±0.84 | 1.47 ±0.94 | 0.830 |
| DFI, mean ± SD: | ||||
| Total score | 17.78 ±6.11 | 18.06 ±5.74 | 17.61 ±6.35 | 0.633 |
| Housework | 1.84 ±0.86 | 1.97 ±0.80 | 1.75 ±0.89 | 0.093 |
| Food | 1.64 ±0.76 | 1.72 ±0.70 | 1.60 ±0.79 | 0.272 |
| Sleep | 1.83 ±0.83 | 1.92 ±0.80 | 1.77 ±0.84 | 0.246 |
| Family leisure activities | 1.48 ±0.94 | 1.47 ±0.84 | 1.49 ±1.00 | 0.889 |
| Time for shopping | 1.44 ±0.88 | 1.47 ±0.84 | 1.42 ±0.90 | 0.699 |
| Expenditure | 2.11 ±0.70 | 2.06 ±0.67 | 2.14 ±0.71 | 0.420 |
| Tiredness | 1.89 ±0.77 | 1.89 ±0.74 | 1.89 ±0.79 | 0.960 |
| Emotional distress | 1.96 ±0.87 | 1.89 ±0.97 | 2.00 ±0.80 | 0.418 |
| Relationships | 1.63 ±0.89 | 1.75 ±0.90 | 1.56 ±0.88 | 0.161 |
| Treatment | 1.96 ±0.93 | 1.92 ±1.02 | 1.98 ±0.87 | 0.651 |
The highest scoring IDQOL items were those related to “child’s mood” (1.83 ±0.80), “itching and scratching” (1.80 ±0.74), and “problems caused by the treatment” (1.72 ±0.84), while the highest scoring DFI items were “expenditure” (2.11 ±0.70), “emotional distress” (1.96 ±0.87) and “treatment” (1.96 ±0.93). There were no differences between two sexes in the overall IDQOL and DFI scores, and in item scores, except for the IDQOL item “disturbed playing” which was more prevalent in boys than in girls (Table 2).
The IDQOL 10 item scores in the subgroups according to the severity of AD (mild, moderate and severe) are presented in Table 3. Significantly higher values of all scores were observed in the moderate group compared with the mild group and in the severe group compared with both the moderate and mild group (Table 3). The highest item values were in the severe group, particularly for “child’s mood”, “itching and scratching” and “problems from treatment”.
Table 3
The IDQOL 10 items scores in subgroups related to severity of atopic dermatitis
| IDQOL | Mild (n = 14) | Moderate (n = 140) | Severe (n = 32) | P-value* (moderate vs. mild) | P-value* (severe vs. mild | P-value* (severe vs. moderate) |
|---|---|---|---|---|---|---|
| Itching and scratching | 0.75 ±0.46 | 1.49 ±0.54 | 2.27 ±0.67 | < 0.001 | < 0.001 | < 0.001 |
| Mood | 0.75 ±0.46 | 1.47 ±0.61 | 2.37 ±0.66 | < 0.001 | < 0.001 | < 0.001 |
| Time to get to sleep | 0.25 ±0.46 | 0.80 ±0.57 | 1.80 ±0.93 | 0.004 | < 0.001 | < 0.001 |
| Sleep disturbances | 0.50 ±0.53 | 0.71 ±0.57 | 1.47 ±0.98 | < 0.001 | 0.002 | < 0.001 |
| Disturbed playing | 0.50 ±0.53 | 1.10 ±0.68 | 1.90 ±0.77 | 0.011 | < 0.001 | < 0.001 |
| Disturbed family activities | 0.25 ±0.46 | 1.16 ±0.77 | 1.95 ±0.78 | 0.015 | < 0.001 | < 0.001 |
| Problems during mealtimes | 0.75 ±0.89 | 1.12 ±0.72 | 1.85 ±0.80 | 0.006 | < 0.001 | < 0.001 |
| Problems from treatment | 0.75 ±0.46 | 1.43 ±0.73 | 2.17 ±0.74 | 0.021 | < 0.001 | < 0.001 |
| Dressing problems | 0.50 ±0.53 | 1.16 ±0.74 | 1.72 ±0.84 | 0.050 | < 0.001 | < 0.001 |
| Problems at bath time | 0.50 ±0.53 | 1.22 ±0.82 | 1.85 ±0.86 | < 0.001 | < 0.001 | < 0.001 |
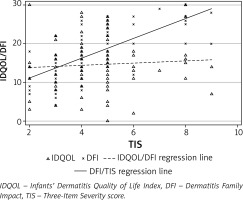
As shown in Figure 1 and Table 4, there was a significant correlation between AD severity score assessed by a doctor (TIS) and both the IDQOL and DFI scores (r = 0.61 and r = 0.67, respectively). Furthermore, the IDQOL and DFI scores correlated significantly (r = 0.79) as well as the AD severity score assessed by parents with the total IDQOL and DFI scores (ρ = 0.64 and 0.68, respectively) (Table 4). A lower correlation was observed between the TIS score and the AD severity score assessed by parents (ρ = 0.47).
Table 4
Correlation between overall scores on the Infants’ Dermatitis Quality of Life Index (IDQOL) and the Dermatitis Family Impact (DFI) questionnaire and AD severity
| Correlation | IDQOL | DFI |
|---|---|---|
| DFI | 0.79* (p < 0.001) | |
| AD severity as assessed by doctors (TIS score) | 0.61* (p < 0.001) | 0.67* (p < 0.001) |
| AD severity as assessed by parents | 0.64† (p < 0.001) | 0.68† (p < 0.001) |
Figure 1
Distribution of IDQOL/DFI scores with relation to the severity of atopic dermatitis according to TIS
All the items of both the IDQOL index and DFI questionnaire showed excellent internal consistency with mean Cronbach’s α coefficients of 0.93 and 0.90, respectively.
The results of multiple linear regression analyses are shown in Table 5.
Table 5
Predictive value of sociodemographic and clinical variables in relation to QoL measures in children with atopic dermatitis
| Score | Characteristic | B | 95% CI | P-value |
|---|---|---|---|---|
| IDQOL | Sex | –0.50 | –2.48–1.48 | 0.618 |
| Child’s age | 1.14 | 0.20–2.07 | 0.018 | |
| TIS | 2.56 | 2.08–3.04 | < 0.001 | |
| Atopic disease* | 3.86 | 1.78–5.94 | < 0.001 | |
| Parent’s age | 0.28 | 0.04–0.53 | 0.023 | |
| Education level of parents | –0.51 | –1.54–0.52 | 0.332 | |
| Family history of atopic disease* | 3.80 | 1.84–5.77 | < 0.001 | |
| DFI | Sex | –0.44 | –2.26–1.38 | 0.633 |
| Child’s age | 0.80 | –0.07–1.67 | 0.071 | |
| TIS | 2.56 | 2.14–2.87 | < 0.001 | |
| Atopic disease* | 2.91 | 0.99–4.84 | 0.003 | |
| Parent’s age | 0.14 | –0.08–0.37 | 0.211 | |
| Education level of parents | –0.35 | –1.30–0.60 | 0.467 | |
| Family history of atopic disease* | 4.33 | 2.57–6.09 | < 0.001 |
The positive independent association was observed between disease severity, presence of concomitant atopic disease, family history of atopic disease, child’s age, parent’s age and the overall IDQOL score as well as between disease severity, presence of other atopic disease, family history of atopic disease and the overall DFI score (Table 5).
Discussion
In the current study, a negative impact on QoL of infants with AD was observed. The overall IDQOL score was 14.72 which is higher than in all previous studies [11, 15, 17–26]. Such high score in Montenegrin infants, similar to those observed in the previous Montenegrin study [27], conducted at the same Dermatology Clinic at CCM, can be explained by the fact that patients referred to CCM (tertiary health care level) would be likely to have more severe disease than patients referred to a general practitioner in public health care centres (primary health care level).
We were unable to detect any significant gender difference in the overall IDQOL score that is in accordance with other studies [18, 23, 25]. In contrast, Chernyshov [22] found that an impact of AD on QoL was more severe for girls. The two IDQOL items showing the highest scores in this study referred to “child’s mood”, and “itching and scratching”. These items and “time to get the child to sleep” were the most affected items in several other studies [18, 25, 28].
A recently published systematic review highlighted the growing number of tools used to assess disease severity in randomized controlled trials on AD. Of the sixty-two identified disease severity measures, the SCORAD index was most commonly used [29]. However, the SCORAD was found to be too complicated and time consuming. That is why we decided to use TIS score, a reliable and simple system for scoring AD which strongly correlated with the SCORAD [11, 30] and was recommended for use in epidemiological studies [12] and in general practice [30]. Our results showed a strong positive correlation between the infants’ QoL measured by IDQOL and clinical disease severity (r = 0.61; p < 0.001), that is in agreement with previous studies [21, 23, 25, 27, 31]. Correlation of the IDQOL score with disease severity as assessed by parents was similar (ρ = 0.64). In the present study all IDQOL items reached significantly higher values in the severe group compared with the moderate or mild groups, which is in accordance with the study by Alzolibani [25].
Furthermore, as might be expected, the IDQOL score was significantly higher in infants with concomitant asthma, allergic rhinitis, or allergic conjunctivitis, than for those with AD alone. This finding is supported by other studies [18, 21, 23, 27]. However, contrary findings were also reported [25].
The impact of AD on QoL is not limited only to affected infants. AD also affects the physical, social and emotional functioning of parents. One of the aims of the present study was to assess the specific impact of childhood AD on the QoL of their parents. In the present study, the mean overall DFI score was 17.78 which is much higher than in previous studies [17, 18, 24, 26].
Like in other studies [17, 24] we found a high correlation between the IDQOL and DFI (r = 0.79, p < 0.001). The parents’ assessment of AD severity correlated well with both the IDQOL and DIF scores (ρ = 0.64, p < 0.001 and ρ = 0.68, p < 0.001, respectively) which was supported by the results of a large international multicentre study conducted in six countries (Ukraine, Czech Republic, Singapore, the Netherlands, Brazil, and South Korea) [24].
In this study parents having infants with a higher AD severity had worse QoL than parents of infants with less severe AD, which is in accordance with a Korean study [26]. We did not find any impact of infant’s gender on parents’ QoL. In contrast, Chernyshov [22] and Jang et al. [26] found that families of girls with AD had a lower QoL than families of boys.
Like the infants’ QoL, the QoL of their parents was worse for children with AD and concomitant atopic diseases (such as asthma, allergic rhinitis, and allergic conjunctivitis) than for those with AD alone (without atopic diseases). This finding is in accordance with a previous study [18].
Our results should be considered in the light of the strengths and weaknesses of the study. The main strength of this study is a large sample size of patients with AD. However, the study has some limitations. First of all, the study was performed at the Dermatology Clinic at CCM, a tertiary-level setting, where more severe patients used to be treated than in primary-level setting. Because of that it was not possible to generalize the results of our study to the all infants with AD in the population of Montenegro. Second, the absence of a control group did not allow the comparative analysis between our results and QoL of healthy infants and infants affected by other skin diseases.
Conclusions
The present study demonstrates and confirms that AD impairs QoL of Montenegrin infants, and also affects their families. Greater severity of disease was associated with greater impairment in QoL. Understanding QoL of infants with AD and their parents might help doctors to facilitate the management and treatment of infants with AD.








