Introduction
Autologous serum skin test (ASST) is an intradermal application of the patient’s serum sample to detect auto-antibodies against high-affinity immunoglobulin E (IgE) receptor, or IgE with a high sensitivity and specificity of about 80% [1].Positivity in ASST with an induration larger than 1.5 mm indicates autoimmunity in urticaria. This rapid in vivo test may help to detect circulating functional auto-antibodies, and thus may show the need of immunomodulatory therapy [2].The incidence of ASST positivity in patients with chronic spontaneous urticaria (CSU) is reported to be in a larger range, i.e. between 4.1% and 82.1%, which might be due to different criteria for positivity [1–3]. Although the general aspect is that ASST is not useful in diseases other than CSU, recent studies have shown ASST positivity in patients with asthma, rhinitis, multidrug allergy syndrome and healthy individuals, at a ratio of up to 55.55% [2, 4–7].Acute urticaria (AU) which lasts shorter than 6 weeks, has identifiable aetiology only in 50% of patients. General laboratory studies are not indicated in AU, however etiologic examination including ASST was shown to presume progression toward CSU [8].
Aim
The aim of this study was to determine the rationality of ASST in AU in comparison with CSU and healthy adults. We hypothesized that ASST is useful to identify aetiology not only in CSU, but also in AU.
Material and methods
This study was a prospective cross-sectional study carried out between 2016 and 2017. It was approved by the Local Ethical Committee of the Kirikkale University (2016/11/08). Patients were recruited from the Departments of Dermatology and Allergy in the Kirikkale University Hospital.
The diagnosis of AU and CSU was done according to the criteria of the European Academy of Allergy and Clinical Immunology (EAACI) [1].Recruitment criteria for patients included: 1) untreated urticaria patients, 2) diagnosed by an expert with a specialty in dermatology or allergy, 3) if the patient had a history of recurrent wheals over 6 weeks he/she was grouped as CSU, or vice versa, 4) the patients had no definite causes in history such as allergic diseases, autoimmune diseases, infections, or drug allergy evidence. Exclusion criteria were: 1) identified urticaria reason such as physical, cholinergic, vasculitis or hereditary angioedema, 2) using antihistamine within a week, steroid or immunosuppressive drugs within a month, 3) having an exact cause of urticaria during the study follow-up, 4) pregnant or nursing women were excluded. In AU, AST was not performed until the symptoms completely subsided.
Clinical details of all subjects were recorded. Selected patients were subjected to ASST and laboratory investigations. The ASST was performed with 0.5 ml of the patient’s own serum injected intradermally into the flexor aspect of the forearm; 0.5 ml of saline was injected 3 to 5 cm away as a control. The test was considered positive if the diameter of the papule after 30 min was 1.5 mm or greater than that of the saline papule [9].
Anti-thyroglobulin, antithyroid peroxidase (anti-TPO), free (f) T3, fT4, and TSH tests were also performed as autoimmunity indicators in addition to total immunoglobulin (Ig) gE tests in Immunoassay Analyzer (Roche, Basel, Switzerland). Deficiency levels of total IgE (< 100 IU/ml), sTSH (0.5–5 µU/ml), fT3 (2.2–4 pg/ml), fT4 (0.76–1.46 ng/ml), anti-thyroglobulin (< 40 IU/ml), anti-TPO (< 35 IU/ml)were determined according to the manufacturer’s standards. Abnormality in thyroid tests was defined as any thyroid test out of the normal range. A patient with clinical thyroiditis was defined as with abnormal TSH, fT3 and fT4 levels besides high levels of thyroid antibodies.
Statistical analysis
The data were recorded and processed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA). The positive rates are expressed as percentages and were analysed using the χ2 test. Numeric variables are expressed as means and were analysed using the Student’s T-test. A p-value < 0.05was considered significant.
Results
The study group was composed of adults with a mean age of 34.35 ±12.68 years, and a female dominance (58.4%) (Table 1). Patients were treatment naïve except 8.7% of the CSU group who used anti-allergic drugs long before admission.
Table 1
Characteristics of patient and control groups (N = 101)
Mean serum total IgE levels were significantly higher in patients with urticaria than the control group, but were similar between AU and CSU groups. Mean fT4, anti-thyroglobulin, and anti-TPO levels in the CSU group were higher than both AU and control groups (Table 2).
Table 2
Laboratory examination results (mean ± standard deviation)
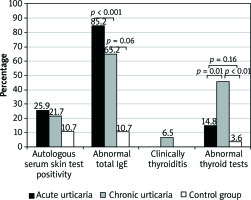
The ratio of ASST positivity was insignificantly higher in the AU (25.9%) and CSU group (21.7%) than in the control group (10.7%) (Figure 1). When serum test values were defined as abnormal according to normal limits, the results were also similar as mentioned above. In logistic regression analysis, no significant risk factor was determined for ASST positivity even if analysed separately in groups.
Discussion
The gold standard for the diagnosis of autoimmunity in CSU is to find positivity in these three tests; ASST positivity (auto-reactivity), bioassay positivity (basophile histamine release assay or basophile activation indicator expression), and immunoassay positivity (Western blot or ELISA immunoreactivity) [2].However, it is not a useful method to be applied to all CSU patients in practical life, since they need specialized laboratories.
Frequency of ASST positivity
ASST positivity in patients with CSU was reported between 4.1% and 82.1%, with different methods for positivity criteria [1–3].In this study, the ratio of ASST positivity was almost one fourth of the urticaria patients and one tenth of healthy ones. Even though these results were lower than in some studies, similarity between urticaria and healthy subjects was a frequent result as in other articles. For example, Taşkapan et al. found that its positivity was 53% in CSU patients, 20% in patients with allergic rhinitis/asthma, and 56% in healthy controls [2].Furthermore, this was one of the first studies comparing ASST positivity among AU and CSU patients. In PubMed search with key words of AU and ASST, there was only one research paper published by Magen et al. [8]. They reported ASST positivity as 63.4% in the CSU, and 23.3% in the AU group. However, this significant difference disappeared after 7 weeks of survey. The contrary results between the two studies may be attributed to different inclusion criteria. As we know this is the first study with patient enrolment from two different departments that deal with urticaria, and this side of the study makes sense if the whole population was included. We suggested that urticaria patients who were admitted to the Allergy Department had a suspicion of allergy, especially to drugs, whereas patients in the Dermatology Department were reported to have autoimmunity in a published paper.
Reliability of ASST
In this study, ASST was found to be insufficient to differentiate autoimmunity in patients from healthy subjects. Actually, it has been known that ASST is not specific for CSU. For example, Güven et al. found ASST positivity in patients with alopecia and vitiligo [10].Its sensitivity and specificity was reported as approximately 70–80% [11].It has been reported that this test was dependent on histamine and mast cell response, and can be passively transferred to healthy individuals. However, it is controversial whether circulating immune complexes are responsible for this response since only 50% of the patients with CSU had autoantibodies filled up [12, 13].Likewise, heating the serum to a certain temperature at which IgE was inactivated, did not change the positivity of the ASST [12, 14–16]. In this case, it would not be appropriate to consider urticaria patients with positive ASST as autoimmune ones [17–19]. Furthermore, in some studies, there was no relationship between ASST and treatment response or disease course [19]. These were the points that make the reliability of ASST doubtful.
Reproducibility of ASST
There are controversial reports advocating that the ASST is a reproducible test [16, 20–23]. Magen et al. observed that there was a conversion in ASST results of patients with CSU in follow-ups as positivity to negativity or vice versa. On the other hand, Eryılmaz et al. argued that ASST should be repeated several times to use it as a screening test for autoimmune urticaria [24]. Even though there was no follow-up in this study, the similarity of ASST results between AU, CSU, and healthy groups would suggest that there would be no change if patients with AU were followed up. We concluded that ASST was not rational in patients with CSU. ASST shows neither diagnostic value for autoimmunity nor reflects urticaria activity. It may be considered that ASST does not contribute to disease management.
Thyroid function test and total IgE results
Studies suggesting the role of thyroid autoimmunity and its relation with ASST in CSU are controversial. In some, ASST positivity was found to be higher in CSU patients that had thyroid autoantibodies than patients without [13, 25, 26]. Furthermore, an exact relationship in CSU patients between having higher autoimmune disease with determined autoantibody and ASST positivity was written in guidelines [1], even though there were opposite results advocating usefulness of ASST in showing autoimmunity [27, 28]. Finally, it was emphasized to look at thyroid autoantibodies although there was no significant difference of ASST between the CSU group and the control group [29]. Likewise, this study showed that clinically thyroiditis and/or abnormality in thyroid tests was significantly higher in the CSU group than the AU and healthy groups. Thus, we recommend performing routine thyroid autoantibodies and thyroid functional tests in CSU.
In this study, total IgE levels were significantly higher in urticaria patients than in the healthy group, which made us to think that patients of urticaria were rich of IgE levels as a target for mast or basophile cell mediator release. However, IgE levels are found to be unimportant to differentiate between AU and CSU patients.
Conclusions
Even though thyroid function tests were found to be related with CSU, and total IgE was associated with urticaria, ASST was found to be of importance. This study confirms that ASST is insufficient to demonstrate autoimmunity and acute-chronic urticaria nature. Further research about auto-antibodies in AU and CSU is needed.