Introduction
Worldwide prevalence of asthma varies between different regions and countries in a wide range from 1% to 16% [1]. The prevalence of asthma in the European Union (EU) was reported to be in the range 5–16% [2]. Although exact data on the prevalence of asthma in the Czech Republic (population of about 10 million) are not known, it was estimated that 8% of the Czech population, i.e. around 800 thousand people, suffered from asthma [1]. Nearly half of the estimated patients were reported to be under the care of allergologists and/or pulmonologists [3].
Many patients with severe asthma remain uncontrolled despite receiving combinations of high-dose inhaled corticosteroids (ICS) and long-acting β2-agonists (LABA) in addition to other medications (leukotriene receptor antagonists, theophylline) [4], and continue to experience asthma symptoms, lifestyle restrictions leading to poor quality of life and even frequent exacerbations needing emergency care [5].
Omalizumab is a humanized anti-immunoglobulin E (IgE) monoclonal antibody approved in the EU for patients with severe persistent allergic asthma aged ≥ 6 years who are inadequately controlled with high-dose ICS and LABA. As an add-on treatment, omalizumab has been shown to improve long-term asthma control and lung function, and reduce the use of corticosteroids, rescue medication and frequency of exacerbations in patients with persistent allergic asthma [6–8]. Supporting the results from clinical studies, real-world studies conducted in various European countries also reported improvement in asthma control and quality of life of patients after treatment with omalizumab [9–12]. To strengthen the evidence for omalizumab, a 2-year, global, post-marketing observational registry (eXpeRience) was conducted [13, 14].
Aim
Here, we report the outcomes of add-on omalizumab treatment in patients from the Czech Republic enrolled in the eXpeRience registry.
Material and methods
Design and patients
eXpeRience was a 2-year, international, post-marketing, non-interventional, multicentre (14 countries in Europe, the Americas and Asia), open-label, single-arm, observational registry which collected safety and effectiveness data from patients treated with add-on omalizumab for uncontrolled persistent allergic (IgE-mediated) asthma [13, 14]. The dose of omalizumab administered was determined following the European Medicines Agency Summary of Product Characteristics [15].
Patients were eligible for inclusion if they met the labelling and local re-imbursement requirements for omalizumab use and had received omalizumab between 15 weeks and 18 months prior to the start of the registry. All patients who provided informed consent entered the registry. Patients were excluded if they were participating in any other clinical study or had received omalizumab in the past 18 months. Detailed inclusion and exclusion criteria have been described previously [14].
The registry design was reviewed by independent ethics committees or institutional review boards at each centre, and the registry itself was conducted in accordance with the Declaration of Helsinki.
The current study was a post-hoc analysis of the global eXpeRience registry.
Assessments
After enrolment in the registry, patients’ baseline data (medical history, asthma status and control and medical resource use in the last 12 months before the start of the therapy) were collected retrospectively from their medical records. Patients were followed up for 2 years after initiation of omalizumab treatment and data were collected for analysis at week 16 ±1 week, and months 8, 12, 18, and 24. Data reported in this analysis include patient response to therapy (as determined by physician’s global evaluation of treatment effectiveness (GETE)), lung function (FEV1 % predicted and peak expiratory flow (PEF)), clinical symptoms (day- and night-time symptoms), use of rescue medication, use of oral and inhaled corticosteroids, number of clinically significant and severe asthma exacerbations, Asthma Control Test (ACT), patients’ health-related quality of life (mini-Asthma Quality of Life Questionnaire (mini-AQLQ)), medical healthcare resource use (hospitalisations, emergency room (ER) visits or unscheduled doctor visits or interventions), number of missed days of work/school, serious adverse events (SAEs) and deaths [13, 16, 17].
A clinically significant exacerbation was defined as any worsening of asthma considered by the treating physician to require systemic corticosteroids, and were recognised as severe if there was a reduction in PEF to < 60% of the patient’s predicted or personal best. Data on exacerbations were annualised; that is, for month 12, rates were derived from week 16, month 8 and month 12 data; for month 24, rates were derived from data collected at months 18 and 24 [14].
Global evaluation of treatment effectiveness analysis was performed at week 16 ±1 week by physicians. Patients were rated on a 5-point scale: 1 – excellent (complete control of asthma), 2 – good (marked improvement), 3 – moderate (discernible, but limited improvement), 4 – poor (no appreciable change), and 5 – worsening (overall deterioration of asthma control). Patients with an ‘‘excellent’’ or ‘‘good’’ response were considered responders, those with ‘‘moderate’’, ‘‘poor’’ or ‘‘worsening’’ as non-responders [18].
The ACT is a patient-reported 5-item questionnaire that assesses shortness of breath, asthma symptoms, rescue medication use, the effect of asthma on daily functioning, and self-rating of asthma control. Each item includes responses with values from 1 to 5 to give a final ACT score of 5 (poorly controlled asthma) to 25 (well-controlled asthma). An improvement of ≥ 3 units in the ACT score is considered to be the minimal important difference [17, 19].
The mini-AQLQ is a 15-item questionnaire (a shorter version of the 32-item AQLQ) covering four domains: symptoms (5 items), activity limitation (4 items which are patient specific), emotional function (3 items) and environmental stimuli (3 items). Patients were asked to respond to each question based on their experience during the previous two weeks, on a 7-point scale (0 – no impairment to 6 – maximum impairment). The overall mini-AQLQ score is the mean of all 15 responses. A change in mini-AQLQ score of ≥ 0.5 is considered to be the minimal clinically important difference [20, 21].
Statistical analysis
All effectiveness variables were analysed using the intent-to-treat (ITT) population, which consisted of all patients from the Czech Republic who enrolled in the whole registry and received at least one dose of omalizumab and who had at least one post-baseline efficacy assessment. For analyses at specific time-points, all patients with available data at that time-point were considered for the analysis. The safety population consisted of all patients from the Czech Republic who enrolled in the registry and who received at least one dose of omalizumab and had at least one post-baseline safety assessment. The safety population was used for collection of data on demographics, baseline characteristics and safety evaluation. Descriptive statistics are expressed as means with standard deviations (SD) or as frequencies. Repeated measures were treated using a general linear model for repeated measures (GLM-RM) or the Friedman ANOVA in cases of normality assumption violation. Frequencies were analysed using the χ2 test. Survival analysis was performed using the Kaplan-Meier algorithm (with mean survival time calculation) or Cox regression (with hazard ratio (HR) with 95% confidence interval calculation). The p-value < 0.05 was considered as statistically significant. Data were analysed by IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
Results
From a total of 943 patients enrolled in the eXpeRience registry, 114 patients originated from the Czech Republic. The ITT and safety population included 112 patients each. Patients’ demographics and baseline clinical characteristics are presented in Table 1. Overall, 17 (14.9%) patients discontinued the registry; reasons for discontinuation included lost to follow-up (n = 5), patient withdrew consent (n = 3), death (n = 1), and other reasons (n = 8); 7 patients from the Czech subgroup had missing data or unresolved data queries. At the end of the registry (month 24), data related to treatment were available for 81 patients from the Czech Republic.
Table 1
Baseline demographics and clinical characteristics (safety population) (N = 112)
| Variable | Results |
|---|---|
| Age group, n (%) [years]: | |
| < 12 | 1 (0.9) |
| 12–17 | 3 (2.7) |
| 18–64 | 102 (91.1) |
| ≥ 65 | 6 (5.4) |
| Age, mean ± SD [years] | 44.0 ±13.0 |
| Female, n (%) | 68 (60.7) |
| Race, n (%): | |
| Caucasian | 112 (100.0) |
| Other | 0 (0) |
| Body weight, mean ± SD [kg] | 77.3 ± 15.9 |
| Baseline IgE level, mean ± SD [IU/ml] | 290.3 ±262.5 |
| Duration of allergic asthma, mean ± SD [years] | 18.5 ±12.4 |
| FEV1 % predicted, mean ± SD | 61.0 ±16.3 |
| Positive skin-prick test/RAST for perennial aeroallergens, n (%) | 105 (93.8) |
| Specification, n (%)a: | |
| Dust mites | 81 (72.3) |
| Cat dander | 47 (42.0) |
| Dog dander | 50 (44.6) |
| Cockroaches | 3 (2.7) |
| Others | 19 (17.0) |
| History of allergy to seasonal aeroallergens, n (%) | 93 (83.0) |
| Smoking history, n (%): | |
| Never smoked | 85 (75.9) |
| Ex-smoker | 26 (23.2) |
| Current smoker | 1 (0.9) |
| Asthma clinical symptoms, n (%): | |
| Daytime asthma symptoms | 109 (97.3) |
| Limitations of activities | 110 (98.2) |
| Nocturnal symptoms/awakenings | 96 (85.7) |
| Asthma control, n (%)b: | |
| Partly controlled | 27 (24.1) |
| Uncontrolled | 85 (75.9) |
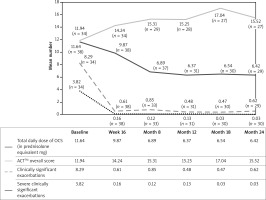
Physician’s global evaluation of treatment effectiveness
Ninety patients had a GETE assessment at week 16 ±1 week, of whom 88.9% (n = 80) were responders (excellent and good response to omalizumab therapy in 7.8% (n = 7) and 81.1% (n = 73) of patients, respectively), and 11.1% (n = 10) were non-responders (Figure 1). For GETE assessed at any time-point, 85.7% (n = 96) of patients were responders whereas 14.3% (n = 16) were non-responders.
Figure 1
Physician’s global evaluation of treatment effectiveness (GETE) at week 16 ±1 weeks (n = 90)
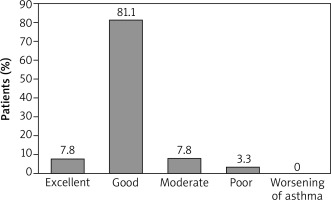
The effect of GETE on health care use risk is described in the section Healthcare utilisation and missed work days.
Lung function
Treatment with omalizumab resulted in improvement in FEV1 with a mean change from baseline (ml) of 205 (n = 105), 215 (n = 88), 273 (n = 87), 200 (n = 85) and 137 (n = 80) at week 16 and months 8, 12, 18 and 24, respectively. The PEF was also improved with a mean change from baseline (l/min) of 11.01 (n = 82), 18.38 (n = 66), 32.82 (n = 65), 25.18 (n = 63) and 21.85 (n = 60) at week 16 and months 8, 12, 18 and 24, respectively.
Asthma symptoms and rescue medication use
Omalizumab reduced the number of patients experiencing daytime symptoms, nocturnal symptoms/awakenings, activity limitations and rescue medication use in the week before months 12 and 24 versus baseline. During the week prior to the baseline visit, 108 (96.4%) patients had been using rescue medication; this was reduced to 61 (75.3%) patients at month 24. Mean use of rescue medication (short-acting β2-agonists) decreased from 5.2 days/week at baseline to 2.9 days/week at month 24 of omalizumab treatment (Table 2).
Table 2
Effect of omalizumab on asthma symptoms, rescue medication and corticosteroid use
| Parameter | Czech Republic | ||
|---|---|---|---|
| Baseline (n = 112) | Month 12 (n = 89) | Month 24 (n = 81) | |
| Daytime symptoms*: | |||
| Number of days: | |||
| Mean (SD) | 5.5 (2.2) | 2.6 (2.4) | 2.6 (2.5) |
| N (%) | 109 (97.3) | 72 (80.9) | 63 (77.8) |
| Change in number of days: | |||
| Mean (SD) | – | –2.7 (2.5) | –2.7 (2.6) |
| N | 88 | 81 | |
| Nocturnal symptoms/awakening*: | |||
| Number of days: | |||
| Mean (SD) | 3.2 (2.4) | 1.1 (1.5) | 0.9 (1.5) |
| N (%) | 96 (85.7) | 44 (49.4) | 34 (42.0) |
| Change in number of days: | |||
| Mean (SD) | – | –2.0 (2.4) | –2.3 (2.1) |
| N | 89 | 81 | |
| Limitations of activities*: | |||
| Number of days: | |||
| Mean (SD) | 5.0 (2.1) | 2.2 (2.0) | 2.2 (2.2) |
| N (%) | 110 (98.2) | 72 (80.9) | 57 (70.4) |
| Change in number of days: | |||
| Mean (SD) | – | –2.8 (2.3) | –2.9 (2.4) |
| N | 87 | 80 | |
| Rescue medication use*: | |||
| Number of days: | |||
| Mean (SD) | 5.2 (2.4) | 3.0 (2.8) | 2.9 (2.8) |
| N (%) | 108 (96.4) | 70 (78.7) | 61 (75.3) |
| Change in number of days: | |||
| Mean (SD) | – | –2.1 (2.6) | –2.1 (2.7) |
| N | 89 | 80 | |
| ICS usage: | |||
| Patients on ICS, n (%) | 111 (99.1) | 87 (97.8) | 78 (96.3) |
| Total ICS daily dose (beclomethasone dipropionate equivalent µg), mean (SD) | 2196.4 (1162.9) | 1947.2 (876.1) | 1886.4 (945.4) |
| Number of patients with reduced ICS dose, n (%) | – | 21 (23.6) | 21 (25.9) |
Oral corticosteroid use
Oral corticosteroids (OCS) were used as maintenance therapy in 38 patients (33.9%) with a mean total daily dose of 11.6 mg (prednisolone equivalent). The proportion of patients on OCS maintenance therapy compared to baseline decreased by 50% (n = 19) and 52.6% (n = 18) patients at months 12 and 24, respectively. The mean total daily dose of OCS (in prednisolone equivalent, mg) in the population using OCS maintenance therapy at baseline decreased to 6.4 mg at months 12 and 24 (Figure 2).
Exacerbations
The mean number of clinically significant exacerbations decreased with omalizumab from 5.7 (n = 104) at baseline to 1.1 (n = 89) and 0.7 (n = 80) and severe exacerbations decreased from 2.2 (n = 105) at baseline to 0.2 (n = 89) and 0.1 (n = 81) at months 12 and 24, respectively (Table 3). Furthermore, the proportion of patients with no clinically significant/severe exacerbations was markedly increased with omalizumab therapy to 56.2% (n = 50)/89.9% (n = 80) and 63.0% (n = 51)/95.1% (n = 77) at months 12 and 24, respectively. The mean numbers of clinically significant exacerbations and severe exacerbations in the population using OCS maintenance therapy at baseline are presented in Figure 2.
Table 3
Asthma control, quality of life, exacerbations and asthma related medical healthcare use after omalizumab treatment
| Parameter | Czech Republic | ||
|---|---|---|---|
| Baseline | Month 12 | Month 24 | |
| Total number of clinically significant asthma exacerbations: | |||
| N | 104 | 89 | 80 |
| Mean (SD)* | 5.7 (7.4) | 1.1 (1.8) | 0.7 (1.2) |
| Number of severe clinically significant asthma exacerbations: | |||
| N | 105 | 89 | 81 |
| Mean (SD)* | 2.2 (3.3) | 0.2 (0.7) | 0.1 (0.3) |
| Patient’s level of asthma control†: | n = 112 | n = 89 | n = 81 |
| Controlled, n (%) | 0 (0.0) | 22 (24.7) | 20 (24.7) |
| Partly controlled, n (%) | 27 (24.1) | 60 (67.4) | 51 (63.0) |
| Uncontrolled, n (%) | 85 (75.9) | 7 (7.9) | 10 (12.3) |
| ACT overall score: | |||
| N | 103 | 84 | 75 |
| Mean (SD) | 12.4 (4.1) | 17.3 (5.0) | 17.3 (5.4) |
| Change from baseline in ACT score: | |||
| N | – | 81 | 73 |
| Mean (SD) | 4.3 (4.0) | 4.3 (3.8) | |
| Mini-AQLQ overall score: | |||
| N | 46 | 45 | 41 |
| Mean (SD) | 3.62 (1.0) | 4.56 (1.4) | 4.67 (1.4) |
| Change from baseline in mini-AQLQ overall score: | |||
| N | – | 38 | 32 |
| Mean (SD) | 0.80 (1.0) | 0.94 (0.8) | |
| ≥ 0.5 improvement, n (%) | 23 (60.5) | 21 (65.6) | |
| Total number of days of asthma related medical healthcare use per patient‡: | |||
| N | 99 | 88 | 80 |
| Mean (SD) | 6.8 (10.0) | 0.8 (2.1) | 0.4 (1.2) |
| Number of days missed work due to asthma: | |||
| N | 43 | 43 | 38 |
| Mean (SD) | 24.3 (27.4) | 2.4 (6.4) | 1.7 (5.1) |
| Number of asthma related hospitalisations: | |||
| N | 105 | 89 | 81 |
| Mean (SD) | 0.5 (1.2) | 0.0 (0.0) | 0.0 (0.2) |
| Patients without asthma related hospitalizations, n (%) | 77 (68.8) | 89 (100.0) | 80 (98.8) |
| Total number of days stayed in hospital due to asthma: | |||
| N | 100 | 89 | 81 |
| Mean (SD) | 3.3 (9.8) | 0.0 (0.0) | 0.2 (2.2) |
Asthma control and health-related quality of life
After 12 and 24 months of omalizumab treatment, 92.1% (n = 82) and 87.7% (n = 71) of patients reported controlled or partly controlled asthma, which is substantially higher than that at baseline (24.1%; n = 27), as per physicians’ assessment (Table 3).
The ACT scores increased from 12.4 (n = 103) at baseline to 17.3 (n = 84) and 17.3 (n = 75) at months 12 and 24, respectively. Clinically meaningful improvements from baseline in ACT scores were observed with omalizumab treatment at months 12 (mean change: 4.3 points, n = 81) and 24 (mean change: 4.3 points, n = 73) (Table 3).
In OCS maintenance therapy at baseline, mean ACT score increased from baseline by 27.7% and 29.9% at months 12 and 24, respectively (Figure 2).
Similar improvements were observed in patient health-related quality of life assessed using the mini-AQLQ. Mean changes of 0.8 and 0.94 points in the mini-AQLQ from baseline werer observed at months 12 (n = 38) and 24 (n = 32), respectively. Overall, 60.5% (n = 23) and 65.6% (n = 21) of patients achieved clinically meaningful improvements in the mini-AQLQ score versus baseline (Table 3).
Healthcare utilisation and missed work days
Asthma-related total medical healthcare use (hospitalisations and ER/unscheduled doctor visits) per patient and missed days of work due to asthma were decreased with add-on treatment with omalizumab at months 12 and 24 compared with baseline (Table 3). The mean ± SD total number of days of asthma-related medical healthcare use per patient decreased from 6.8 ±10.0 during the 12-month pre-treatment period (n = 99) to 0.8 ±2.1 and 0.4 ±1.2 at months 12 (n = 88) and 24 (n = 80), respectively with omalizumab. Thus, healthcare resource utilisation was reduced compared with baseline by 88.2% and 94.1% at months 12 and 24, respectively.
The effect of GETE on medical healthcare use risk was calculated using Cox regression (overall model evaluation p < 0.001). The reference value was defined as poor responders. The calculated hazard ratio (HR) for moderate responders was 0.26 (p = 0.04, 95% CI: 0.072–0.937), HR (good responder) = 0.168 (p < 0.001, 95% CI: 0.067–0.462) and HR (excellent responder) = 0.117 (p = 0.01, 95% CI: 0.023–0.599). We did not register any case of worsening asthma during the study period (Figure 3). Thus in contrast to poor responders, excellent, good and moderate responders had a reduced risk of healthcare use by 88.3%, 83.2% and 74%, respectively.
Figure 3
Effect of physician’s global evaluation of treatment effectiveness (GETE) on medical healthcare use risk calculated by Cox regression (n = 112)

The mean ± SD number of days of missed work due to asthma decreased from 24.3 ±27.4 at baseline (n = 43) to 2.4 ±6.4 and 1.7 ±5.1 at months 12 (n = 43) and 24 (n = 38), respectively. Mean number of days of missed work due to asthma decreased by 90.1% and 93.0% after months 12 and 24, respectively.
The mean ± SD number of asthma-related hospitalisations decreased from 0.5 ±1.2 in the 12-month pre-treatment period (n = 105) to 0.0 ±0.0 at month 12 (n = 89) and 0.0 ±0.2 at month 24 (n = 81). The mean ± SD number of days stayed in hospital due to asthma decreased from 3.3 ±9.8 in the 12-month pre-treatment period (n = 100) to 0.3 ±2.0 at month 12 (n = 89) and to 0.2 ±2.2 at month 24 (n = 81). Overall, 100% and 98.8% of patients were free of asthma-related hospitalizations at months 12 (n = 89) and 24 (n = 80), respectively.
Serious adverse events
A total of 11 serious adverse events (SAEs) were reported in the 112 patients from the safety population. Four patients experienced each SAE in the 2-year observational period in the Czech Republic. These SAEs (hepatic failure, pneumonia in right lung, pulmonary embolism, sigmoid diverticulitis) were not suspected to be study-related. One patient experienced cumulated AE (headache, dizziness, flushing, hyperhidrosis, tremor, and dry mouth), which was considered as an SAE, and this was suspected to be study-related, leading to treatment withdrawal. One death occurred in this study group during the 2-year observation period (sudden death, due to viral endocarditis), which was reported as not being related to the treatment.
Discussion
The eXpeRience registry was designed to collect data on the real-world effectiveness and safety of omalizumab in patients with uncontrolled persistent allergic asthma [14]. Results from this international registry provide data on patient demographics and baseline characteristics, treatment effectiveness and safety after 24 months of add-on omalizumab therapy [13, 14]. The baseline demographics and clinical characteristics of the Czech Republic sub-population were comparable with the overall eXpeRience registry patient population.
Treatment effectiveness in patients from the Czech Republic was demonstrated by using GETE at 16 ±1 weeks. The investigators rated the majority of patients as responders to omalizumab therapy (excellent/good; 88.9%), which was 27.2% higher than that in the overall population (69.9%) [13].
In the Czech Republic, physicians refer patients with asthma who are not able to achieve complete control even with GINA step 4 treatment to one of the specialised sites of the National Centres for Severe Asthma (NCTA) [22]. Each individual patient is re-evaluated in these centres for asthma diagnosis, comorbidities and complicating factors. Based on the consensus of both an allergologist and a pulmonologist from each centre, biological therapy could be initiated. Only NCTA centres are eligible to indicate biological treatment with anti-IgE antibody (omalizumab) in the Czech Republic [22, 23].
After 16 weeks, and 8, 12, 18 and 24 months of treatment with omalizumab, lung function assessed as mean change from baseline in FEV1 improved by 205 ml, 215 ml, 273 ml, 200 ml and 137 ml, respectively. The effect of add-on omalizumab to high-dose ICS/LABA on FEV1 is comparable to what was reported for add-on tiotropium in patients with poorly controlled asthma [24].
Omalizumab add-on treatment in the Czech Republic sub-population resulted in considerable reductions in the daytime and nocturnal symptoms, limitations of activities, and rescue medication use, which was comparable with results seen in the overall population of the eXpeRience registry and other real-life studies [10, 11, 13, 25–29]. There was also a considerable reduction from baseline in the number of patients on OCS maintenance therapy (n = 38) to 24 months after the treatment (n = 18) along with a 44.8% reduction in the total daily dose from 11.6 mg at baseline (prednisolone equivalent) to 6.4 mg at month 24. The effect on OCS maintenance dose was associated with a substantial increase in ACT score. In this regard, it is worth noting that omalizumab add-on treatment is recommended in GINA as the preferred choice over OCS in step 5 [1]. Severe asthma patients require long-term treatment, and withdrawal from omalizumab may cause loss of asthma control and increase exacerbations and the OCS maintenance dose [29–31].
From the results presented in this report, it is evident that omalizumab add-on treatment reduced the number of clinically significant exacerbations (annualised) from 5.7 at pre-treatment to 0.7 after 24 months of treatment in the Czech Republic sub-population. These results were similar to those observed in the global registry (4.9 to 0.6), Czech Anti-IgE Registry (CAR) and other real-life data with up to 9 years of follow-up [9, 13, 28, 29, 32, 33]. Additionally, clinically meaningful improvements in asthma control (ACT; mean change from baseline of 4.3 units) and patient health-related quality of life (mini-AQLQ; mean change from baseline of 0.94 units) were also observed. These results are supported by the results from various other studies (ACT improvement of 5.01 and AQLQ improvement of 0.91 from baseline) [7, 34]. Based on the investigator assessment in the Czech Republic, a higher percentage of patients had controlled or partly controlled asthma at month 12 versus baseline (92.1% vs. 24.1%) upon treatment with omalizumab. These results were higher than those seen in the overall population of the eXpeRience registry and symptoms remained controlled at month 24. Asthma-related healthcare resource utilisation and days of missed work due to asthma were also substantially reduced with omalizumab treatment in the Czech Republic sub-population. Reliability of GETE assessment at 16 ±1 weeks as a predictor of healthcare use risk was analysed and significant risk reduction was seen for excellent responders (88.3%), good (83.2%) and moderate responders (74.0%). These results indicate both a clinical benefit and an overall economic benefit (direct medical cost savings in healthcare utilisation and improvement at work productivity) [35]. Only 1 patient reported SAE that was considered to be study treatment related. The frequency of SAEs reported in the Czech Republic subgroup population (5.4%) was similar to that reported in the global eXpeRience registry (6.9%) and various clinical studies (3% to 6%) [25, 36, 37]. The single death reported was not related to omalizumab.
The limitation of this Czech Republic sub-population analysis is the low patient number for data analysis, in addition to limitations mentioned previously for the overall eXpeRience registry [13]. Moreover, demographic and clinical factors other than the treatment of interest may contribute to the observed effects in observational studies. Perceived physician bias in patient selection and continuation on omalizumab therapy beyond 16 weeks could have influenced the outcomes (for example, physicians were not blinded to the treatment). Another limiting factor could be the relatively infrequent data collection. Despite these potential obstacles, the present findings are in line with those from the randomised controlled trials, and statistical power was further invigorated by the repeated measures design. Thus, the improvement in clinical outcomes observed here is very likely due to omalizumab treatment. Since this study utilises an observational registry, there was no placebo arm; it is therefore possible that some of the improvements seen with omalizumab treatment may be partly related to a placebo effect and/or to the closer monitoring of the patients enrolled in the registry. Another limitation is that patients’ baseline data were collected retrospectively from their medical records. Nevertheless, the baseline characteristics were similar to those in the global registry [13].
Conclusions
The results from the Czech Republic subgroup analysis are supportive of the existing evidence that omalizumab add-on therapy improves lung function and asthma control and reduces OCS use, exacerbations, healthcare utilisation and absence from work in patients with uncontrolled persistent allergic asthma [14]. These findings are likely to be relevant to the positive impact of omalizumab on the direct and indirect healthcare costs and in reducing the socioeconomic burden of uncontrolled allergic asthma in the Czech Republic. Patients’ assessments and omalizumab administration are performed at the network of National Centres for Severe Asthma. Such specialized centres should be made accessible to the patients with uncontrolled allergic asthma for optimal care. GETE assessment is an effective predictor of long-term response to omalizumab treatment in the Czech Republic.