Classic dermatomyositis (DM) is an idiopathic inflammatory myopathy characterized by symmetric, proximal muscle weakness and a wide range of cutaneous findings. Its pathogenesis is not fully understood, however, it is believed that immunogenetic and probably other factors have a significant impact on the manifestation of the disease. Classically, patients exhibit proximal skeletal muscle weakness accompanied by cutaneous symptoms i.e. heliotrope eruption on the eyelids, shawl sign, Gottron sign. Scrotum involvement is an unusual finding in DM. To the best of our knowledge, scrotal ulcerations accompanied by severe pain have been extremely rarely reported as the first dominant manifestation of the disease.
A 35-year-old man presented with‾severe pain in the scrotum area impeding walking as well as weakness of proximal muscles of the upper and lower extremities. He reported that 4 weeks before admission he had an upper respiratory tract infection with a fever up to 38°C. A week later he noticed erythema, swelling and marked soreness of the scrotum followed by the appearance of erosions on the scrotal skin and on the oral mucosa. He also noted the weakness of the proximal muscles of the upper and lower extremities.
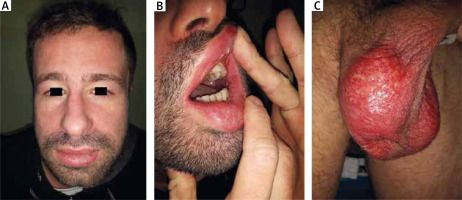
On admission shallow erosions and ulcerations on the erythematous background over the entire surface of the scrotum, as well as in the vestibule of the mouth and on the lateral surfaces of the tongue were observed. Erythema and swelling of the face and lips were also found. On the extremities, swelling of the hands, erythematous papules over the small joints of the hands (Gottron sign) and desquamative erythematous lesions on the arms and legs were noticed (Figure 1).
Figure 1
Skin lesions in a 35-year-old man with dermatomyositis. A – Erythema and erosions on the scrotum, B – oedema and erythema on the face, C – erosions on the oral mucosa
Investigations revealed increased muscle enzymes activity: alanine aminotranspherase (ALT) 71 U/l (normal values: 90–55 U/l)), aspartate aminotranspherase (AST) 159 U/l (normal values: 5–34 U/l), and creatine kinase (CK) 1924 U/l (normal values: 30–200 U/l). Peripheral blood count and peripheral blood biochemistry were within the normal ranges except for elevated ESR 13 mm (normal values: 3–8 mm). Antinuclear antibodies ANA were positive (titre: 1 : 320), whereas myositis-specific autoantibodies were negative. Direct immunofluorescence obtained from the oral mucosa demonstrated deposition of complement protein C3c at the dermal-epidermal junction. Histology of the oral mucosa revealed diffuse, partially more abundant lymphocytic infiltrate in the connective tissue stroma. Direct immunofluorescence obtained from the scrotum erythematous lesion showed deposition of IgM at the dermal-epidermal junction. On light microscopy, scrotum skin lesion showed vacuolar changes in the basal keratinocyte layer and a perivascular infiltrate composed mainly of lymphocytes in the dermis. Performed electromyography revealed abnormal spontaneous activity of the muscles including insertional activity, fibrillation potentials, and complex repetitive discharges. Virology including HAV, HBV, HCV, EBV, CMV and HIV was negative. Bacterial and yeast culture results obtained from scrotum, prepuce and urethra were also negative. Antigen tests for Chlamydia trachomatis was negative. Neoplasm markers were within the normal ranges.
The clinical picture together with the results of additional tests indicated the diagnosis of dermatomyositis. Initially, in the treatment with high doses of prednisone (1 mg/kg/day) were administered, subsequently slowly tapered within 3 months to 0.5 mg/kg per day. The patient improved rapidly in terms of skin changes, pain and muscular weakness. The oral lesions resolved after three weeks of therapy. Scrotum oedema subsided within a week, while scrotum erythema and erosions healed after 4 weeks of treatment. Due to gradual resolution of the skin lesions, the dose of prednisone was further reduced. On the follow-up, 5 months after therapy administration, he has been asymptomatic on the maintenance therapy with a very low dose of prednisone (0.125 mg/kg/day).
So far, only 5 cases of scrotal involvement in DM have been described in world literature. On this basis, three groups of symptoms have been distinguished: scrotal calcinosis, oedema, and dermatitis with erosions or ulcerations.
Calcinosis is a common manifestation in juvenile DM usually found in subcutaneous tissue, muscles, fascia or tendons on the extremities. Scrotal calcinosis was described in two children and one 42-year-old man. The first case was a patient suffering from DM with disseminated calcinosis since the age of two, who developed scrotal pain and swelling accompanied by calcinosis of the scrotum after 4 years of disease duration [1]. The scrotum calcinosis was improved after 6 months of the therapy with alendronate in association with intravenous immunoglobulins (IVIG). In the second described patient, at the age of 13 scrotal tenderness and calcinosis was detected and the lesions improved after treatment with alendronate only [1]. In turn, in a 42-year-old patient with amyopathic DM, painful lesions in the course of calcinosis in the scrotum were surgically removed [2].
Oedema, especially associated with heliotrope eruption is a common finding in the periorbital area, however, in other regions of the body it is observed less frequently. Penile and scrotum swelling with mild erythema were reported in a 10-year-old patient with a history of severe DM with cutaneous vasculitis and oedema of the face and limbs [3]. The lesions were accompanied by significant muscle weakness and atrophy, vasculitis, disseminated calcinosis and periorbital rash. The changes have been resolved after rituximab therapy (4 cycles).
The third type of skin lesions in the scrotum described in the literature is erosions, ulcers and necrosis [4, 5]. Cutaneous ulcerations, most frequently seen in the juvenile DM, indicate underlying vasculopathy in the skin and may be a sign of similar processes involving internal organs, primarily the lungs and intestines. In the literature, a 6-year-old boy was described who presented with severe DM and extensive ulcerations involving scrotum, prepuce, gluteal region, neck, bilateral axilla, periumbilical area and bilateral elbows and popliteal fossa [4]. The patient required combined therapy including pulses of methylprednisolone, intravenous cyclophosphamide, mycophenolate mofetil and subcutaneous methotrexate, that induced remission of the symptoms.
To the best of our knowledge, we report the first case of an adult patient with extensive painful erosions on the scrotum. The lesions accompanied by severe pain were the dominant symptom of the disease associated with typical manifestations of DM. The cutaneous lesions as well as muscle weakness subsided after the therapy with glucocorticosteroids in slowly tapered doses.








