Introduction
Atopic dermatitis (AD) is a chronic childhood dermatosis that not only affects patients’ well-being but also, as a source of chronic stress for caregivers, disrupts the functioning of the entire family [1]. The disease burden involves the child’s ailments, but it also requires parents to take constant care of the skin, provide a special diet, avoid exacerbating factors, and seek alternative therapies. The amount of time spent on caring for children with AD, lack of sleep, emotional discomfort of seeing a child suffering, and the need to adjust the family’s lifestyle to the disease contribute to deterioration of well-being, finances, and relationships and in turn to high levels of stress in the parents [2–4]. Parents of children with AD are likely to develop depressive symptoms, anxiety, and sleep problems, which can decrease psychosocial functioning [1]. It was demonstrated that mothers experience higher level of stress than fathers, which is probably associated with time spent on parenting and doing housework [2]. Our previous data showed that mothers of children with AD experienced significantly higher levels of stress compared with mothers of healthy children [5]. Recently, Lee et al. have also found a higher frequency of stress perception and suicidal ideation in mothers of children with AD compared with mothers of unaffected children [2].
The effectiveness of stress management by caregivers affects adherence to treatment and consequently contributes to successful or poor outcomes [6].
Two of the most common concepts of stress were described in Lazarus and Folkman’s Transactional Model of Stress and Coping and Hobfoll’s Conservation of Resources Theory [7, 8]. Our present study is based on the former, which deals with stressful situations in the processual and transactional contexts. Authors defined coping as “constantly changing efforts that include cognitive processes and types of behaviour taken to meet the internal and/or external requirements, which are perceived as overwhelming or exceeding the individual’s capabilities” [7]. Coping may take one of two forms: problem-focused coping aimed at solving and preventing the cause of the stressful situation or emotion-focused coping that promotes the use of strategies for coping with negative emotions [9]. This concept was broadened by Carver et al., who developed the Coping Orientation to Problems Experienced (COPE) Inventory, a tool for evaluating coping strategies that may be problem focused, emotion focused, or other [10]. The transactional concept of stress was verified by Endler and Parker, who classified coping styles as task oriented, emotion oriented, and avoidance oriented [11].
As coping plays an important role in managing the stress involved in taking care of children with AD, ascertaining coping strategies with a validated measure seems to be the primary step in developing effective coping programs for parents.
Aim
The aim of this study was to compare strategies for coping with stress in mothers of children with and without AD. Moreover, coping strategies of mothers of affected children were investigated for relationships with stress intensity, quality of life, and AD variables such as AD severity, disease duration, and itch severity.
Material and methods
Participants
A total of 120 Caucasian mothers of children with AD (AD group) and 70 mothers of children without AD (control group) were invited to participate in the study. Children with AD were hospitalized in the Department of Dermatology, Paediatric Dermatology, and Oncology at the Medical University of Lodz, Poland. Children without AD visited the same Department of Dermatology on an outpatient basis or attended a preschool located in Lodz. The inclusion criteria were age of the child from 3 months to 18 years, AD diagnosis according to Hanifin and Rajka criteria [12], and age of the mother of at least 18 years. The exclusion criteria were additional chronic and non-atopic diseases in AD patients and psychiatric or other chronic disorders in mothers.
The study was accepted by the Bioethics Committee of the Medical University of Lodz (RNN/296/17/KE) and was performed according to the principles of the Declaration of Helsinki. Informed consent was obtained from all participants, and participation was voluntary.
Atopic dermatitis assessment
To assess the severity of eczema in children, the Scoring Atopic Dermatitis (SCORAD) index was used, which combines the extent, intensity, and subjective symptoms (e.g. sleep loss). The total score range is from 0 to 103, and AD severity was classified into mild (< 25), moderate (25–50), or severe (> 50) [13].
To evaluate the intensity of pruritus in children, the modified Numerical Rating Scale (NRS) was used. Mothers of children with AD indicated the intensity of their children’s itch from the past 3 days on a 10-cm horizontal line with numbers from 0 to 10 (0 – no itch, 10 – the worst itch). Itch NRS scoring was classified as follows: mild (< 3 points), moderate (3–7 points), and severe or very severe (≥ 7 points) [14, 15].
Perceived stress level and quality of life assessment
The Perceived Stress Scale (PSS-10) was used to measure the perceived level of stress of mothers during the last month [16]. It consists of 10 questions scored from 0 (never) to 4 (very often), and hence a total score range from 0 to 40. The Polish version of the scale has a Cronbach’s α of 0.86.
Additionally, mothers of children with AD filled out the Family Dermatology Life Quality Index (FDLQI), which consists of 10 questions about the influence of the child’s skin disease on various aspects of family life in the last month. Subjects choose 1 out of 4 answers scored 0–3, which gives a total score range from 0 to 30 [17]. Higher scores indicate poorer quality of life.
Assessment of coping strategies
To evaluate strategies for coping with stress, the Coping Orientation to Problems Experienced (COPE) scale was used. The scale consists of 60 items representing 15 different coping strategies: active coping, planning, suppression of competing activities, restraint coping, seeking social support for instrumental reasons, seeking social support for emotional reasons, positive reinterpretation and growth, acceptance, denial, turning to religion, focus on and venting of emotions, behavioural disengagement, mental disengagement, humour, and alcohol/drug disengagement. Subjects choose 1 out of 4 answers about behaviour in a stressful situation, scored from 1 (I never behave in such a manner) to 4 (I almost always behave in such a manner). The scores are added up for each strategy (range: 4–16 points) [10].
Statistical analysis
The results were presented as means and standard deviations (SD). The data were analysed using a nonparametric test (data did not meet the assumptions of normality and equality of variances) and described in descriptive statistics. The correlation was determined using Pearson’s correlation coefficient for normally distributed data or Spearman’s rank correlation coefficient for non-normally distributed data. The level of significance was set at α = 0.05. The size of the study cohort was determined using the principle of an anticipated response distribution of 50%, with a 95% confidence interval (CI) and 10% precision. All analyses were performed with Jasp ver. 0.12.1/774 (University of Amsterdam, Netherlands).
Results
Characteristics of study groups
From a total of 120 mothers of children with AD and a total of 70 mothers of children without AD, 88 and 52 mothers returned the completed questionnaires, respectively (response rate 73.33% vs. 74.29%). Detailed characteristics of the study groups, including sociodemographic data, AD parameters, and overall psychosocial health status were described in our previous work on the relationship between AD in children and the psychosocial functioning of their mothers [5].
In brief, the average age of mothers and children in the AD group was similar to that of the control group (about 35 years and about 60 months, respectively) (Tables 1 and 2). Sex distribution differed between children in the AD and control groups (Table 2). The average duration of AD was 43.7 months. Most children (69.3%) had been suffering from AD for at least 6 months. Assessment of AD severity in children showed that the mean SCORAD score was 46.6 points, and mild, moderate, or severe AD was reported in 12.5%, 52.3%, and 35.2% of children, respectively. The mean itch NRS score was 6.1 points, with mild, moderate, or severe pruritus noted in 12.5%, 33.0%, and 54.5% of children, respectively (Table 2).
Table 1
Maternal characteristics
Table 2
Children’s characteristics and atopic dermatitis severity
The perceived stress level assessed with PSS-10 was significantly higher in mothers in the AD group than in the control group. Quality of life impairment score in the AD group was slightly higher than the midpoint of the FDLQI scale. The intensity of stress was moderately and positively correlated with the quality of life impairment (Table 3).
Strategies for coping with stress
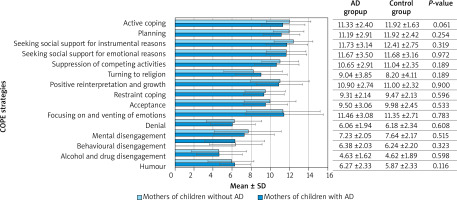
The frequency of choosing particular coping strategies did not differ significantly between the mothers in the AD and control groups. Mothers in both groups were more likely to choose active coping, seeking social support for instrumental and emotional reasons, focusing on and venting of emotions, and planning. By contrast, coping strategies such as denial, mental and behavioural disengagement, humour, and alcohol and drug disengagement were used less frequently (Figure 1).
It was also investigated whether the duration of AD affected the choice of coping strategies. Mothers of children suffering from AD for over 6 months were found to more frequently choose active coping (p < 0.05) and turning to religion (p < 0.05) compared with mothers of children with AD lasting less than 6 months.
The relationships between different coping strategies and disease and stress outcomes were examined in the group of mothers of children with AD (Table 4). It was found that longer disease duration enhanced suppression of competing activities (rs = 0.222, p < 0.05), while increased AD severity reduced restraint coping (rs = –0.238, p < 0.05), denial (rs = –0,306, p < 0.01), and mental disengagement (rs = –0.232, p < 0.05) (Table 4). The itch intensity was not significantly correlated with any coping strategies. Higher level of perceived stress promoted positive reinterpretation and growth (rs = 0.230, p < 0.05), focusing on and venting of emotions (rs = 0.281, p < 0.01), and alcohol/drug disengagement (rs = 0.245, p < 0.05). Quality of life impairment favoured such strategies as planning (rs = 0.249, p < 0.05), suppression of competing activities (rs = 0.351, p < 0.01), and turning to religion (rs =0.296, p < 0.01). Other correlations were not statistically significant.
Table 4
Correlations between different coping strategies and parameters of atopic dermatitis, stress, and quality of life perception in the group of mothers of children with atopic dermatitis (n = 88)
| COPE strategies | Spearman’s Rho (rs) | ||||
|---|---|---|---|---|---|
| SCORAD | Itch NRS | Disease duration | PSS 10 | FDLQI | |
| Active coping | –0.031 | 0.088 | 0.174 | 0.018 | 0.139 |
| Planning | 0.025 | 0.124 | 0.013 | –0.114 | 0.249 (*) |
| Seeking social support for instrumental reasons | 0.214 | 0.158 | 0.066 | –0.075 | 0.112 |
| Seeking social support for emotional reasons | 0.075 | 0.108 | 0.029 | –0.034 | 0.086 |
| Suppression of competing activities | –0.004 | 0.212 | 0.222 (*) | 0.125 | 0.351 (**) |
| Turning to religion | –0.049 | 0.015 | 0.192 | 0.130 | 0.296 (**) |
| Positive reinterpretation and growth | –0.061 | –0.077 | –0.047 | 0.230 (*) | 0.054 |
| Restraint coping | –0.238 (*) | –0.097 | –0.073 | 0.028 | 0.095 |
| Acceptance | –0.002 | 0.013 | 0.035 | 0.109 | 0.152 |
| Focusing on and venting of emotions | 0.148 | 0.064 | –0.075 | 0.281 (**) | 0.140 |
| Denial | –0.306 (**) | –0.164 | –0.136 | 0.105 | –0.195 |
| Mental disengagement | –0.232 (*) | 0.007 | 0.039 | 0.148 | 0.084 |
| Behavioural disengagement | –0.189 | –0.206 | –0.087 | 0.165 | –0.083 |
| Alcohol and drug disengagement | –0.020 | 0.062 | 0.062 | 0.245 (*) | 0.196 |
| Humour | –0.215 | –0.094 | –0.104 | 0.041 | –0.026 |
Discussion
As reported by many authors, having a child with AD significantly correlates with the quality-of-life impairment and high level of perceived stress of the mothers [2, 3, 5, 18]. Moreover, our previous research showed that mothers of children with AD had significantly higher insomnia, anxiety, and depression scores than mothers of healthy children. The scores increased with the duration of the disease [5]. In this study, we investigated whether the child’s disease severity, stress intensity, and quality of life affect the choice of coping strategy. We also tried to refer to data of some authors who emphasized that the chosen coping strategies might have an impact on experienced stress and quality of life. For example, using active coping strategies positively affects the quality of life [19, 20].
Coping strategies and correlations
Strategies for coping with stress in parents of children with AD are important but rarely studied. Our findings showed that there were no significant differences in choosing coping strategies between the mothers of children with and without AD despite the fact that mothers of children with AD experience high mental health burden and high levels of stress [2, 5, 18]. Hence, it can be presumed that the high intensity of stress in mothers of children with AD, affecting also the quality of life, is not caused by using less effective strategies or inappropriate coping behaviours. Instead, it may be associated with the child’s illness itself and the need to provide adequate care, including at night. This assumption is partially confirmed by our previous results showing that higher severity of disease is associated with higher perception of stress and poorer quality of life [5]. On the other hand, in this study we observed that higher SCORAD results were related with decreased usage of strategies like restraint coping, denial, and mental disengagement. This may suggest that the high severity of the disease makes mothers less likely to use less effective strategies and target more effective solutions. It seems to be a proper approach in the context of results of a meta-analysis that considered non-avoidance strategies as more beneficial for long-term stress, which undoubtedly comes with the care of a child with AD [21]. However, even if mothers of children with AD used relevant coping strategies, they are insufficient in the case of a child’s chronic illness. As was mentioned before, the use of active coping strategies may reduce stress and improve quality of life [19, 20]. However, although mothers of children with AD were using some of these strategies, they still experienced high level of stress.
There were several statistically significant correlations between the selected coping methods and the severity of the child’s AD, duration of the disease, perceived stress, and quality of life of mothers of affected children. However, because the correlations can be regarded as weak (rs < 0.4), probably due to the small sample size (n = 88), they require further verification. A slight positive correlation between the duration of AD and suppression of competing activities could mean that the longer the disease, the more mothers focus on the problem of AD and look for a solution. Such an assumption is supported by findings of studies on coping strategies in parents of chronically ill children (e.g. with cystic fibrosis) emphasizing that coping methods are related to the chronicity of the disease [22]. Perceived stress was weakly correlated with emotion-focused strategies such as positive reinterpretation and growth, focusing on and venting of emotions, and alcohol and drug disengagement. Quality of life impairment promoted different types of strategies: planning and suppression of competing activities (problem-focused) and turning to religion (emotion-focused). Interestingly, according to other authors, people using passive strategies obtain lower scores for indicators of well-being [23, 24]. Also, the use of emotion-oriented strategies is associated with higher level of stress, anxiety, and depression [25].
To sum up, mothers experiencing increased stress related to their child’s AD are more likely to mobilize and use varied task-oriented and emotion-oriented strategies and, to a lesser extent, avoidance-oriented methods.
However, due to the weak nature of the correlations, we cannot unambiguously determine whether the factors connected with AD severity will modify the coping strategies used by mothers.
Nevertheless, our results suggest that the commonly used coping strategies are insufficient for mothers of children with AD. Therefore, they need support in coping with stress and strengthening strategies that contribute more to reducing perceived stress.
How can we improve the coping skills and well-being of parents of children diagnosed with AD?
It needs to be highlighted that the diagnosis of AD, which is usually traumatic for the parents, is followed by immediate initiation of medical treatment and lifestyle adjustments to adhere to the specific regimen [26]. Thus, every parent’s effort to cope should be supported from the beginning, since the diagnosis by preventive counselling, to avoid the stress caused by misinformation. Parental education is important in managing childhood chronic diseases. A study by Pustisek et al. showed that a 2-hour simple structured educational program about the course of disease and treatment was enough to reduce the level of stress in parents of children with AD from 21 points to 16.97 points on the PSS-10 scale [27]. According to other studies, parents of children with AD who participated in the educational multi-session programs experienced significant improvement in the quality of life [28, 29].
The well-being of caregivers of children with AD affects compliance with the recommendations and effectiveness of treatment. A study by Tu et al. highlighted the importance of fostering constructive and positive coping in caregivers, which in consequence leads to improved symptoms and control of AD [30]. Because of increased socioemotional burden, impairing quality of life [5], mothers of children with AD need to be supported both for their comfort and for children’s benefits. A stress management program targeted at caregivers of children with AD who experience highly elevated stress symptoms would be one of the solutions, which may encourage participants to assess the usefulness of their current coping strategies and promote more functional coping strategies. Some easily accessible relaxation techniques, such as meditation and mindfulness-based stress reduction, can help to reduce the negative consequences of chronic stress [31]. Cognitive behavioural therapy seems to be an effective treatment for clinical depression, anxiety, and high level of stress [32].
The stepped-care intervention “mental health” model is a useful tool that allows adjustment of the most appropriate strategy of treatment to the patient’s needs. First of all, it is important to diagnose the problem at the very beginning; therefore, screening for depression, anxiety, sleep, and stress disorders should be performed [33–35]. Then, depending on the severity of the disorders, an appropriate level of intervention is applied. In mild cases, guided self-help or brief psychological interventions may be used, whereas in severe cases, medication and complex intervention should be applied. Individuals may be ‘stepped up’ or ‘stepped down’ in the case of disorder enhancement or reduction. The stepped-care intervention has been implemented in many health domains, including depression and anxiety [34], Internet use disorders [36], and problematic substance use [37]. So far there is no established model of stepped care for AD. In the case of parents of children with AD, the first, basic step of the intervention could involve participation in supporting groups and psychoeducation (including relaxation, schools of atopy). However, it is also important to inform caregivers that such therapies are available to them. Taking into account that our lives are becoming increasingly digitalized, implementation of digital health interventions would also be reasonable [33, 38].
Limitations
The study was conducted at a single centre in Poland, which limits the generalization of the results to other populations because cultural context can influence the use of specific strategies for coping with stress. Mothers were recruited from a hospital dermatology ward, where more severe cases of eczema are more prevalent, and this may also limit the generalization of our findings. Also, the observed relationships between the evaluated variables were rather weak, probably due to the small sample size, so they require further analysis.
Conclusions
Our study showed that although mothers of children with AD experience increased stress levels and impaired quality of life, they do not choose different coping strategies compared to mothers of healthy children. Hence, intense stress in mothers of children with AD is not caused by inappropriate coping behaviours. However, the commonly used coping strategies seem to be insufficient in the case of child’s AD. Therefore, it is important to support mothers of children with AD in strengthening the coping strategies that contribute to reducing perceived stress, because their well-being has an impact on treatment effectiveness.