INTRODUCTION
Xanthelasma palpebrarum (XP) is the most common form of cutaneous xanthoma, which is a benign periorbital tumor containing mainly lipid droplets within cells. Xanthelasmas typically occur in middleaged or elderly people as multiple, soft, yellowish plaques most frequently located on the medial aspects of the upper and lower eyelids [1, 2]. Lesions are symmetrically distributed and may be singular or multiple, nodular or flat, and soft, semisolid or calcareous [2]. Histologically, lipid-containing foam cells are found in the superficial dermis. The cells cluster around blood vessels and may even involve their walls [1]. In the literature, xanthelasmas are divided into 4 stages period. The fourth stage corresponds to a diffuse lesion that affects both the medial and lateral parts of the upper and lower eyelids [3]. Giant xanthelasmas is a term used to indicate the fourth-stage xanthelasma extensively involving all four eyelids [4]. Although xanthelasma lesions are usually benign and asymptomatic, their removal is often requested for aesthetic purposes [5]. Even if patients manage to control their cholesterol level by adhering to a strict low-lipid diet and taking medication such as statins, the giant lesions tend to extend and occupy the eyelids area, which requires a well-thought-out therapeutic approach [5]. Numerous treatment options have been used to treat XP, such as surgical resection, chemical peeling, cryotherapy, targeted injections and ablations with various lasers, e.g. carbon dioxide, erbium-YAG, pulsed dye, Nd-YAG. For extensive xanthelasma, a combination of surgical removal, eyelid reconstruction and skin grafting is often suggested, but also carbon dioxide (CO2) and Er:YAG lasers have shown promising results, with a significant percentage of patients experiencing substantial improvement [6].
For giant xanthelasmas surgical treatment has several disadvantages, including the need for skin grafting, which may result in suboptimal aesthetic outcomes. Additionally, graft contraction can impair functional movements of the eyelids. Furthermore, it may lead to the development of a prominent scar [4].
Chemical peeling is also not recommended for the treatment of giant xanthelasma palpebrarum due to difficulties in controlling the depth of penetration of the exfoliating agent, which may result in retraction, hypertrophic scarring, or damage of the anatomical structures of the eyelids. Lasers other than the CO2 laser provide inferior hemostasis during procedures [4]. The CO2 laser is considered the most effective and gold standard treatment for xanthelasma palpebrarum, particularly in deeper lesions, due to its superior thermal tissue penetration. However, giant xanthelasmas, owing to their extensive tissue involvement, may still present a therapeutic challenge even when using the CO2 laser [5].
OBJECTIVE
To present a rare case of giant xanthelasma palpebrarum successfully treated with a CO2 laser, achieving excellent and long-lasting aesthetic and functional outcomes.
CASE REPORT
A 62-year-old male patient presented to a general practitioner with progressive edema and erythema around the right eye, suspected to be secondary to an insect bite. Due to the presenting symptoms, the patient was prescribed methylprednisolone 16 mg once daily, with a gradual tapering of 4 mg per day orally, as well as hydrocortisone eye ointment. After the resolution of the edema, the patient observed the appearance of bilateral yellow plaques on all eyelids and was referred to a dermatologist. On physical examination, the right supraorbital lesion measured 3 × 1.5 cm, the right infraorbital lesion 3 × 1 cm, the left supraorbital lesion 3 × 1 cm, and the left infraorbital lesion 2 × 0.5 cm. Partial ptosis of the right upper eyelid was also noted (fig. 1). No similar lesions were detected elsewhere on the body. The patient had a known history of type 2 diabetes mellitus and hypercholesterolemia.
Figure 1
The patient before CO2 laser procedures has giant xanthelasmas palpebrarum involving all four eyelids. The right supraorbital lesion was 3 × 1.5 cm, infraorbital lesion was 3 × 1 cm and the left side supraorbital lesion was 3 × 1 cm and infraorbital lesion was 2 × 0.5 cm

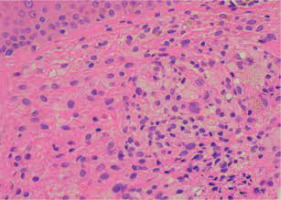
Considering differential diagnoses such as necrobiotic xanthogranuloma and leishmaniasis, a 4 mm punch biopsy was performed along with blood tests for ANA/ ENA IgG autoantibodies, serum protein electrophoresis/ immunoelectrophoresis, and a conjunctival smear for Leishmania spp. Histopathological examination revealed multiple clusters of macrophages with lipid droplets in cytoplasm and mild interstitial dermal and perivascular edema, findings characteristic of xanthelasma, thereby confirming the diagnosis (fig. 2). No autoantibodies were detected, and protein fractions remained within normal limits, effectively excluding monoclonal gammopathy associated with necrobiotic xanthogranuloma. Additionally, no Leishmania DNA was identified in the conjunctival smear from the right eye.
Figure 2
In histopathology the collection of macrophages with lipid droplets within their cytoplasm, slight interstitial dermal and pericapillar edema was found
The cutaneous lesions negatively impacted the patient’s quality of life due to cosmetic and functional concerns. Ablation of the giant XP was performed using a carbon dioxide (CO2) laser in three sequential procedures at one-month intervals. Analgesia was achieved by infiltration anesthesia with 2% lidocaine prior to each session. Titanium intraocular eye shields were used to protect the eyes. The procedure employed a CO2 laser (Deka Duoglide, Italy) with a surgical handpiece in fully ablative pulsed emission—High Pulse (HP) mode— with power settings of 1.5–2.5 W and frequency between 50 and 80 Hz. The HP mode was selected for its ability to achieve ablation with reduced thermal damage to surrounding tissues. No complications occurred during or after the treatment. At the 7-month follow-up, excellent results were observed, with no common side effects such as scarring or dyspigmentation. The patient expressed high satisfaction (fig. 3).
DISCUSSION
The prevalence of XP in the general population ranges from approximately 1.1% to 4.4% [7]. Giant xanthelasmas are rare and have a high recurrence rate of up to 80% following treatment [4]. XP occurs more frequently in women (32%) than men (17.4%), with the most commonly affected age group being 30–50 years [2, 8].
Xanthelasmas in 50% are associated with hypercholesterolemia [9, 10]. Cholesterol esterified with saturated fatty acids is selectively deposited in xanthelasmas, primarily originating from serum that often contains abnormally elevated levels of total and esterified cholesterol [8]. If xanthelasmas occur before the age of 50 or in the presence of elevated low-density lipoprotein levels in the lipid profile, a familial lipoprotein disorder should be considered [11]. Xanthelasmas can result from primary hyperlipidemias, such as familial hypercholesterolemia, or secondary hyperlipidemias associated with conditions including hypothyroidism, diabetes mellitus, primary biliary cholangitis, and nephrotic syndrome. Additionally, certain medications (e.g., glucocorticoids, cyclosporine, cimetidine, estrogens, some antihypertensives, retinoids, specific antiepileptics, anabolic steroids, tamoxifen) and dietary factors (diets high in saturated fats, cholesterol, and alcohol) may contribute to their development [2, 12].
In the present case, the patient was on daily treatment for type 2 diabetes mellitus, hypothyroidism, primary arterial hypertension, and statins, with the SGLT-2 inhibitor being the only medication potentially promoting xanthelasma formation [13].
Xanthelasma palpebrarum may present with clinical features similar to necrobiotic xanthogranuloma, syringomas, adult-onset asthma, periocular xanthogranuloma, palpebral sarcoidosis, and sebaceous hyperplasia [2]. Other differential diagnoses to consider include juvenile xanthogranuloma and nodular basal cell carcinoma. However, key distinguishing features of xanthelasma palpebrarum are its bilateral occurrence, typical location above the medial canthus, and characteristic yellowish coloration of the lesions [12].
Numerous treatment options have been used to treat XP, such as surgical resection, chemical peeling, cryotherapy, targeted injections and ablations with various lasers, e.g. carbon dioxide, erbium-YAG, pulsed dye, Nd-YAG [6]. During laser therapy, light is absorbed by tissue chromophores corresponding to the laser’s specific wavelength. The main skin chromophores are melanin, hemoglobin, and cellular water. Absorption of light by these chromophores generates thermal energy, which is transferred to surrounding tissues, causing tissue destruction. In xanthelasma, this thermal energy damages perivascular foam cells, leading to their elimination [14].
CO2 lasers are considered the most effective and gold standard treatment for XP, especially for deeper lesions due to greater thermal tissue penetration [5]. However, giant xanthelasmas are rare, and no single standardized treatment protocol exists. The CO2 laser emits a carbon dioxide beam absorbed by cellular water – a chromophore present in collagen, blood vessels, and epidermal keratinocytes — causing tissue vaporization and ablation. This mechanism enables its use in skin resurfacing and removal of epidermal lesions [4, 14, 15]. Ablative CO2 laser induces fractional photothermolysis, triggering molecular cascades that affect cytokines, heat shock proteins (HSPs), and matrix metalloproteinases (MMPs). The pulsed High Pulse (HP) emission mode achieves deeper ablation with less thermal damage compared to Deka Pulse (DP) or Smart Pulse (SP) modes [16]. Multiple treatment sessions are necessary to minimize risks of iatrogenic telecanthus, ectropion, and other complications related to scar contraction [4]. Common side effects include dyspigmentation, scarring, and edema. However, these risks decrease when the procedure is performed by experienced clinicians [5]. In this case, the CO2 laser was selected for its ability to provide gentle, selective photothermolysis of the surrounding tissues.
CONCLUSIONS
Giant XP are very rare and their treatment algorithm is not clearly defined. Therefore, accurate differentiation from other similarly looking lesions with proper intervention are crucial. It is necessary to choose the correct treatment to reduce the risk of frequent recurrence and prevent complications. In this context, pulsed CO2 laser therapy represents an effective option, offering excellent, long-lasting results with high patient satisfaction.









