Lupus erythematosus tumidus (LET) is a chronic relapsing inflammatory disease of the skin and was first described by Erich Hoffmann in 1909 [1]. Lupus erythematosus tumidus is characterized by a relatively mild course of the disease. LET usually occurs in the fourth or fifth decade of life, affects more women than men, with the majority of cases being reported in the Caucasian race [2]. Morphological and clinical morphological features of children and adults with LET are quite similar [3]. The clinical diagnosis may be burdensome since lupus erythematosus tumidus very often presents without associated systemic symptoms and the lesions are without characteristic features [4]. Diagnosing paediatric cases of lupus erythematosus tumidus may be more difficult as the condition is extremely rare in this age group; so far only 12 cases of this disease have been reported in children [2, 5–11].
Herein we present the case of lupus erythematosus tumidus in childhood with head and neck involvement, successfully treated with chloroquine. An 8-year-old female patient was admitted to the Dermatology Ward because of recurrent skin changes on the face and arms that have presented as well-demarcated and indurated pink plaques on the face (mainly the cheeks, eyelids and the right side of the forehead) resembling erythematous-exfoliating rings with a clearly defined, rounded dark pink edge (Figure 1 A). Dermoscopy revealed blurry linear-irregular/reticular vessels along multifocal whitish areas over a pinkish background and whitish bright areas over a reddish/purple background with or without dotted/linear-irregular vessels and haemorrhagic spots (Figure 1 C). Appearance of lesions was not accompanied by fever or prodromal symptoms. These skin changes first appeared during spring approximately 12 months prior to the hospital admission, the onset of lesions was related to sun exposure. When skin changes appeared for the first time, they resolved spontaneously without treatment after about a week. Subsequent recurrences of similar skin lesions occurred three more times, during the summer months, for the last time a week prior to hospital admission. The patient had a family history of psoriasis and no chronic comorbidities. She had no cutaneous lesions elsewhere and no clinical eye symptoms and systemic findings. Laboratory investigations, including complete blood cell count, erythrocyte sedimentation rate (ESR), liver tests and urine tests, were within reference values. The antinuclear antibody (ANA) indirect immunofluorescence assay was negative. Scrapings from lesions for mycological examinations were taken and results were negative.
Figure 1
A – Clinical presentation of the indurated ring-shape erythematous plaques on the face. B – Dermoscopy in polarized light (10× magnification) revealed the presence of blurry linear-irregular/reticular vessels along multifocal whitish areas over a pinkish background and with whitish bright areas over a reddish/purple background with linear-irregular vessels and haemorrhagic spots. C – Histopathologic examination with superficial and deep dermal perivascular, interstitial and periappendageal lymphocytic infiltration (hematoxylin-eosin staining; 100× magnification)
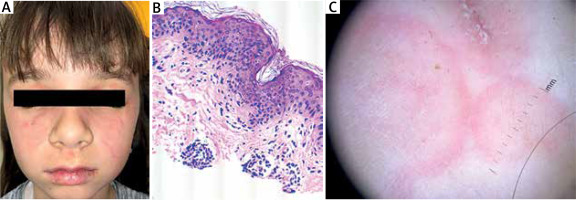
Skin biopsy revealed superficial and deep dermal perivascular, interstitial and periappendageal lymphocytic infiltration associated with stromal mucin deposits (Figure 1 C). Thus, the diagnosis of lupus erythematosus tumidus was made.
The preferred therapeutic option for lupus in children is hydroxychloroquine, drug unavailable at the time, therefore we had initiated treatment with 7.5 mg/kg oral chloroquine which resulted in a complete clinical remission, after 2 weeks chloroquine dosage was reduced to 3.75 mg/kg. Literature data indicate no difference in the effectiveness of both drugs in the treatment of lupus erythematosus tumidus [12]. No side effects were observed during treatment. Regular eye examinations and blood tests were performed monthly. The patient’s parents were informed that effective photoprotection is the most essential and effective approach to avoid photoaggravation of LET.
On her follow-up visit 4 weeks after discharge from hospital, her lesions on the face showed obvious improvement. Plaques and induration had almost disappeared. Only mild post-inflammatory hyperpigmentation and remaining erythema could be found.
LET has a chronic, recurrent and relatively mild course. The characteristic features of the skin lesions are annular or semi-annular in appearance, skin changes resolve spontaneously without scarring, discoloration or atrophic skin changes [4, 12]. LET is characterized by extreme photosensitivity, it occurs mainly in sun-exposed areas [6, 12].
There is no specific theory concerning the pathogenesis of LET, most hypotheses are derived from the study of other cutaneous lupus erythematosus (CLE) subtypes. UV-induced damage of the skin, impaired clearance of apoptotic cells and externalized autoantigens as well as innate and acquired immune response dysfunction are all implicated in the development of LET lesions. The pathogenesis of CLE remains unclear, and is likely multifactorial. One hypothesis, as yet unconfirmed, suggests that skin lesions caused by exposure to sunlight in the LET can arise when certain peptides bind to autologous DNA, which leads to the formation of immunocomplexes that activate plasmacytoid dendritic cells (PDCs), inducing the production of type I interferon. Interferon induces the production of chemokines (CXCL 9, 10 and 11) by epithelial cells, fibroblasts and keratinocytes, which amplifies the inflammatory response. Identified associations with subsets of CLE suggest future research questions in CLE pathogenesis [13].
Although single lesions in LET often resolve spontaneously if disease recurrence occurs, treatment may be necessary. In single lesions, the desired therapeutic effect can often be obtained with topical therapies, such as topical corticosteroids, topical calcineurin inhibitors and may not require further treatment. However, systemic therapy is often used in patients with refractory or repeatedly relapsing LET.
Systemic treatment with antimalarial drugs is considered essential in the treatment of CLE and SLE and the first-line systemic therapy for refractory LET. Their favourable efficacy profile and relatively few side effects support the decision to use systemic therapy, especially in the case of frequent relapses or resistance to local treatment of the disease. A recent meta-analysis of all studies including treatments of CLE patients with antimalarials reported 145 courses of antimalarials in LET patients and an overall response rate of 68% [14].
Kreuter et al. found no difference in efficacy between the group treated with chloroquine and the group treated with hydroxychloroquine. Lower incidence of adverse effects and equal efficacy might favour the use of hydroxychloroquine [12].
Among children, LET is an extremely rare entity and treatment protocols are based on adult treatment regimens, case reports and anecdotes [6, 8, 10, 11].
Paediatric cases of LET may be more challenging as the condition is extremely rare in this age group. Dermoscopy may be a useful tool for improving the recognition of LET especially in the paediatric population. Frequent dermoscopy patterns is irregular vessels along with multifocal whitish areas over a pinkish background with annular arrangement [15]. Dermoscopy is not sufficient to establish the diagnosis of LET but it is helpful in differential diagnosis.
Effective treatment of tumid lupus is imperative because the recurrence and persistence of lesions can affect quality of life. Further research and investigations are needed to define this condition more precisely.








