Introduction
Venous leg ulcers (VLUs) often heal slowly and result in long-term suffering and intensive use of health care resources [1, 2]. VLUs represent a growing health problem, and they are a condition that is very expensive to treat for both the health system and the patients.
VLUs endanger the patient’s normal life. Treatment of VLUs requires dedication and cooperation between the patient and the doctor. The health-related impact of VLUs is increasingly recognized as a valuable outcome measure for assessing interventions, especially when complete cure is improbable [3].
Patients with VLUs often have different symptoms: pain, sleep disturbance, depression, swelling of the lower extremities, fatigue and symptoms associated with inflammation of the lower leg (redness, localized heat, discomfort due to high exudate levels and itching) [4]. The patients experience a high-level burden of symptoms. Patients with VLUs have four or more concomitant symptoms [5]. It should be noted that approximately 20% to 30% of patients have ulcers that heal very slowly or do not heal at all, despite receiving adequate medical care [6].
How there are differences between different compression systems in relation to cost, application expertise, comfort and ease of use, all relevant information must be provided to both doctors and patients [7–9].
Aim
The aim of the study is to compare the effectiveness of two different sub-bandage pressure values on healing and quality of life outcomes.
Material and methods
One hundred and sixteen patients with VLUs over 18 years of age who were treated on an outpatient basis at the Nis Clinical Centre were monitored. Patients were followed for 24 weeks. A duplex scan of the lower extremity veins and arteries was performed. In all patients, an ankle-brachial pressure index (ABPI) was determined. The direction of the flow was estimated in the 20–30° reverse Trendelenburg position during the Valsalva manoeuvre.
In a standing position, a cuff inflation-deflation method was performed with rapid cuff inflation to induce reflux. A significant flow in the feet indicated reflux. A reflux time of < 0.5 s was used to determine and diagnose the presence of reflux.
Patients with ABPI < 0.8, with pre-existing heart failure (ejection fraction < 35), patients on immunosuppressive drugs, patients with malignant diseases, pregnant women, and patients with cortical therapy were excluded from the study. Patients with VLUs associated with pyoderma gangrenous, other neutrophilic dermatoses, cutaneous vasculitis and bilateral ulcerations were excluded from this study, too.
This research used patient data such as age, sex, previous venous surgery, previous episodes of ulceration, body mass index (BMI), history of deep vein thrombosis, calf circumference, ulceration location, size of the ulcer, number of ulcers, ulcer duration and healing rate. The presence of venous ulceration infection, lipodermatosclerosis and dermatitis was determined in all patients.
In order to determine the dimensions of venous ulceration, measurements of the maximum diameter of the width and length of the ulceration were performed. Dimensions were determined by mapping a two-dimensional digital image to a polygonal mesh. The circumference of the ankle and calf was measured in a supine position, with minimum (ankle) and maximum (calf).
The definition of VLU healing was the point at which complete epithelialization of the limb occurred. Data on the quality of life measures were collected through a patient questionnaire at the beginning of treatment and 24 weeks later.
Randomization was computer generated. This research was approved by the Review Board of the Nis Clinical Centre (No. 2015-05-07) and patients in this research had given the informed consent.
The randomization of the patients was performed in relation to the degree of compression. The first group of patients received class III compression therapy with a compression pressure of 35–40 mm Hg (moderate pressure). The second group had an elastic bandage added to Class III compressive agents and the compressive pressure was > 45 mm Hg (high pressure).
Local treatment of VLUs involved the use of antibiotics and local antiseptics. The standard treatment regimen included wound debridement. Absorbent bandages were applied to the wet wounds. The dressings were changed between one and 7 days, based on the amount of wound exudate. After debridement and rewinding of the VLUs, bandage systems were applied. The first and second layers included gauze without any pressure. In the first group, for the third layer, tubulcus (tubular compression system) was used. Different tubulcus sizes (S, M, L, XL, and XXL) were used depending on the circumferences of the leg measured of the ankle, and the largest part of the calf. An additional elastic bandage was placed over the tubulcus for the patients of the second group. Elastic bandages were placed spirally with 50% overlap with the patient in a supine position and the foot in dorsiflexion. The bandages were characterized as long stretch (200% stretch). The applied elastic bandage was renewed after two and 4 months, and cleaned in between. The compression system was placed on the patient’s leg every morning, and the bandages were removed during the night. Before applying the compression bandage, patients were educated by a competent practitioner.
In a group of patients with healed venous ulcerations, we advised to continue using tubulcus in order to prevent recurrence.
Quality of life measures included:
Quality of Life Index (QL) consists of five items that measure the domains of activity, psychological perspective, health support, and daily life. The QL index was developed for the chronically ill patients. A large number of studies conducted in the United States have shown good validity and reliability of this index [10, 11]. The study by Spitzer et al. [10] showed correlations of 0.74–0.84 for reliability and coefficient a = 0.77 for internal consistency among evaluators.
Numeric Pain Rating Scale (NPRS) is one of the most commonly used scales for measuring pain intensity. The advantage of this scale is reflected in its simplicity. NPRS values range from 0 to 10, with 0 “absence of pain” and 10 “strongest pain imaginable”. The benefits of this scale are reflected in simplicity, sensitivity to small changes in pain, easy comprehensibility and repeatability [12].
Geriatric Depression Scale (GDS): advantage of this scale is that it can be easily filled in by the elderly [13]. The abbreviated version of this 15-item scale is very easy to use. A large number of studies have shown good reliability and high sensitivity (84%) and specificity (95%) among cognitively intact elderly people [14].
Statistical analysis
The data are presented in the form of arithmetic mean, standard deviation, and as absolute and relative numbers. If the distribution of data is normal, the comparison of continuous variables between groups was performed by t test. If the distribution of data did not satisfy the normality of the data, the comparison of continuous variables between groups was performed by Mann-Whitey test. The χ2 test was used to compare categorical features. Cox regression analysis was used to assess risk factors for healing. The Kaplan-Meier curve and log rank test were used to estimate healing by type of compression. The hypothesis was tested with a significance threshold of p < 0.05. Data were analysed using R software (Version 2.15.2, Tubulcus; Laboratoires Innothera, Arcueil, France).
Results
Overall, 139 patients were assessed for eligibility. One hundred and twenty-three patients were randomized. We analysed 116 patients. The first group consisted of 56 patients with a moderate pressure compressive therapy, while the second group was composed of 60 patients with a high pressure compressive therapy. For the patient CONSORT [15] flow diagram see Figure 1.
Figure 1
Flow diagram of the progress through the phases of a parallel randomized trial: (A) group with a moderate pressure and (B) group with a high pressure

The study included 116 patients, 52 (44.8%) male patients and 64 (55.2%) female patients. The average age of the examined population was 62.87 ±10.86 (min. 42 years, max. 85 years). Age and sex did not differ statistically significantly in relation to the type of compression (p = 0.441 and p = 0.822, respectively). The calf circumference was statistically significantly smaller (p = 0.033), and the size of the ulcer was statistically significantly larger in the high pressure compression group (p = 0.038). Lipodermatosclerosis was statistically significantly more common in the high pressure compression group (55.0% vs. 33.9%, p = 0.036). Healing at 24 weeks was statistically significantly more common in patients in the high pressure compression group (55.0% vs. 32.1%, p = 0.022) (Table 1).
Table 1
Demographic and clinical characteristics in relation to the level of compression
Quality of life, GDS scores and NPRS scores at the beginning of the follow-up period were equalized between groups (p = 0.080, p = 0.071; p = 0.078). In patients with high compression, there was a statistically significant increase in QL scores (p = 0.005), decrease in GDS scores (p = 0.040) and NPRS scores (p = 0.002) during 24 weeks. In patients with moderate compression, during 24 weeks, there was a statistically significant increase in QL scores (p = 0.013) (Table 2).
Table 2
QL, GDS and NPRS in the follow-up period in relation to the type of compression
| Score | Sub-bandage pressure | P-value1 | |
|---|---|---|---|
| High pressure | Moderate pressure | ||
| QL1 at baseline | 5.50 ±1.67 | 5.02 ±1.41 | 0.080 |
| QL1 at 24 weeks | 5.78 ±1.92 | 5.38 ±1.84 | 0.323 |
| P-value | 0.005 | 0.013 | |
| GDS2 at baseline | 7.72 ±2.90 | 6.82 ±1.84 | 0.071 |
| GDS2 at 24 weeks | 7.02 ±3.06 | 6.29 ±1.51 | 0.005 |
| P-value | 0.040 | 0.099 | |
| NRS3 at baseline | 4.72 ±1.09 | 4.36 ±0.92 | 0.078 |
| NRS3 at 24 weeks | 4.33 ±1.05 | 4.11 ±0.93 | 0.155 |
| P-value | 0.002 | 0.518 | |
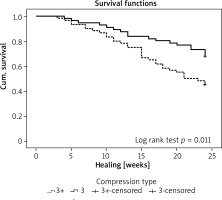
Kaplan-Meier curve shows a statistically significant difference in healing with respect to the type of compression (p = 0.011) (Figure 2).
Multivariate Cox regression analysis showed that statistically significant healing predictors were duration of the ulcer (OR = 0.921), size of the ulcer (OR = 0.786, p < 0.001), high sub-bandage pressure (OR = 5.603, p < 0.001), and the presence of infection (OR = 0.211, p = 0.006) (Table 3).
Table 3
Association of demographic and clinical parameters with healing (Cox regression analysis – multivariable model)
It was determined that the quality of life after 24 weeks is affected by the size of the ulcer (p = 0.007), duration of the ulcer (p = 0.049) and the presence of infections (p < 0.001) (Table 4).
Table 4
Risk factors that affect the quality of life after 24 weeks
Discussion
A large number of different research studies deal with the issues of treatment and care of patients with chronic diseases. One of the very important questions that arise is how health professionals can influence the improvement of the well-being and life of patients with chronic diseases [16].
Compression therapy, which is used as the gold standard in the treatment of VLUs, in a certain number of patients can lead to limitations in daily activity and social activity. Numerous studies [17] dealing with this problem have shown that a large number of patients with VLUs believe that health professionals are not always qualified enough to provide them with adequate treatment. These studies have shown that these professionals do not always empathize with their patients’ situation.
Compression bandage, which is used in the treatment of patients with VLUs, has a positive effect on wound healing, improves the quality of life, increases patient mobility and reduces pain. It should be noted that in addition to the correct choice of compression systems, it is very important to determine the compressive categories. There are a number of guides [18] that recommend the distribution of the bandage pressure, the site of bandage application on the extremity and the position of the extremity. If inadequately compressed bandage is applied, it can cause serious complications and worsen the course and disease outcome.
If compression therapy is adequately applied, venous ulcers will heal in 40% to 95% of cases [19–21]. However, despite the application of adequate therapy, venous ulcers will not heal in a relatively large number of patients. This is a very big health, social and economic problem because there is a relatively large group of patients that doctors fail to adequately treat.
The size and duration of venous ulcers have been identified in a large number of studies as the most significant risk factors for delayed healing of VLUs [22–24]. Studies have indicated that deep vein involvement [25], age [25] and history of DVT [26] are risk factors for slow VLU healing. Patients’ sex [25], general mobility [26], ankle movement [25], venous surgery [27], ABPI, 50% of wound covered with fibrin [25] and hip/knee replacement surgery [28] are also factors that slow down the healing process. Despite the clear correlation of these factors with delayed VLU healing, studies have shown the importance of other parameters as well as their interconnectedness [23, 24].
A randomized, open, prospective, single-centre study [22] examined how different compression strength affects the degree and rate of VLU healing. The results of the study showed the need to determine the compression system in relation to individual leg characteristics. In this study, a higher pressure led to a faster healing rate of venous ulcers.
A study by Finlayson et al. [7] compared the healing rate and quality of life for patients with VLUs relative to the compression system applied. A four-layer compression bandage system compared to Class 3 compression hosiery leads to significantly faster healing of VLUs after 24 weeks of treatment. The results of the study did not show statistically significant differences between the two groups in the proportions of healed patients in relation to the applied compression therapy. Quality of life and intensity of pain did not show a statistically significant difference between the examined groups.
A number of studies have shown the advantage of using multicomponent compression systems over single-component systems because their application achieves a higher degree of compression. Research has also shown a better effect of high-compression stocking systems compared to short-stretch bandages [29].
Our study showed that the healing rate was statistically significantly higher in the group with a higher pressure applied compared to the moderate pressure (p = 0.034). Patients with VLUs in which a high pressure was applied healed considerably faster in relation to VLUs in which a moderate pressure was applied (p = 0.008).
In patients with VLUs, pain is very often present in everyday life. The intensity of pain varied among patients from mild to so severe that patients also considered suicide [30–32]. Studies have shown that pain was present in about 74% of patients with VLUs, while patients described pain as “moderate to severe” in 56% of cases [32].
Pain that occurs in patients with VLUs leads to a decrease in physical activity or walking [33]. Pain was very common in patients with leg and ankle oedema [34]. Productive activities were disrupted due to the presence of pain in these patients [35]. These patients were less likely to come out due to the presence of pain and feelings of discomfort although they remained in contact with their environment [36]. In patients with VLUs, pain mostly occurred at night [37], leading to sleep problems [38]. Feelings of discomfort and pain did not allow some patients to fall asleep, while others woke up after a short sleep after the cessation of analgesics. Patients have characterized the intensity of this pain as “unbearable pain” or “tear-inducing pain” [39, 40].
Patients with VLUs also have problems with social life in terms of limited leisure activities, as well as reduced social contacts with friends and family members [41].
Various psychological problems also occur in these patients. In these patients, negative emotional reactions occur with the appearance of the feeling that the disease controls them. Most patients had a pessimistic vision of the future and a negative experience in their body image [41].
Bad mood and depression are present in patients with VLUs [31, 32]. Studies have shown a direct link between depression and the treatment of these patients [42]. Mood improves in patients in proportion to the cure [30]. Anxiety and depression are present in a large number of patients with VLUs, which is directly correlated with the number of experienced venous ulcers [43–45].
Previous studies have shown in patients with VLUs, the following factors and physical complaints that lead to QL worsening: unpleasantly smelling wound [46, 47], wound pain [48], pain and itchiness of the skin [47], exudate [48] and joint deformation [49, 50].
Our study showed that QL, GDS scores and NPRS scores at the beginning of the follow-up period were equalized among groups. During the 24-week treatment period in the high compression group, there was a statistically significant increase in QL scores, decrease in GDS scores and NPRS scores. In patients with moderate compressions during 24 weeks’ treatment, there is a statistically significant increase in QL scores, while there was no statistically significant decrease in GDS scores and NPRS scores. The reason for this result lies in the fact that a larger number of ulcers healed in the group of patients with high compression and they had an improvement in QL, reducing the severity of pain and an improvement in the psychological domain.
Our study singled out as the most significant risk factors that affect the quality of life after 24 weeks – the size of the ulcer, duration of the ulcer and the presence of infections. This can be explained by the fact that the mentioned parameters represent statistically significant predictors in the healing rate. In patients who experienced healing of venous ulcers, QL improved, pain levels and depressive disorders decreased.
Conclusions
This study showed that patients with VLUs who received a high pressure, healed considerably faster compared to the group of patients to whom a moderate pressure was applied. The application of compression therapy leads to VLU healing, but when a high pressure was applied, there was a statistically significant increase in QL scores, decrease in GDS scores and NPRS scores compared to the group of patients to whom a moderate pressure was applied.