Introduction
According to the data of the European Agency for Safety and Health at Work from 2008, dermatoses accounted for as much as 7% of the total percentage of diagnosed occupational diseases [1]. The most common of these is contact dermatitis (CD), which develops both from allergies (allergic contact dermatitis – ACD) and from irritants (irritant contact dermatitis – ICD). This disease is not just an aesthetic problem. It leads to the impairment of the physical and mental health of employees, which often results in the inability to continue the current job or the necessity to start a new one. In addition, it leads to financial problems of these subjects, and having in mind the scale of this phenomenon, it has undoubtedly significant socio-economic consequences [2]. The gold standard of ACD diagnostics is the so-called “patch tests” [3]. Other additional tests, such as intradermal tests, “practical tests” or provocative oral tests, are also helpful. However, the professionals also have to keep in mind to precisely collect the medical history. Combining it with – even seemingly irrelevant – information about the patient’s daily habits, allows for an appropriate selection of the range of haptens in the patch tests performed. Collecting a comprehensive history requires knowledge about the most common allergenic factors in specific occupational groups, as well as about selected disease symptoms with their most frequent location. Most of the available research in the literature focuses on these issues [4–7]. However, there are no studies that would correlate the incidence of given allergens with a given workplace or work environment.
Aim
To maximize and facilitate the work of a dermatologist, an original, innovative questionnaire was designed to assess occupational exposure to the risk factors of contact allergy in the work environment of health professionals. Identification of allergens occurring in the work environment should allow for optimizing the frequency of preventive examinations and reducing the risk of exposure by the need to use personal protective equipment, and possibly also removing substances with high allergenic potential from the direct environment of the hospital workers. It will also enable the identification of a group of exposed people and thus the development of algorithms of primary and secondary prevention of allergic reactions among healthcare professionals.
Material and methods
We design a proprietary questionnaire consisting of 3 parts considering: (1) workplace (15 questions), (2) family interview (2 questions), and (3) medical history (36 questions). On its basis, a scale about the risk of occupational diseases of the skin among healthcare workers was created (OSDES-49) (Table 1).
Table 1
Scale of the level of exposure to occupational diseases of the skin consisting of 49 points (OSDES-49)
To assess the level of potential development of contact allergy, the sum of points obtained by each of the respondents for affirmative responses to 47 items (yes – 1 point, no – 0 points) and for the frequency responses (not present – 0 points, occasionally – 0.25 points, regularly, but less than once a month – 0.5 points, regularly, but at least once a week – 0.75 points, regularly at least once a week, but the lesions cease after a weekend or break from work – 1 point) were used in this case. In total, each of the surveyed employees could obtain a score ranging from 0 (the lowest exposure) to 49 points (the maximum exposure to contact allergens).
To test the reliability of the scale items, the internal consistency method of the scale was used. It was assumed that the individual items of the scale should be correlated with the total score of at least 0.4 (Kleine’s criterion) and the Cronbach’s coefficient should be higher than 0.7 (Nunnally’s criterion). The validation of the proposed scale was based on the results of a survey in a group of 230 hospital workers from the Specialised Medical Centre (SCM) in Polanica-Zdrój in Poland. To take part in the survey, the worker needed to meet the following criteria: employment in the SCM, informed consent, being above 18 years old, Polish-speaking, and undergoing preliminary, periodic, and control medical examinations performed by a departmental doctor between March and December 2017. The exclusion criteria were: pregnancy and breastfeeding; in 4 weeks preceding the examination: disseminated or generalized eczema, acute eczema, occurring of eczema in the planned area of testing, local steroid or calcineurin inhibitor treatment in the planned area of testing; immunosuppression, use of the solarium, phototherapy or sun-bathing; in 2 weeks preceding of the examination: infectious diseases and fever, antibiotic therapy. Among all 682 workers of the SCM, 230 met the following inclusion criteria. The percentage of women included in the research was much higher than men (88.3% vs. 11.7%). This ratio arises from our hospital employment’s sex structure and domination of female workers. According to the work position, workers were also divided into four groups: Doctors (n = 21); Nurses, midwives, rescuers, orderlies (n = 162); Medical analysts, pharmacists (n = 17);Others: technical staff, medical secretaries, administration staff (n = 30). In 103 (44.8%) employees (93 women and 10 men) who agreed, the patch tests were performed and interpreted to check the correlation between OSDES-16 as a screening tool with the clinical picture. According to the results of our research, the risk of exposure depends on factors such as work position, and job seniority. However, due to the complex and extensive analysis of the data, we dedicated a separate paper to the detailed results. We want to emphasise that the aim of this study is to measure whether the clinician is able to take the medical history easier and faster with the usage of OSDES-16 in comparison to the longer and more time-consuming way with the usage of OSDES-49, or not.
During the preparation of the research, we followed the guidelines of the Good Clinical Practice and the Helsinki Declaration of the World Medical Association of 2008 – “Ethical Principles for Medical Research Involving Human Subjects”. All patients participating in the study were informed about the goals, methods, and possible test results of the study. Patients before being included in the study were asked to sign their informed consent to participate in the study and give written consent to the processing of personal data. The research obtained the approval of the Bioethics Committee of the Wroclaw Medical University – decision no. KB - 178/2017.
Results
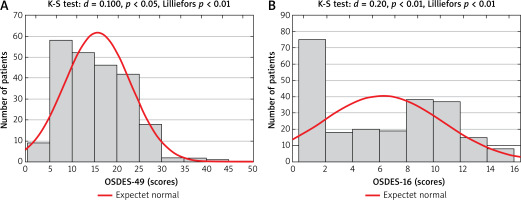
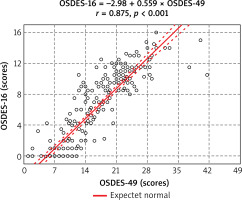
For the scale consisting of 49 items, the mean value was M = 15.68 (standard deviation – SD = 7.45 with Cronbach’s a = 0.891, and the mean value of the correlation coefficient r = 0.151). Following the previously adopted criteria for determining the reliability of the scale items, after eliminating the items that did not meet the Kleine’s and Nunnally’s criteria, a final scale consisting of only 16 items was obtained. For a scale of 16 items, the average in the studied group of SCM employees was M = 5.89 (SD = 4.76; Cronbach’s a = 0.91, and the mean value of the correlation coefficient r = 0.397). Assessment of the level of the risk to develop occupational skin diseases using a questionnaire consisting of 49 items (OSDES-49) strongly correlated with the assessment using a questionnaire consisting of only 16 items (OSDES-16) (Table 2). Spearman’s rank correlation coefficient was rho = 0.85 (p < 0.001), therefore, possible further screening can be limited in the future to a questionnaire consisting of only 16 items (Figure 1). The high level of compliance between the assessments of both scales and the possibility of replacing the questionnaire consisting of 49 items with a questionnaire consisting of 16 items in screening tests is evidenced by the high value of the k Cohen coefficient. In the group of 230 employees, this coefficient was k = 0.639, and its 95% confidence interval ranged from 0.556 to 0.722 (Figure 2).
Table 2
Scale of the level of exposure to occupational diseases of the skin consisting of 16 points (OSDES-16)
Discussion
Contact allergy is a significant medical and social problem. According to the results of studies from various countries [8–10], the incidence of atopic eczema is estimated at 5–23%, ACD at 17%, and irritant eczema at 13%. ACD is estimated to be the most common occupational disease of healthcare workers. According to the results of the study by Machovcowa et al. [11] on a group of 545 employees of this sector, ACD was responsible for 85% of diagnosed occupational diseases. The majority of patients (95%) were women. The prevalence and the relationship with various work environments make this disease a serious problem, not only clinically but also socially. If the effectiveness of identifying allergens associated with particular work environments could be improved, many methods could be introduced to secure employees, thus reducing the absence ratio, costs, and increasing work efficiency. The authors of the current study attempted to link the risk factors of allergic skin diseases with demographic data, job profile as well as medical and family history, and to design a questionnaire that could be used in the future as a screening test for ACD and optimize further diagnostic procedures. The gold standard in ACD diagnostics is patch tests, which are used as part of the so-called “standard series”. They are sets of allergens specific to a given geographical region (country, continent) and a specific social or professional group (depending on the profession, lifestyle and exposure factors). So far, “national” series have been used, which seems to be less justified in today’s times of globalization. It seems logical to replace them with “continental” series. The Polish Basic Series, effective from January 2014, contains 30 haptens. Its composition is adjusted to European standards and takes into account the specificity of the most common allergens in the Polish population [12]. Each country has a Basic Series that includes the most common haptens. Depending on the country or part of the world, it contains a different number of allergens. It should be noted that there is a universal tendency to expand the Basic Series. Depending on the result obtained from the Basic Series, diagnostics are extended to tests with additional haptens or provocation tests. It should be borne in mind that although the tests have a well-established position in diagnostics, due to certain limitations, they do not always give a reliable result [13]. Depending on the hapten, the sensitivity and specificity of typical patch tests are in the range of 70–80% [14]. Hence, it is very important to take the medical history properly. Our proprietary questionnaire helps collecting it correctly. According to the basis of indications, based on its result, test sets can be modified so that they are individually adjusted to each patient. The questionnaire includes questions about personal data, job characteristics, family history, and medical history. Based on the statistical analysis, it was determined that the short version of the questionnaire, containing 16 questions, turned out to be as sensitive in determining occupational exposure to contact allergy as its original, extended version, containing 49 questions. Therefore, OSDES-49 should be perceived as a point of departure and the OSDES-16 as a final and clinically useful screening tool that can be used by dermatologists. It will contribute to minimizing the risk of not taking the therapy in people affected by ACD, and also reducing the risk of implementing treatment in wrongly diagnosed, healthy people. OSDES-16 has no significance in predicting the occurrence of allergy diagnosed with the use of patch tests. The results of the above research are a valuable starting point for the study that we performed for checking the correlation between the OSDES-16 survey’s results and the clinical picture.
Conclusions
Both OSDES-49 and OSDES-16 have statistically proved efficacy in measuring the risk level of occupational skin diseases’ exposure. However, due to its simplified features, OSDES-16 is a more convenient tool in clinical practice than OSDES-49. The use of this scale reduces the time of initial diagnostics. Although we performed research that demonstrates the effectiveness of this scale in practice, we decided to mention just samples of its samples in this article, and to elaborate on the results in a separate paper, that we will submit in the nearest future.