Introduction
Stress is a factor with an influence on patients’ mental, physical and social balance. The presence of many stressors may interfere with homeostasis and thereby lead to allostasis as adaptive mechanisms [1]. The effect of psychological stress on men is dependent on their positive or negative perception of the situations experienced, and on their behaviours and genetic predisposition. Stress as a stimulus is analysed by the central nervous system and changed into biological responses by stimulation of the hypothalamus and pituitary activation. Its consequence is the release of neurotransmitters which act on the body. Stress manifests in a variety of ways: deriving from positive or negative stimuli, chronic or acute, conscious or unconscious and escapable or inescapable [1, 2].
The impact of stress on health conditions and disease activation has been investigated in numerous studies. The skin, as the largest organ, appears to respond to stress because many dermatoses are considered to be associated with the patient’s mental status. The skin therefore reacts to a variety of stressors, including psychological stress. In this complex interaction induced by stress, immunological cells, hormones, neurotransmitters and their receptors are likely to play an important role in negative effects on the skin. Many of these relationships have not been fully investigated, and nor has the effect of stress on individual dermatological diseases. One example of such a disease is psoriasis [3].
Stress can activate complex immune reactions in the skin: the nervous and immunological systems can receive, transmit and respond to many signals, induce memory and influence other tissues. Furthermore, the immunological and neuroendocrine systems also share numerous mediators that activate and modulate the activity of immunocompetent cells in the skin. Additionally, pro-inflammatory cytokines synthesised as a response to stress stimulate neuroendogenic inflammation and the central glandular system, which strengthens the reaction to the stressor. It is now known that in chronic stress, neurotransmitter stimulation and the secretion of neurotransmitters and selected cytokines, e.g. interferon-γ (IFN-γ), contribute to the disruption of skin homeostasis, including the impairment of endogenous cortisol secretion [4].
Many studies have confirmed a positive relationship between high stress levels and a diverse range of skin conditions and illnesses. One such condition is psoriasis, in which hypothalamic-pituitary-adrenal axis impairment is manifested [4].
Epidemiology and pathomechanism of psoriasis
Psoriasis is a common immune-mediated, chronic inflammatory disease, causing adverse effects on patients’ quality of life and disease burden. Worldwide, psoriasis has a prevalence of approximately 1.99% in East Asia, 1.92% in Western Europe, and 1.10% in high-income Latin American countries. The underlying pathogenesis of psoriasis results from an interplay between various genetic and environmental factors [5]. Psoriasis occurs equally in both males and females and has a bimodal age of peak occurrence: between 20–30 and 60–70.
Environmental factors triggering psoriasis may vary by patient, including stressful events, physical trauma, streptococcal infections and some medications, although there is also a significant genetic component [6].
The overall pathogenesis of psoriasis can be divided into initiation and maintenance phases [7].
The initiation phase is primarily mediated by the effect of antimicrobial peptides (AMPs) on dendritic cells. Keratinocytes release AMPs in response to injury, the primary AMPs involved in the pathogenesis of psoriasis containing LL37, β-defensins, and S100 proteins. The function of LL37 is mediated by its differential binding to DNA or RNA. After binding to DNA, LL37 stimulates toll-like receptor (TLR) 9 to activate plasmacytoid dendritic cells (pDCs) which, when activated, produce type I interferons, for example, IFN-α and IFN-β, which then enable myeloid dendritic cells (mDCs) to start the maturation and differentiation of type 1 helper T cells (Th1) and type 17 helper T cells (Th17). Th1 cells produce IFN-γ and TNF-α, and Th17 cells produce IL-17, IL-22, and TNF-α. Activated mDCs can also migrate to lymph nodes, where they directly secrete various inflammatory cytokines, such as TNF-α, IL-23 and IL-12. IL-23 facilitates Th17 and Th22 cell survival and proliferation, whilst IL-12 stimulates naive T cell differentiation to Th1 cell differentiation. The essential inflammatory cytokine in psoriasis is TNF-α, which is produced by Th1, and Th17 cells. Following activation, mDCs can continue to mobilise dendritic cells, thus leading to an autoinflammatory loop. After binding to RNA, LL37 stimulates TLR7 and TLR8, which activate pDCs and mDCs. Finally, LL37 bound to RNA can also boost slan+ monocytes, which secrete TNF-α and IL-23.
β-defensin is another important AMP in psoriasis that acts similarly to LL37, whilst S100 acts to recruit neutrophils, which are commonly present at high levels in psoriatic lesions [5]. Through activation of pDCs, it increases the recognition of self-RNA and self-DNA.
The maintenance phase of psoriasis is mainly mediated by various helper T cell subtypes and their cytokines: the TNF-α/IL-23/IL-17 axis is relevant in the pathogenesis of psoriasis, whilst the IL-23/IL-17 inflammatory cascade plays a particularly key role. Meanwhile, mDCs produce IL-23, which is found in significant amounts in psoriatic lesions, and maintains Th17 cells – they are a major source of IL-17, production of which can also occur independently of IL-23. A hypothesis describes the involvement of γδ T cell, group 3 innate lymphoid cells (ILC3s) and natural killer T (NKT) cells in the production of IL-17 by the innate immune system. γδ T cells specifically contain a TCR consisting of an γ and δ chain, contrary to the classical T cell α and β chain, and are found in increased numbers in psoriatic skin lesions. However, according to high-throughput TCR screening, γδ T cells comprise less than 1% of the total T cells in psoriatic lesions. Since ILC3s positive for the natural cytotoxicity receptor (NCR+) are also found in significant amounts in psoriatic lesions, in vitro stimulation of ILC NCR+ leads to IL-22 production, which is involved in the pathogenesis of psoriasis and increases the production of S100 AMPs. Although the role of NKT cells is not yet fully understood, NKT cells are found in psoriatic skin and decrease after psoriasis treatment. Moreover, transplantation of NKT cells is known to lead to the induction of psoriasis, suggesting their involvement in its pathogenesis [5].
IL-17 acts through two separate mechanisms [5]. The first mechanism depends on the cytoplasmic adaptor protein ACT1 which interacts with TNF receptor-associated factor (TRAF) 6, which subsequently activates transcription factor NF-κB. This is followed by the initiation of transcription of inflammatory genes and the activation of p38 mitogen-activated protein kinases, which help stabilise mRNA for cytokines and chemokines involved in psoriasis [5]. The second mechanism is independent of ACT1. This pathway involves the Janus kinase (JAK)-signal transduction and activator of transcription (STAT). JAKs are non-receptor tyrosine kinases involved in cytokine signal transduction; their function is dependent on specific cytokine binding. The JAKs family includes JAK 1, JAK 2, JAK 3 and tyrosine kinase 2 (TYK2). The receptor is oligomerised by forming a bond between the cytokine ligand, and the underlying molecular pathway is initiated by forming a bond between the cytokine ligand and the receptor. This therefore causes the receptor-associated JAK to separate, leading to JAK activation and phosphorylation. After JAK activation, it can form a homodimer, combining with a member of the same family, or a heterodimer, combining with a JAK from a different family. JAK dimerisation enables STAT activation, which then contributes to STAT dimerisation and allows STAT to translocate to the nucleus to regulate transcription, further contributing to the inflammatory pathogenesis of psoriasis [5].
Two STAT molecules, STAT1 and STAT3, are crucial in the pathogenesis of psoriasis. STAT1 transduces signals for type I and II interferons through JAK1 and JAK2. Through signal transduction, IFN-y makes keratinocytes more sensitive, and this contributes to the penetration of inflammatory cells into psoriatic lesions. For its part, STAT3 is responsible for the induction and differentiation of Th17 cells through different pathways. STAT3 can be activated by JAK2/TYK2, induced by IL-23, JAK1/JAK2, and JAK1/TYK2, both caused by IL-6. A transcription factor and activated STAT translocate to the nucleus to alter transcription so that gene expression can be controlled. All this leads to promotion of the inflammatory pathogenesis of psoriasis [5].
Clinical presentation of psoriasis
The clinical features of psoriasis differ depending on the variant. Variants include plaque psoriasis, guttate psoriasis, erythrodermic psoriasis and pustular psoriasis, although most variants of psoriasis share the three key clinical features of erythema, thickening and scale [8].
The symptoms of psoriasis vary considerably from patient to patient, ranging from single to generalised lesions with different localisation.
While the primary manifestation of the disease is in skin lesions, it may also be accompanied by psoriatic arthritis. There is also an increased risk of cardiovascular disease, metabolic syndrome, diabetes, chronic kidney disease, certain cancers and inflammatory bowel disease [9].
Psoriasis occurs in several distinct locations. Typical sites of occurrence are elbows and knees, which are associated with the exposure of these areas to trauma. The scalp is also a common site of localisation [10], along with skin folds and areas with increased sweating. In these areas, erythema predominates and scales are usually absent. In more than 30% of patients, psoriasis affects genital areas, and just under 30% occurs on the face, whilst lesions are often localised on hands and feet. Nail changes occur in 30–50% of patients, involving multiple nails, more often on hands than feet [11].
The diagnosis of psoriasis in children is more complex than in adults, where the clinical picture is often unquestionable. Children have the same clinical forms of the disease as adults, but the localisation and morphology of the lesions differ between age groups very often. The most important clinical features differentiating child from adult psoriasis include more frequent involvement of the face, auricles, volar regions and the occurrence of exudative psoriasis [12].
Stress in psoriasis
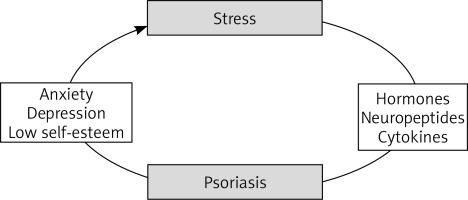
Studies which analyse the role of stress in dermatoses usually divide it into three main categories: environmental, physiological and psychological. For individuals with a genetic predisposition to psoriasis, activation of any of these may result in the first appearance or worsening of existing psoriasis [13]. It has been shown that 40-80% of psoriasis exacerbations can be attributed to psychosocial factors [14]. Devrimci-Ozguven et al. [15] reported that psychological stress was related to the onset of lesions in 40–80% of psoriasis patients. Meanwhile, Farber et al. [16] surveyed 2,144 patients in the United States, 40% of whom reported that their psoriasis first occurred during “worry“ periods, while 37% said that the disease worsened during such periods.
The major pathways by which stress influences pathological skin changes include stress-induced dysregulation of the hypothalamic-pituitary-adrenal axis, stress-induced immunomodulation, and neurally activated skin neuropeptide imbalance [14].
It is possible that, in response to contact with a stimulus (e.g. a stressor), activated keratinocytes produce and secrete various cytokines and chemokines that regulate inflammatory responses in the skin capable of stimulating the onset of psoriasis in predisposed patients. Therefore, activated keratinocytes produce cytokines such as the granulocyte-macrophage colony-stimulating factor, interleukin (IL)-1α, IL-6 and interferon-g. Keratinocyte-derived cytokines enhance the migratory activity of Langerhans cells (antigen-presenting cells); these cells then migrate to the area of the lymph nodes, where they stimulate the replication of specific T cells, which later penetrate the target area of the skin via endothelial adhesive molecules on the endothelial cells of skin blood vessels attracted by chemokines [17]. Keratinocyte-derived cytokines act through appropriate skin cell receptors and, along with keratinocyte-derived chemokines, have numerous effects on inflammatory cell migration, keratinocyte proliferation and differentiation, and on the production of other cytokines. Among the cytokines secreted by keratinocytes, IL-1 and IL-6 were the most characterised. Some studies have suggested that the skin is a separate compartment of the neuroendocrine system with autoregulatory properties, composed of locally produced mediators whose primary function is local control and response to adverse effects. The neuroendocrine substances of the skin come partly from the nerve fibres that innervate the skin and partly from skin cells that can produce and secrete humoral signalling molecules (neurotransmitters, neuropeptides and hormones). These skin cell signalling products are analogous to the neurotransmitters, neuropeptides, and HPA axis hormones [17].
CRH is distinguished as the primary proopiomelanocortin release hormone (POMC), which is a pre-prohormone, a precursor (in the pituitary and other organs and skin) to a group of pharmacologically diverse neuropeptides and hormones, including ACTH, opioid peptides and melanotropin. Thus, parcel neurons of the hypothalamus often release CRH (2–3 pulses every 2 h) into the pituitary portal system. Therefore, ACTH promotes the synthesis and release of glucocorticoids, mineral corticosteroids and androgenic steroids in the adrenal cortex. Glucocorticosteroids are synthesised in the adrenal cortex (under the influence of pituitary ACTH), affecting immunity and inhibiting all endocrine systems that are not essential for the body’s basic functioning; after disturbance, they stimulate the restoration of homeostasis. Glucocorticoid hormones act through their intracellular tissue receptors (glucocorticoid and mineralocorticoid) [17].
Notably, the skin produces all peptide hormones that are part of the HPA axis, including the major stress response system. Among the key hormones involved in the classical neuroendocrine pathways are the hypothalamus CRH and related urocortin, most of which exhibit the same functions in response to stress [17].
The main pituitary hormones in the skin are POMC and neuropeptides resulting from its cleavage. In addition to pituitary hormones, POMC and its degrading peptide hormones have been found in the skin. They are considered key in regulating growth and differentiation as well as in the immunomodulatory effect of skin cells. Therefore, the expression of POMC in the skin is under neuroendocrine control. Healthy skin contains low levels of POMC peptides, while elevated POMC peptides are found in various skin diseases/conditions (e.g. inflammation (atopic dermatitis), hyper keratinisation (psoriasis), skin cancers (melanoma, epidermal and other cancers) and skin lesions under the influence of UV radiation) [17].
Neuropeptides have mitogenic effects and can modulate the body’s immune response. Most fibres containing neuropeptides are localised around hair glands and blood vessels and in the papillary layer of the skin. The most important skin neuropeptides are substance P, vasoactive intestinal peptide, calcitonin gene related peptide, neuropeptide Y, somatostatin, neurotensin, neurokinin A. These substances have regulatory roles in the nervous and immune systems. Farber et al. present a psychoneuroimmunological theory of psoriatic lesion formation, stating that under stress there is an increase in substance P in the skin, brain, and blood and a substance P-induced neurogenic inflammation. The authors noted the symmetrical occurrence of psoriatic lesions and the resolution of lesions after transverse transection of peripheral nerves due to various surgical procedures, and the worsening of disease symptoms under the influence of emotional factors [15, 16].
The physical and psychological impact of psoriasis may affect intimate areas of the patient’s life, such as emotional well-being, personal relations, sexuality, and interpersonal relations (family, work and community). The economic impact of illness increases with the severity of psoriasis and the associated psychosocial impact [18].
In this regard, the visibility of lesions affects the body image of the patients. More than 40% of psoriasis cases appear before the age of 30, causing stigmatisation and affecting psychological functioning. Psoriasis also has consequences for marital relationships, because of emotional disturbances suffered by patients, their low self-esteem, and limited participation in family activities [19].
The burden of disability has been estimated to be comparable to other severe chronic conditions, such as heart failure, chronic obstructive pulmonary disease and cancer [20].
Psoriasis and mental diseases
In psychodermatology, psoriasis is included both in the group of dermatological diseases, in which the psychophysiological background plays a key role, and in dermatoses being a potential source of emotional disturbances or being a trigger for the development of secondary mental disorders [21]. The prevalence of psychiatric disorders among dermatological patients is higher than that of the general population and is estimated at 30–60%. Typically, patients suffer from affective disorders, primarily elevated anxiety and episodes of anxious depression. Lesions that are extensive or localised in essential areas of the body for self-image can significantly impact the onset of depressive symptoms [22]. A study by Parafianowicz and Sicińska [23] that included 32 patients with psoriasis found that psychiatric disorders in this group were 4 times more common than in patients with other skin diseases.
The relationship between depression and psoriasis appears to be bilateral. Depression may be primary or secondary to psoriasis, and both conditions may modulate each other’s course: preceding the onset of first symptoms and inducing subsequent relapses and exacerbations. Depression and higher self-rated psoriasis severity may result in the emergence of suicidal thoughts and tendencies. The role of stressful life experiences as one of the triggers of many disorders, including depression and psoriasis, is also well established [24]. In a study by Rapp et al. [25], a quarter of all respondents experienced a death wish due to the disease at least once in their lives, 8% continued to think that life was not worth living because of psoriasis, and for 1.6% psoriasis was the reason for an attempt to maim or to bargain for life (Figure 1).
A holistic approach to treatment of psoriasis
Due to the role of genetic background, it is impossible to cure completely and avoid all exacerbations of psoriasis. Furthermore, treatment is often empirical due to the fact that the exact pathogenesis of psoriasis is still unknown. Different topical and systemic medications are used to remove scales, slow down the keratinocyte conversion rate, improve cell differentiation and inhibit inflammation. We also have modern solutions that affect comprehensive immune reactions. The therapeutic method should provide durable disease control and allows for the minimisation of its negative impact on the patient’s life, whilst drug adverse events should be limited [26].
The introduction of biologic drugs ushered in a new era in the treatment of severe forms of psoriasis and enabled many patients to achieve long periods of remission from the disease and a consequently improved quality of life. Comparative studies on the influence of biological therapy on serum and salivary stress parameters, as well as on the subjective assessment of the quality of life in these patients, are currently in progress. The authors’ preliminary observations indicate a statistically significant relation between salivary concentration of cortisol, nerve growth factor (NGF) and substance P and stress level in patients before and during biological treatment.
Despite advances in the treatment of psoriasis, it is essential not to focus only on pharmacotherapy. Many patients’ psychological problems, feelings of alienation and rejection have drawn attention to the usefulness of psychotherapy as an additional supportive form of treatment. Borzęcki and Cielica [24] emphasise the necessity of closer psychological contact between patients and doctors than in the treatment of other skin diseases. Psoriasis patients seem, therefore, to be one of the patient types requiring “special care”. The authors’ observations suggest that pharmacological treatment in combination with psychological care in these patients brings greater improvement in the quality of life than isolated pharmacological therapy.
A significant issue in the overall therapy of psoriasis is the spreading of knowledge and tolerance for psoriasis patients in the society, with attention given to emphasising that psoriasis is not a contagious disease. Support groups are helpful not only for the patients themselves, but also for children with psoriasis and their parents. It is essential to teach them techniques to reduce the stress experienced. Basińska and Kasprzak [27] emphasise the advisability of psychological support for patients with psoriasis aimed at modelling coping strategies and building positive attitudes in patients. These skills may allow the patient to adapt to the disease, actively participate in the treatment process and increase the assessment of their quality of life.
All of these factors suggest that such patients require tailored management using psoriasis therapies and psychological support – the right treatment for suitable patients at the right time.
Conclusions
A comprehensive view of the patient with psoriasis, not only from the point of view of skin disease, but as a result of a wide impact of stress, including low self-esteem and inappropriate social perception may have a key influence on improvement of quality of life of these patients. Far-reaching measures should be taken to make the treatment of patients with psoriasis a holistic therapy.