Rheumatoid arthritis (RA) is common autoimmune autoinflammatory arthritis. According to the European and American guidelines for the RA treatment, biologic agents are recommended [1, 2]. Although biological drugs have demonstrated safety and efficacy in clinical trials, an increasing number of cases of autoimmune processes triggered by biological treatment has been reported. According to the last update of the Study Group of Biological Agents in Autoimmune Diseases (BIOGEAS) Registry which consists of 12,731 cases, acute lupus erythematosus and vasculitis are the most frequent systemic autoimmune diseases induced by biological therapies [3]. Among 291 cases of vasculitis, only in 2 patients’ vasculitis was caused by tocilizumab [4, 5].
We report another case of vasculitis induced by tocilizumab in a patient with RA but the first one in which granulomatous vasculitis was diagnosed in skin biopsy. Moreover, a review of the literature has not revealed to date a case report of cutaneous actinomycosis in a patient with RA during treatment with tocilizumab. Tocilizumab is a humanized monoclonal anti-interleukin-6 (anti-IL6) receptor antibody. IL-6 plays a significant role in the innate immune response, so inhibition of this cytokine might cause an increasing risk of adverse events including infections [6]. Tocilizumab might mask signs of active infection such as fever or an elevated C-reactive protein (CRP) level which makes early diagnosis of the infectious disease more difficult.
A 67-year-old Polish woman had been suffering from RA for 20 years. She had a history of treatment with many different biologic agents and she was temporarily treated with glucocorticosteroids. She was initially treated with infliximab and etanercept. That therapy was switched to rituximab for 2 years (2007–2009). For 3 years (2014–2017) she was treated with sirukumab. That therapy was stopped because of the decision of the Arthritis Advisory Committee of the U.S. Food and Drug Administration (FDA) not to recommend using of sirukumab for the treatment of adults with moderate to severe RA because of the sirukumab benefit-to-risk profile. Six months later, in September 2018, the treatment was changed to tocilizumab with methylprednisolone 8 mg/day.
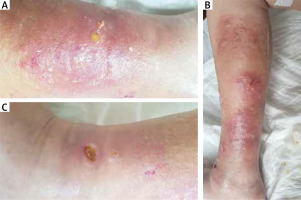
In January 2019, she was admitted to the Department of Rheumatology because of worsening joint pain and soft tissue infection. During hospitalization she presented with blisters filled with yellow fluid, ulcerations covered with necrotic tissue and sero-purulent exudate as well as nodules located on her left lower extremity. Additionally, on her right lower leg she developed redness and swelling accompanied by warmth as well as ulceration.
The patient was consulted by a dermatologist, surgeon, angiologist and microbiologist. They diagnosed erysipelas of the right lower extremity whereas culture confirmed soft tissue infection of the left lower leg caused by Staphylococcus aureus. The therapy was extended by ceftriaxone, cefazolin and clindamycin.
Results of diagnostic tests: ANA was negative, Quantiferon TB Gold was positive. She was consulted by a pulmonologist who decided that the treatment was not needed.
Ultrasound examination of the right lower leg showed soft tissue swelling, located mainly on the medial aspect with hypoechogenic heterogeneous areas filled with dense fluid. Subcutaneous tissue of the right extremity: width up to 18 mm, hyperechogenic, with fluid bands (width up to 3 mm). The left lower leg subcutaneous tissue was also slightly swollen.
Because of additional test results and the suggestion that she could have sarcoidosis (an ACE level test was not done) or cutaneous tuberculosis, the patient was transferred to the Department of Dermatology for further diagnostics.
At the time, diffuse flaky patches of dry skin after inflammation regression were present on the skin of the right lower extremity. Additionally, on the medial part of the left lower leg and on the right thigh and lower leg, painful, inflammatory, palpable 4-cm nodules with ulceration covered by fibrin developed (Figure 1).
Laboratory studies showed normochromic normocytic anaemia (RBC 3.41 × 106/μl, HGB 9.6 g/dl), thrombocythemia (605 × 103/μl), elevated D-dimer (3206 ng/ml), elevated potassium (5.6–5.8 mmol/l), slightly increased CRP level (7.29 mg/l), pANCA was positive, ASO was negative. Eosinophilia was not present.
Microbiological tests detected physiological flora: Staphylococcus epidermidis in the first culture. Whereas the second culture confirmed infection of Actinomyces spp. (broth culture on the basis of a microscopic specimen) – filamentous Gram-positive anaerobic to microaerophilic bacteria responsible for induction of actinomycosis.
Skin biopsy revealed Granulomatous vasculitis (PAS staining negative) (Figure 2).
Figure 2
A – Photograph showing yellow grains of Actinomyces spp. as a pathognomonic symptom. B, C – Photomicrographs of histopathology featuring granulomatous vasculitis in a cytological smear

However, on the basis of clinical presentation and investigations the patient did not fulfil the criteria of recognition of Granulomatous vasculitis in the setting of Granulomatosis with polyangiitis and Eosinophilic granulomatosis with polyangiitis.
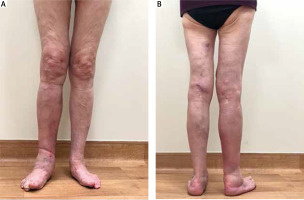
Because we considered tocilizumab-induced Granulomatous vasculitis, treatment with this biologic agent was discontinued. The patient’s vasculitis was treated with topical agents (boric acid, phenol and resorcinol, corticosteroids). Her actinomycosis was treated systemically with penicillin G 5M IU every 6 h for 9 days. It is proved that high doses of penicillin G are effective in the treatment of all forms of actinomycosis [7]. Subsequently she received oral phenoxymethylpenicillin 1500 every 8 h for the next 12 weeks. With the above regime the signs and symptoms resolved (Figure 3).
The differential diagnosis was complex because of the overlapping clinical presentation and the comorbidities. On the basis of clinical findings and skin biopsy we diagnosed not only very rare tocilizumab-induced vasculitis but also cutaneous actinomycosis which is also a rare (especially in the latitude of Poland) disorder which is not well described when primary invasion concerns skin and soft tissue [7]. The most frequent clinical form, which is estimated at around 50–60% of all described cases, is orocervicofacial actinomycosis [7, 8].
A rare complication of long-standing RA is a rheumatoid vasculitis (RV). RV most often affects vessels of skin and peripheral nerves. Cutaneous presentation of RV includes peripheral localized lesions with a predilection for the lower extremities – ulcers near the ankles, upper calf or dorsum of the foot are typically seen. Over the several past decades the prevalence of RV has decreased due to frequently used biologic agents [9, 10]. Biopsies are mostly recommended in RV diagnosis. Majority of them show leukocytoclastic vasculitis. Scott and Bacon proposed diagnostic criteria for systemic RV: 1) mononeuritis multiplex, 2) peripheral gangrene, 3) biopsy evidence of acute necrotising arteritis in addition to systemic illness (fever, weight loss), 4) deep cutaneous ulcers or active extra-articular disease (e.g. pleurisy, pericarditis) accompanied by vasculitis. Having one or more of the above suggests RV [9, 11].
Although cutaneous vasculitis might be seen in the course of RA, in our case vasculitis do not fulfil Scott and Bacon criteria, moreover localization and skin changes are not typical. Also the fact that skin changes developed 4 months after changing the treatment to tocilizumab, gave sufficient grounds to suspect a drug-induced vasculitis.
The etiopathogenic mechanism contributing to the development of vasculitis in patients treated with tocilizumab is not clearly understood. Potentially, tocilizumab as an antibody against IL-6 receptor could have resulted in immune complex formation and this may be the responsible mechanism for vasculitis [12].
On the basis of overall clinical presentation we diagnosed drug-induced, pANCA positive, Granulomatous vasculitis as well as actinomycosis.
Actinomyces are commensals of human oral cavity, gastrointestinal tract and urogenital tract and rarely are causative agents of the disease. They might become pathogenic when the mucosal injury appears and Actinomyces invade local organs. Hematogenic spread was also described [7].
Risk factors associated with the development of actinomycosis include male patients (except for actinomycosis of the pelvic which is usually seen in women after removing the intrauterine contraceptive device) aged 20–60 years as well as people with diabetes. Actinomycosis is also associated with immunosuppression caused by using steroids [8]. Because of RA the patient was chronically treated with steroids. When the actinomycosis developed she was on methylprednisolone 8 mg/day what could be a causative agent of actinomycosis development. Cutaneous actinomycosis was described in immunosuppressed patients with RA and psoriasis who were treated with anti-TNF-α inhibitors [13].
Actinomycosis is a chronic granulomatous condition [7] and there are isolated cases that also present with granulomatous vasculitis in the course of that infection [14]. Recently many investigators have focused on the relationship between infections and vasculitis. The two major pathogenic mechanisms of infection-related vasculitis include damage of the vessel wall caused by pathogen invasion and by immune-mediated mechanisms [15]. In general, the association between infection and vasculitis in most cases remains hypothetical. The casual link between infection and vasculitis has only been proven in few instances, including HBV in polyarteritis nodosa (PAN) and HCV in cryoglobulinemia [16]. In our case, vasculitis resolved as the infection caused by Actinomyces resolved. Although the vasculitis in our case might be caused by actinomycosis, available literature does not provide sufficient evidence to support that theory. Nevertheless, more research should be done to explain the possible link between the infection caused by Actinomyces and vasculitis.
This report gives additional information to the limited knowledge about tocilizumab-induced vasculitis and reminds about this paradoxical side effect of the recommended drug in the treatment of autoimmune diseases like RA. Additionally, it reminds a very rare manifestation of actinomycosis. Diagnosis of actinomycosis might be difficult and can be misdiagnosed because it frequently mimics different diseases such as malignancy or tuberculosis [7, 8]. Appropriate differential diagnosis and treatment ensure a full recovery.
Nevertheless, more research should be done to explain the link between the use of tocilizumab and the risk of vasculitis.