INTRODUCTION
Trichilemmal carcinoma is a very rare malignant tumor originating from the outer root sheath of the hair follicle. A distinctive histological feature of trichilemmal carcinoma, which differentiates it from other skin cancers, is the keratinization of the hair sheath, with the absence of a granular layer between the spinous and keratin layers in the tumor [1]. The main risk factors include exposure to sunlight [2, 3]. Other risk factors encompass radiation exposure, local injuries, burns, immunosuppression, and genetic conditions such as xeroderma pigmentosum and Cowden syndrome [4].
The average age of patients at diagnosis is 70 years, with a predominance of cases in males [4, 5]. The primary treatment for trichilemmal carcinoma is local wide excision with tumor-free margins. In cases of metastatic trichilemmal carcinoma, chemotherapy may be used and combinations of drugs such as cisplatin, cyclophosphamide, 5-fluorouracil, vinblastine, and bleomycin can help delay disease progression [6–8].
CASE REPORT
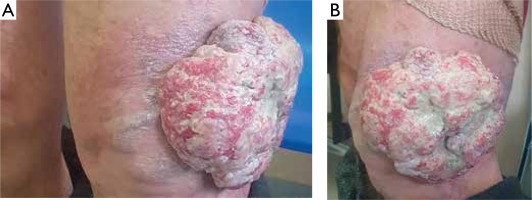
A 71-year-old patient was admitted to the Clinical Department of General Surgery for surgical treatment of a tumor located in the left thigh area, just above the knee. According to the patient, the lesion had been present since 2017 and had gradually increased in size, reaching a diameter of 12 cm (figs. 1 A, B). In the months prior to hospital admission, the patient reported increased bleeding from the tumor mass along with the development of a malodorous scent.
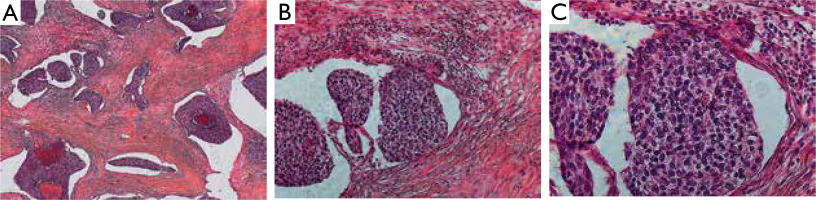
Additional tests revealed normocytic anemia at a level of 11.4 g/dl, with no other clinically significant deviations. The patient was qualified for the tumor resection. Tumor excision and skin reconstruction were performed, involving skin flap repositioning and Redon drainage of the subcutaneous tissue. Histopathological examination of the postoperative specimen, consisting of a 12 cm tumor and four skin fragments with a maximum dimension of 4 cm, confirmed trichilemmal carcinoma (figs. 2 A–C).
Figure 2
A–C Image of trichilemmal carcinoma. The extensive connective tissue structures with scattered inflammatory cells separate the nodules of atypical epithelioid cells (particularly visible in figure 2 B – 20× magnification). A – 5× magnification. C – 40× magnification
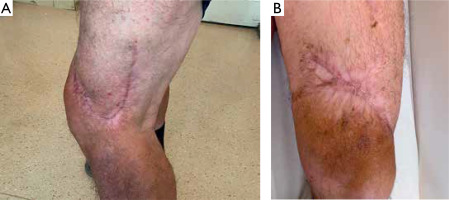
Clear margins without tumor infiltration were observed. Due to the fragmentation of the postoperative material, the patient remains under observation in the Surgical Outpatient Clinic. In a 4-month follow-up, enlarged lymph nodes were observed in the left inguinal region. The patient, however, declined further diagnostics and treatment. Figures 3 A and B depict the site following radical tumor resection.
DISCUSSION
Trichilemmal carcinoma (TLC), also known as trichilemmal hair sheath carcinoma, is a rare malignant tumor primarily originating from the outer root sheath of the hair follicle and developing within the follicular sheath [2, 3]. It typically appears on skin areas previously exposed to sunlight or in locations with prior trauma [4, 8]. This tumor often grows exophytically, as observed in the presented patient, and can resemble an ulcer. Histopathologically, larger lesions may show signs of necrosis and hemorrhagic changes [9]. Immunohistochemically, trichilemmal carcinoma shows positive reactivity to cytokeratins such as CK1, 10, 14, 17, and 19, while generally being negative for carcinoembryonic antigen (CEA), although occasional positive results have been reported [2]. The tumor is also negative for S-100 antigen and other cytokeratins, including CK7, 8, 15, 16, and 18 [10].
Although TLC can sometimes exhibit local malignancy, it generally has a benign course, especially when treated with radical excision [2, 11, 12]. Radical surgical resection is the primary treatment method for this type of tumor. A literature review showed that out of 35 cases treated surgically, only 2 patients experienced recurrence, with 1 patient having up to three recurrences. Patients were followed for periods ranging from 2 months to 10 years [4, 13], which confirms the high efficacy of radical excision in achieving lasting therapeutic outcomes. In our presented case, surgical resection was also performed, with clear margins free from tumor infiltration.
Lymph node metastasis and distant metastases are relatively rare and require systemic chemotherapy, typically involving four cycles of cisplatin and cyclophosphamide. However, there is currently no established standard protocol for treating trichilemmal carcinoma metastasis [14]. There are several different treatment options available in the literature. Recurrent or metastatic TLC can be treated with radiotherapy and/or chemotherapy, although treatment regimens are usually borrowed from other skin malignancies. In the case of TLC with metastases to lymph nodes, infiltration of bones, muscles and salivary glands, as reported in the study by Hayashi et al., CAV chemotherapy (cisplatin, adriamycin, vindesine) was performed according to the treatment regimen for very advanced cases of squamous cell carcinoma (SCC) [15]. In another case of recurrent TLC, after multiple surgical interventions, several cycles of chemotherapy with cisplatin, a-interferon and vinorelbine were administered [16]. Also, chemotherapy with cisplatin, bleomycin and vindesine was used in the case of a patient with involvement of regional lymph nodes and distant metastases [14].
Radiotherapy is the preferred method when the lesion is unresectable. In the case of metastatic disease, combined chemotherapy and radiotherapy are used. Lymph node dissection combined with local radiotherapy may provide a better prognosis in patients with lymph node metastases [17].
In the case of lymph node metastasis in trichilemmal carcinoma described by Lv et al., radical lymph node dissection was initially used, followed by 2 cycles of chemotherapy (docetaxel + cisplatin). Due to tumor invasion of muscles and additional lymph nodes, postoperative adjuvant radiotherapy and oral capecitabine chemotherapy were prescribed, considering that it might produce better outcomes for local-regional control [18]. In another case, the use of 5-fluoracil associated with cisplatin chemotherapy combined with subsequent adjuvant radiotherapy was also described [8].
In addition, completely different treatment options are being investigated. A case of TLC originating from parotid gland involvement with metastases to the lymph nodes of the neck has been described. The patient was treated with pembrolizumab, an immune checkpoint inhibitor targeting programmed cell death protein-1 [19].
In 1 reported case, a 90-year-old woman was successfully treated with imiquimod 5% cream. A case of TLC occurring on the scalp was described and treated with excision combined with photodynamic therapy, which has not been previously documented in the literature. The patient underwent intra- and postoperative therapy with the photosensitizer 5-aminolevulinic acid (ALA), which is a light-activated compound that produces reactive oxygen species, leading to the destruction of tumor cells and blood vessels while stimulating the immune system, then selectively eliminates tumor cells ensuring negative margins and minimizing the risk of recurrence [20].
This tumor is characterized by a slow progression (in this patient, the lesion had been present for 6 years), and local recurrences or distant metastases are rare after complete resection [21]. Nevertheless, strict patient follow-up is recommended to enable early detection of potential recurrences.
CONCLUSIONS
Trichilemmal carcinoma is an exceptionally rare tumor. Radical surgical resection remains the primary treatment method for trichilemmal carcinoma, providing high efficacy in preventing recurrence when adequate tumor-free margins are achieved. Although trichilemmal carcinoma is typically slow-growing and generally benign in nature, the risk of recurrence and rare metastases warrants long-term, close monitoring of patients. Regular follow-ups enable early detection of any potential changes, which is essential for preventing complications and improving long-term prognosis. Developing more precise treatment guidelines for trichilemmal carcinoma requires further research and data collection from additional cases. Reporting and analyzing new cases are crucial for a better understanding of the biology of this tumor and for optimizing therapeutic strategies, which, in the long term, may improve treatment outcomes for patients with trichilemmal carcinoma.