INTRODUCTION
The use of electronic photographic recording has greatly facilitated the process of image post-processing. With the growth of computing power of computers, more and more work relies on machine learning and artificial intelligence technologies, which increase the likelihood of obtaining excellent results without significant effort on the part of the user [1].
One of the areas of application of post-processing in medicine is special research in dermato-oncology. Digital images of the skin surface obtained during dermoscopy depend on the quality of the diagnostic and recording equipment, as well as the professional skills of the researcher. This dependence becomes more critical in the case of small lesions, the size of which does not exceed several millimetres.
Fixation with a digital camera allows for extensive work with the image, which can reveal valuable diagnostic features. In our opinion, the most important parameters of a photo are correct colour reproduction and clarity, which have the greatest impact on the recognition of structures in dermoscopy [2].
OBJECTIVE
To demonstrate the probable usefulness of digital photo post-processing in certain diagnostic situations.
CASE REPORT
Patient A, 29 years old. A spot on the skin of the back, up to 4 mm in diameter, irregular in shape, with hyperaemia of the surrounding tissues. The time of appearance and the presence of dynamic changes had not been established. The skin was in a state of severe photodamage.
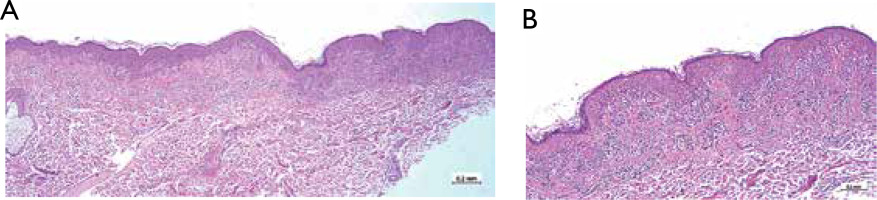
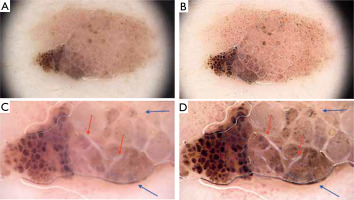
Dermoscopy was performed. The neoplasm contains branched and curved pigment lines. Focal areas of negative pigmentation (red arrows) and blood vessels (blue arrows) were found, but the image clarity was not sufficient for a confident assessment (fig. 1 A). After post-processing of the dermoscopic photos using machine learning algorithms, the vascular elements and negative pigmentation were significantly better visualised (fig. 1 B).
Figure 1
A – Patient A dermoscopy with Dermlite DL4 10 Pol; B – Patient A dermoscopy with Dermlite DL4 10× Pol Postprocessing ML Enhance and Sharpen. Areas of negative pigment meshwork (red arrows), blood vessels (blue arrows)
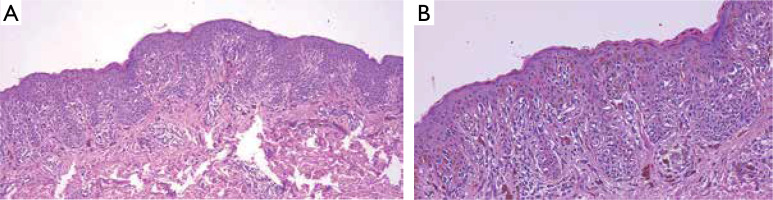
Histopathological examination revealed skin fragments exhibiting mild hyperkeratosis and acanthosis. Within the regions of acanthotic projections and along the dermoepidermal junction, focal areas of nested cellular proliferation were observed. These proliferating cells demonstrated pale, slightly granular cytoplasm and, in some areas, contained pigment. Additionally, dendritic cellular processes were noted. The nuclei of the proliferating cells were oval, pale basophilic, and exhibited prominent nucleoli. The histopathological diagnosis was consistent with a dysplastic nevus (figs. 2 A, B). A hint of such a diagnosis could be a negative pigment network, which was more noticeable after post-processing of the image. The histological basis for this dermoscopic criterion was probably the presence of local dermal fibroplasia.
Patient B, 14 years old. A single high-intensity spot, 2.3 × 2.7 mm in size, in the area of the right scapula; it appeared about 2 years ago and gradually increased in size.
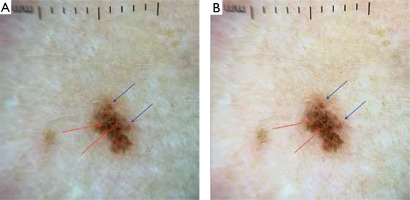
Dermoscopically, there was a heterogeneous lesion with a radiating pattern of the outer borders and high-intensity, low-structured areas in the middle part, where there were grey-blue inclusions and pigment granules. In the central part, there was a lumen where a hair follicle was present (figs. 3 A, C).
Figure 3
A – Patient B. Dermoscopy with FotoFinder Medicam 1000s Pol 60×. B – Patient B. Dermoscopy with FotoFinder Medicam 1000s Pol 60× postprocessing ML Enhance and Sharpen. C – Patient B. Dermoscopy with FotoFinder Medicam 1000s Pol 140×. D – Patient B. Dermoscopy with FotoFinder Medicam 1000s Pol 140× ML postprocessing Enhance and Sharpen. Linear-globular structures, probably hypertrophied skin vessels obscured by pigment located at the top of the dermal papillae (red arrows), surrounded by grey pigment located around the dermal papillae (blue arrows)
After the post-processing, the pigment network was visualised more clearly, with linear-globular structures (red arrows), probably hypertrophied skin vessels obscured by pigment located at the top of the dermal papillae, surrounded by grey pigment located around the dermal papillae (blue arrows). There were also areas of diffuse shallow pigmentation which may be caused by pigment incontinence (figs. 3 B, D).
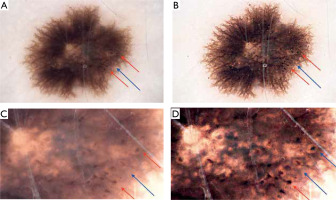
The lesion was excised with a suspicion of Spitz nevus or dysplastic nevus. The obtained material had epidermis with focal acanthosis; the basal layer was intensely pigmented. In the thickness of the acanthotic strands of the epidermis and at the level of the epidermal-dermal transition, there were foci of proliferation of melanocytes with an epithelioid histiotype, with uniform eosinophilic cytoplasm, mainly ovoid nuclei, groups of melanocytes with moderate polymorphism. Melanocytes were located in groups with the formation of nesting structures of different diameters over a larger area, between the areas of melanocyte accumulation there were foci of incontinence of deep brown pigment (fig. 4 A). The dermis surrounding the melanocytes had mild interstitial oedema, the vessels are hyperaemic, there were foci of mild lymphocyte infiltration and extensive foci of pigment incontinence (fig. 4 B). The conclusion was Spitz nevus. Thus, the elements of dermoscopy, which became clearer after post-processing, had their histological basis.
Patient C, 35 years old. A nodular lesion, 5.2 × 9.3 mm in size, on the left forearm, which, according to the patient, had existed since birth, but over the past year had changed colour and slightly increased in size.
Dermoscopically, at 20× magnification, a light brown papillomatous nodule was observed against the background of the spot. There were eccentrically located grouped pigment globules of different sizes, which turned into an area of diffuse pigmentation in the papillomatous part of the neoplasm. Vascular elements were represented mainly by curved vessels increasing their diameter closer to the pigmentation zone (fig. 5 A). At 60× magnification, white lines were visualised in the papillomatous part of the lesion, emphasising the cellular structure of the node (red arrows), and diffuse shallow pigment was seen in the middle of the cells (blue arrows) (fig. 5 C). After digital post-processing, the vascular pattern was more clearly distinguished and white lines were seen in 20× magnification (fig. 5 B). In addition to these structural features, pigment inclusions of various sizes and shapes were also more visible at 60× magnification (fig. 5 D).
Figure 5
A – Patient C. Dermoscopy with FotoFinder Medicam 1000s Pol 20×. B – Patient C. Dermoscopy with FotoFinder Medicam 1000s Pol 60× postprocessing ML Enhance and Sharpen. C – Patient C. Dermoscopy with FotoFinder Medicam 1000s Pol 60×. D – Patient C. Dermoscopy with FotoFinder Medicam 1000s Pol 60× after ML Enhance and Sharpen postprocessing. White lines emphasising the cellular structure of the node (red arrows), diffuse shallow pigment in the middle of the cells (blue arrows)
The neoplasm was removed because of the suspicion of tumour reactive changes or dysplasia. Subepidermal and dermal infiltrative vertical and horizontal growth was observed, extending into the deep reticular dermis to a depth of 2.4 mm. There was a proliferation of polymorphic melanocytes with an epithelioid histiotype, characterized by uneven eosinophilic cytoplasm, polymorphic nuclei with prominent nucleoli and coarse chromatin, and the presence of atypical mitoses. Tumour cells grew mainly in the form of nested structures, some of which merge with each other. Between the atypical melanocytes, there were foci of brown pigment deposition, haemorrhages, thin-walled vessels and foci of fibrous connective tissue growth (figs. 6 A–D). The conclusion was nevoid melanoma pT3aNxMx; Clark’s level 4; Breslow’s Stage III 2.4 mm.
Figure 6
A – Patient C. H&E 40× micrograph, B – Patient C. H&E 100× micrograph, C – Patient C. H&E 100× micrograph, D – Patient C. H&E 200× microphotograph
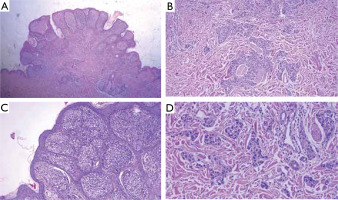
Therefore, despite a small number of alarming signs at 20× magnification, the use of 60× magnification and post-processing of the image allowed for improved visualisation of white lines, pigment structures and vascular elements, which became a key factor in choosing the right tactics for the patient’s management. The histological basis for the appearance of white lines was probably focal proliferation of connective tissue. Also, histological sections showed brown pigment deposits, which manifested as diffuse clods during dermoscopy.
DISCUSSION
In recent years, the digitalization of dermoscopy has enabled high and super high magnification, automated dynamic monitoring of moles, and open way to the use of artificial intelligence. These advancements have contributed to redistribution of roles and have relieved doctors from performing routine procedures. However, such systems require significant capital investment for acquisition and maintenance, unlike optical dermatoscopes and mobile phones, which are widely used to capture photographic images.
At the same time, the quality and informativeness of such examinations can vary significantly. It is not uncommon for professionals using phone cameras in clinical practice to encounter discrepancies between what is seen with the naked eye and the image captured through a dermatoscope. These differences may result from procedural shortcomings or the influence of built-in digital filters, which are often not optimized for medical photography.
In such cases, digital post-processing can be a valuable tool for restoring the native features of images. However, the quality and reliability of the results must be validated using sufficiently large research. It is also important to identify which dermoscopic structures can most effectively be detected after post-processing. The clinical cases presented in this article highlight the value of pigmentary features, vascular elements, and polarization-specific structures.
CONCLUSIONS
The use of digital photo post-processing can serve as a useful tool in certain diagnostic situations. The use of machine learning and artificial intelligence technologies simplifies the obtaining of results without significant effort on the part of the user. Establishing the reliability of the results obtained due to post-processing of images requires multicentre retrospective comparative studies.