Juvenile xanthogranuloma (JXG) is the most often occurring representative of a very rare group of disorders classified as non-Langerhans cell histiocytosis. It is most frequently diagnosed in children patients under the age of 1 year, but it can occur in every age group [1–4]. The character of the lesions is usually benign and of a very good prognosis, the changes often undergo spontaneous remission.
Xanthomas appear as a result of cholesterol and triglyceride accumulation in the tissues, most often in the skin, subcutaneous tissue and tendon sheaths. It is usually directly connected with hypercholesterolemia or hypertriglyceridemia [5–9].
Both abovementioned skin disorders, xanthoma and juvenile xanthogranuloma, are classified within a very wide group of cutaneous changes called xanthodermatoses. The most important characteristic of this group, easily distinguished during physical examination, is yellowish colour of the lesions that is a result of a substance accumulating in the skin (e.g. lipids) characterized by visible light reflection at wavelengths of 570–590 nm [10].
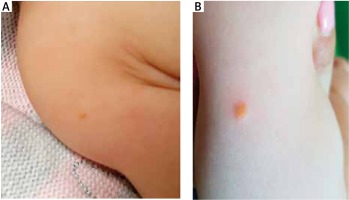
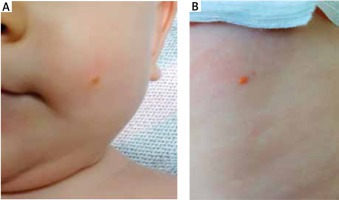
A 7-month-old girl sought medical attention in an outpatient dermatology clinic because of yellowish nodular changes located on her left cheek, on the brachial region – a lesion on the right arm, on the back and in the groin area. The lesions persisted for more than 3 months and the last change was noticed in the groin area 7 days before the medical appointment. During physical examination the occurrence of dome-shaped, well-demarcated, several millimetres in diameter, painless and non-itching nodules was observed. Besides, the girl was suffering from no other disorders, was taking no medications permanently and was under no medical specialist’s care. The child was caesarean-born in the first pregnancy and received 10 points in APGAR score. The mother was taking dydrogesterone during pregnancy because of a threatened miscarriage. A sample of the skin was obtained from the child’s lesion and on the basis of the outcome of histopathological examination, xanthogranuloma juvenile was diagnosed. The girl was also referred to an ophthalmological and paediatric clinic to undergo further diagnostic tests that excluded any extracutaneous lesions.
A 7-month-old boy was admitted to hospital to undergo diagnostic evaluation of six skin lesions located on the head, neck, back and posterior brachial region. During physical examination well-circumscribed, several millimetres in diameter, yellow-orange nodules were noticed. The biggest observed change was located on the head. The first lesions occurred on the neck and on the back at the age of 6 months followed by four additional changes on the back, head and posterior brachial region. The child was born naturally in the second pregnancy and in the second delivery, and received 10 points in APGAR score. During the gestation the mother was hospitalized because of nephrolithiasis and besides no other complications were noticed. In the family history contact dermatitis was observed in the child’s grandmother. On the basis of clinical manifestations of the disorder, a possible incidence of xanthomas was suggested. After admission to the hospital ward, the first skin biopsy was taken for histopathological examination, in which a microscopic image of the sample suggested occurrence of a linear epidermal nevus. After 3 months another skin biopsy was performed, but the outcome of the examination was non-diagnostic. In the histopathological examination of the third sample the prevalence of foamy cells in the dermis was noticed. Morphological appearance of the lesions was very characteristic of xanthomas. No abnormalities in the full lipid profile (low-density lipoprotein – LDL, high-density lipoprotein – HDL, triglycerides, total cholesterol) and other basic laboratory tests were found. The patient was then referred to a paediatric clinic for further diagnostic tests on possible lipid abnormalities. In the repeated laboratory tests no lipid metabolism disorders were confirmed (Figures 1, 2).
As mentioned above, juvenile xanthogranuloma is a very rare skin disorder belonging to a group of non-Langerhans cell histiocytosis. The most often occurring form of the disease is cutaneous juvenile xanthogranuloma, but it is also possible that changes develop on other tissues only or are accompanied by skin lesions that are usually located on the face, head or neck and normally take the form of a single, firm, well-demarcated nodule or papule [4, 11]. In the retrospective research conducted on the group of children suffering from juvenile xanthogranuloma it has been confirmed that among the cutaneous forms of the disease multifocal skin lesions were 9 times less often than cases with solitary occurrence of nodules or papules. The cases with multifocal skin lesions are also characterized by a considerably lower age at the moment of recognition. The average age of the patient at the moment of diagnosis was 5 months in case of multifocal skin lesions and 2 years in case of solitary changes. It was also proven that boys suffer from the multifocal form of the disease more often than girls (12 : 1), and in case of a solitary form of the disorder the prevalence is no longer so considerable (1.15 : 1) [12]. In the presented case of a 7-month-old girl, 4 lesions of the appearance typical of juvenile xanthogranuloma was observed.
Systemic forms of the disorder amount to 4% of all JXG cases and may lead to serious complications such as the central nervous system, liver, spleen and lungs involvement. Source literature provides case studies describing patients who died of juvenile xanthogranuloma complications, such as hepatic failure or changes in the central nervous system [11, 13, 14]. The most common location of extracutaneous lesions is the eye, in the area of which iris is most often involved [4, 15]. Unquestionable diagnosis of JXG can be only made basing on histopathological examination, but taking into consideration invasiveness of this method and usually young age of the patients, especially in case of lesions located on the face and characterized by typical appearance, biopsy can be avoided. In such cases recognition of the disease is made on the basis of the clinical picture and dermoscopic examination [11, 16, 17]. In the histopathological picture in the area of skin lesions, dense cellular infiltration is observed consisting mainly of histiocytes, giant cells including Touton cells, foamy cells and to a lesser extent, of eosinophils and lymphocytes [5, 18]. The composition of the infiltration evolves over the duration of the disease and in its late stage moderate fibroses can be also noticed [18]. Immunohistochemical staining, in which the expression of markers such as CD 68, CD 14,CD 163, Factor XIIIa, fascin, vimentin and no expression of proteins S100, CD1a, Langerin is found, may prove helpful in making differential diagnosis [5, 6, 11]. Sometimes the presence of protein S100 is also observed, but it is much more characteristic of Langerhans cell histiocytosis [6]. Juvenile xanthogranuloma should be distinguished not only from Langerhans cell histiocytosis, but also from various skin disorders of similar appearance such as i.a. nevus sebaceus, linear epidermal nevus or xanthoma [10]. Xanthomas are very often a manifestation of various disorders in the lipid profile, but can also accompany lymphoproliferative disorders or monoclonal gammopathy. In the histopathological picture the occurrence of lipid-laden cells called foamy cells is most characteristic of xanthomas. The pathomechanism of xanthomas formation is based on an increased local penetration of lipids through the vascular wall directly to connective tissue, where they are absorbed by macrophages and monocytes by means of phagocytosis and also thanks to specific receptors. Xanthomas occur most often in middle-aged or elderly patients and their manifestation in infants arouses suspicion of possible metabolic diseases, such as autosomal recessive hypercholesterolemia, homozygous familial hypercholesterolemia or sitosterolemia [19–21]. In the presented case of a 7-month-old boy, an incidence of histopathologically proven xanthomas with no abnormalities in laboratory tests was observed. The source literature contains case studies of xanthomas occurrence in patients with a normal lipid profile and suffering from no systemic disorders, but it is undoubtedly a very rare situation [19, 22–24].
In this article we have described two different cases of yellowish nodules appearing in infants which are rare in paediatric population and might coexist with various systemic complications. Despite many case reports of JXG available in the literature this disease entity is not thoroughly known even for dermatologists because of its infrequent occurrence in clinical practice. It is often difficult to differentiate between the two types of skin lesions only on the basis of clinical manifestations of the changes and in the early diagnosis both xanthoma and juvenile xanthogranuloma should be taken into consideration. Unquestionable diagnosis of the disorders is of utmost importance because both diseases may be connected with significant systemic complications.