Introduction
The proper function of the skin involves the protection from pathogens and physical damage. The skin consists of the superficial epidermis and the dermis which is located deeper. The continuous renewal of skin cells is attained in the process of cornification to maintain the protective function of the skin. The division of the basal layer of the epidermis is followed by cell migration to the surface, their maturation and death, and the formation of the stratum corneum which is the outermost epidermal layer [1]. The process of cornification is of special interest, because it combines the phenomenon of terminal differentiation and programmed cell death, and plays a particular role in non-oncological and oncological disorders [2]. Keratinocyte-derived non-melanoma skin cancers, i.e., basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) are the most common skin cancers [3, 4]. Skin cancers are a group of the most common neoplasms in humans. However, the actual incidence of epithelial skin cancer is difficult to estimate, as it is rarely included in cancer registries and, sometimes, both pathologies are registered together. The incidence of both cancers has been growing over the past decades [5, 6]. Basal cell cancer is the most common skin cancer with a low metastatic potential. Chronic sun exposure is the major risk factor for BCC development making the head and neck region the most common locations of BCC. Therefore, numerous patients who developed BCC are subsequently diagnosed with other malignant lesions. The incidence of BCC differs between countries and varies between 44.6/100 000 cases in Spain and 407/100 000 in the USA [7]. Men are more prone to develop BCC, but recently an increase in the number of cases in women has been noted in the younger population [8]. The risk of subsequent BCC is about 17-fold higher than in the general population, 3-fold higher for SCC and 2-fold higher for melanoma [9, 10]. SCC is the second skin cancer with the incidence being estimated at about 341/100 000 in men and 209/100 000 in women in Australia, and 497/100 000 in men and 296/100 000 in women in the USA [11]. The risk factors for SCC development include older age, male gender, cumulative UV exposure dose, low skin phototype, living in equatorial zones, chronic use of immunosuppressive drugs and some skin lesions.
Actinic keratosis (AK) is a precancerous lesion which predisposes to SCC development. The incidence of AK varies between geographical locations and the age of patients. The natural history of AK is divergent and involves remission (25%) [12, 13], stabilization, or progression to invasive skin cancer. The risk of progression from AK to SCC reaches 1–10% [2, 14]. However, it is largely unknown which lesions progress to SCC. It was suggested that some clinical features such as infiltration, inflammation, diameter over 1 cm, fast-growing lesion, bleeding, erythema, presence of ulceration within the lesions might be the markers of transformation [15].
Despite significant advances in molecular pathobiology and the era of personalized therapy in many cancers, the approved targeted therapy in skin cancer is still limited. Caspases constitute a large family of new molecular markers, which may be used in the diagnosis and treatment of cancer. They are enzymes that participate in the apoptosis, inflammation and terminal differentiations of cells [16–19]. However, the location and function of caspase 14 is different, because it does not participate in apoptosis. It is expressed only in mammals, mostly in the cornifying epithelia, Hassall’s bodies of the thymus and the forestomach of rodents [20]. According to the literature, caspase 14 plays an important role in processes leading to the formation of the epidermal barrier in the skin where it acts as an effector enzyme in processing profilaggrin and filaggrin. Consequently, it participates in the reorganization of cytoskeletal keratin filaments, which leads to the formation of the cornified envelope, and enables the production of substances called natural moisturizing factors (NMFs) that protect the skin from water loss [21, 22]. The role of caspase 14 in skin cancers has not been elucidated and the published data are limited [23]. The results of studies conducted on other cancer models are also inconclusive.
Aim
Therefore, we carried out a study to evaluate the potential role of caspase 14 in skin cancer and its precancerous lesions.
Material and methods
The study was approved by the Bioethics Committee of the University of Warmia and Mazury, Olsztyn. The study population comprised samples obtained from 56 patients who were admitted to the Department of Dermatology, Sexually Transmitted Diseases and Clinical Immunology in Olsztyn between January 2017 and March 2019. Informed consent for the procedure and the use of the biological material in research was obtained from all the participants. The samples were collected from patients with clinically suspected epithelial malignancies. Three samples were collected from each patient – one from the healthy skin on the dorsal surface of the hand (healthy samples) and two samples from the suspected skin lesions, one of which was subjected to pathomorphological examination. The diagnosis of malignancy was confirmed by an experienced pathomorphologist before further analysis. The control samples were collected from the healthy skin of the dorsal surface of the hand of patients without symptoms or a history of any epithelial malignancies. UV-exposed areas constituted the location from which samples were collected. Skin cancers are mostly located on sun-exposed areas and the goal was to obtain a comparable sample.
The biopsy procedure was conducted with the use of 2% lignocaine anaesthesia and a biopsy punch of 4 mm. The wounds were sutured afterwards. The samples were stored at –80°C for further analysis. The sample which was used for histopathological examination (routine H&E staining) was stored in buffered formalin.
The patients were divided into groups based on the outcome of the histological examination: SCC, BCC and AK. The SCC group consisted of 5 patients (2 men and 3 women, aged 69–87, mean: 77). We obtained reliable results from the lesional skin of all the patients and reliable results from the non-lesional skin of 3 of those patients. The BCC group consisted of 10 patients (6 men and 4 women aged between 48 and 84, mean: 73.8). We obtained reliable results from the lesional skin of all the patients and reliable results from the non-lesional skin of 7 of those patients. The AK group consisted of 20 patients (13 men and 7 women aged between 47 and 93, mean: 74.7). We obtained reliable results from both the lesional and non-lesional skin of 12 patients, and only lesional skin of 6 patients and only non-lesional skin of 2 patients. The control group consisted of 21 patients aged between 47 and 88. Their mean age was 70.5 years old. The group included 14 women and 7 men. The clinical diagnosis was consistent with the histopathological one in all the cases.
The loss of samples was due to damage during transportation and processing.
Skin samples were taken from the storage in tubes kept at –80°C and homogenized using a ceramic mortar in liquid nitrogen to the form of fine tissue powder. Subsequently, the samples were moved into a 1.5 ml Eppendorf tube with 400 µl of phenozol. They were stored for 30 min, vortexed for 1 min, and centrifuged. According to the manufacturer’s protocol, total mRNA was isolated from the samples with the Total RNA Mini Plus kit (A&A Biotechnology, Gdynia, Poland, #036-100). The quantification of RNA was performed using the Nanodrop system (Hampton) and its quality was assessed by the visualization of 28S and 18S rRNA bands after electrophoresis through 1.5% agarose gel and red staining (41,003; Biotium, Hayward, CA, USA). The same amount (1000 ng) of mRNA from each sample was reverse transcribed using the Maxima First Strand cDNA Synthesis Kit (Thermo Fisher, Waltham, MA, USA, #K1641). Reverse transcription was performed according to the manufacturer’s protocol. cDNA was frozen at –20°C until further analysis. All the reactions for target and reference genes were performed in duplicate on 384-well plates (MicroAmp™ Optical 384-Well Reaction Plate with Barcode, #4309849) and run in the ABI Prism 7900 sequence detection system (Applied Biosystems, Life Technologies, Foster City, CA, USA) with Maxima SYBR Green/ROX qPCR Master Mix (2X) (Thermo Scientific, Waltham, MA, USA, #K0222). Sample preparation was performed according to the manufacturer’s protocol with the use of 15 ng cDNA per well in a total of 10 µl of the reaction mix. The housekeeping gene was selected according to the literature. Relative mRNA data were quantified using the quantitative PCR miner algorithm. Briefly, the average of the cyclic threshold (Cq) and the primer efficiency level (E) for each sample were related using the following equation: [1/(1þE)Cq]. Afterwards, the expression levels of the target genes were normalized against the reference gene.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University of Warmia and Mazury (approved on 19.02.2017).
Results
The samples were collected from 56 patients including 21 control group subjects without skin lesions or a history of skin cancer. The number of samples was quite low and the numbers varied in different groups. Therefore, they could not have been analysed with parametric tests (the criterion of normal distribution of variables was not fulfilled). As a result, nonparametric tests were used.
The calculations were performed with Statistica PL v.13.1 using the modules: descriptive statistics and non-parametric statistics. The following tests for independent samples were used: the Median test, the Kruskal-Wallis test, the Kolmogorov-Smirnov test, and the U-Mann-Whitney test. The tests used for dependent samples were the sign test and the Wilcoxon pairwise order test, and Spearman’s rank correlation coefficient.
The mRNA expression of caspase 14/GAPDH in the healthy skin is presented in Table 1.
Table 1
mRNA expression of caspase 14 in the healthy skin
No correlation between the expression and the patients’ age or sex was observed in any of the groups.
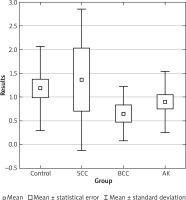
The expression level of caspase 14 was similar in the control group and actinic keratosis group. It was much higher than in squamous cell carcinoma healthy skin samples and basal cell carcinoma healthy skin samples (Figure 1).
As regards calculations for healthy skin samples in different groups, statistically significant differences were observed between the compared groups for the Median test with p = 0.043 and for the Kruskal-Wallis test with p = 0.023.
As the results were similar for the control group and actinic keratosis patients from non-lesional samples, they were analysed together and compared to SCC non-lesional samples together with BCC non-lesional samples.
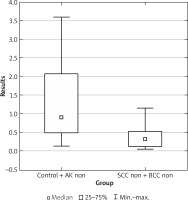
Clinically, group selection may be considered justified because the groups included patients with invasive skin cancer (BCC/SCC) and without invasive skin cancer (AK/healthy). The Kolmogorov-Smirnov test with p = 0.025 and the U-Mann-Whitney test with p = 0.003 showed statistically significant differences (Figure 2).
Figure 2
The mRNA expression of caspase 14 in the combined groups of healthy skin samples – the control group with actinic keratosis non-lesional samples, and non-lesional samples from BCC and SCC patients
As regards lesional skin samples, the expression of caspase 14/GAPDH is presented in Table 2.
Table 2
Expression of caspase 14 in the lesional samples
As presented in Figure 3, caspase 14 levels are comparable in the range of standard deviation in control group samples and in the lesional samples. No significant correlation was observed between the expression, sex and age in any group of lesional samples. In accordance with the accepted classification, the correlation of expression was high in SCC and SCC non-lesional samples, and BCC and BCC non-lesional samples.
A statistically significant correlation was noted between non-lesional and lesional samples in basal cell cancer (correlation coefficient of Pearson r = 0.82 with 7 samples, with the confidence level of a = 0.02).
As regards the actinic keratosis group, a statistically significant correlation was observed between non-lesional and lesional samples (correlation coefficient of Pearson r = 0.55 with 12 samples, and the confidence level of a = 0.05). Although a high correlation was observed, no statistically significant differences were noted for lesional and non-lesional groups.
Due to the fact that no significant differences occurred between SCC lesional and BCC lesional samples, and SCC non-lesional and BCC non-lesional samples (homogeneous groups), and the values of rank correlation coefficient were similar and of the same mark we decided to analyse them in combination. As regards the combined group of SCC and BCC (15 samples), mRNA caspase 14 expression levels ranged from 0.03 to 3.72, with the mean of 0.89, median of 0.72, standard deviation of 0.95, and statistical error of 0.25. As regards the combined group of SCC non and BCC (10 samples), mRNA caspase 14 expression levels ranged from 0.05 to 1.15, with the mean of 0.38, median of 0.31, standard deviation of 0.31, and statistical error of 0.10. The levels were lower in healthy skin samples and the difference was approx. 2 standard errors.
Statistically significant differences were observed between SCC/BCC vs. SCC non/BCC non groups with p = 0.027 for the sign test, and p = 0.022 for the Wilcoxon pairwise order test.
As regards combined groups, a statistically significant correlation was observed between the levels of mRNA expression of caspase 14 for lesional and non-lesional samples (correlation coefficient of Pearson r = 0.55 for 10 samples and confidence level of a = 0.01) – Figure 4. No statistically significant correlation was observed for gender or age in the combined groups.
Discussion
According to epidemiological data, BCC and SCC are the most common skin cancers with an observable increase in the incidence. The clinical course of BCC and SCC is different. Contrary to BCC, SCC grows faster and develops distant metastases more frequently, leading to patient death. The palliative systemic treatment options for patients with metastatic BCC or SCC are limited and are mainly based on classic chemotherapeutics. Currently, vismodegib, a Hedgehog pathway inhibitor, is registered for patients with metastatic, locally advanced BCC which is not suitable for surgery or radiotherapy. As regards SCC, some clinical trials are ongoing to evaluate the role of immunotherapy or anti-EGFR therapy. The development of molecular science led to significant discoveries. It provides better understanding of processes which control cancer growth and development. However, new discoveries are needed to improve diagnostic and therapeutic options for skin cancers. Caspases are a group including many proteins involved in the process of cancerogenesis. Despite the special role of caspase 14 in the skin as an external protector, there is paucity of clinical data in skin cancers, contrary to other solid tumours. A preclinical study by Hsu et al. showed that the transfection of caspase 14 expressing vector to epidermoid cancer cell line A431 reduced the growth and tumorigenicity of the cell line. The level of expression in other solid tumours may be decreased (cervical and colon cancer) or increased (lung adenocarcinoma) [23].
We performed the prospective pivotal study to evaluate the potential role of caspase 14 in skin cancer and its precancerous lesions. We enrolled 56 patients to the study.
mRNA caspase 14 was studied in lesional and non-lesional AK, BCC, SCC and control samples. The statistical analysis of collected data revealed clinically interesting results. Patients with the diagnosis of basal cell cancer and patients with squamous cell cancer were characterized by lower levels of the mRNA expression of caspase 14 in the healthy skin. Caspase 14 is known for its role in regulating the process of cornification, and protecting the skin from UV damage and water loss. The dysfunctions of caspase 14 activity may lead to the development of skin cancer. Potentially, the stimulation of caspase 14 might result in protecting patients from skin cancer. Exogenous stimulators of caspase 14, such as polyphenols, e.g., epigallocatechin-3-gallate EGCG, ceramides and delphinidin, were shown to upregulate caspase 14 levels and could be further researched for clinical application [24–27].
Furthermore, the data showed that the mRNA expression of caspase 14 was significantly lower in the healthy skin than in the lesional skin of patients with the diagnosis of squamous cell cancer or basal cell cancer.
In conclusion, the results suggest that patients with skin cancer are characterized by lower levels of the mRNA expression of caspase 14 in the healthy skin. However, when they develop skin cancer, this level is upregulated in skin lesions. The collected data did not allow the comparison of those values with the control group so it should be evaluated at subsequent study stages. It would be of crucial value to assess if those upregulated levels were higher or lower than in the healthy skin of the control group. Some issues still need to be analysed, e.g., whether upregulation is a way of trying to control the initiated malignant process by the compensative stimulation of protective molecules, or if cancer develops because the upregulation is insufficient. More data need to be collected to assess this issue and to be able to obtain statistically significant results.
The fact that patients with skin cancer are characterized by a lower mRNA expression of caspase 14 is easy to understand, knowing the potent role of the molecule in protecting cells from UV damage.
It is an element of cell physiology. The pathophysiological aspect and the role of caspase 14 in cells already affected by cancer is yet another issue.
Our study is the first one to describe the potential role of caspase 14 in human skin cancers. The results of our study show directions for future research. A relatively small study group which was not well-balanced constitutes a limitation of our study. It is to be continued to confirm the primary results and investigate the subject further. Moreover, the role of caspase in skin malignancies should be confirmed and compared at the protein level. Currently, we are assessing other molecules connected with cell death to compare them to caspase 14 (caspase 3, caspase 7, caspase 9, JAK-2, STAT-3). It could help us elucidate the role of caspase 14 in cancer-affected skin cells.