Introduction
Despite the shift towards minimally invasive procedures with lateral mini-thoracotomy and partial sternotomy, median midline full sternotomy is still the most employed technique in open heart surgery, providing excellent exposure [1]. However, sternal wound related complications and sternal dehiscence whether infectious or non-infectious are still concerns causing morbidity and/or mortality. Incidence can be as high as 3% and recurrent sternal opening and accompanying mediastinitis increase this rate up to 15% [2].
Robicsek weave, sternal cable systems, rigid plate fixation and thermoreactive nitinol clip implantation are currently employed methods for preventing aforementioned complications [1, 2]. Robicsek weave, which was defined in 1977, is still the most frequently used sternal wiring method in high-risk patients to avoid such problems and is proven to be safe and cost-effective, yet time-consuming [2, 3]. It is reluctantly performed by surgeons since it is the final step of surgery and may pose a challenge at this step.
Aim
In this study, we aimed to document the effectivity equivalence of a novel method with the currently most frequently employed method, of proven efficiency, namely Robicsek weave.
Material and methods
We have defined a novel method, “/” wiring (Durukan weave), for sternal wire closure which we thought would be as effective as Robicsek weave to prevent sternal wound related complications and or sternal dehiscence, yet would be less time consuming. We avoided extra material use, which would increase the cost.
We have been employing the technique since June 2021. We have retrospectively analyzed the patients who underwent on-pump surgical coronary revascularization with complete midline median sternotomy operated on between July 2018 and July 2021. Out of 756 patients eligible, Robicsek weave was performed in 312 patients. We compared those with “/” wiring operated on between July 2021 and November 2022. Redo cases and those with renal impairment were excluded. We performed propensity score matching to compare the two procedures. To obtain matched pairs with similar clinical and preoperative characteristics we calculated a propensity score using a logistic regression model that included clinical and perioperative characteristics. Patients were matched one-to-one on propensity scores with the “nearest neighbor matching” technique. We compared 50 patients with “/” wiring with 50 patients with Robicsek weave.
The study was conducted in Liv Ankara Hospital, Ankara, Turkey and approved by the institutional ethical committee, waiving informed consent based on its retrospective nature, and complies with the Declaration of Helsinki (Ethical Committee Approval Number: LAH 12/2022/006). Follow-up data were based on clinical follow-up visits of the patients during hospital stay and 1 month postoperatively. Chest X-ray was routinely performed 1 month postoperatively.
Robicsek weave is routinely employed by us when body mass index (BMI) > 25 kg/m2, in cases with diabetes mellitus, chronic obstructive pulmonary disease, bilateral LIMA use, presence of chronic obstructive pulmonary disease and in cases where the responsible surgeon defines the bone as osteoporotic upon surgical exposure. The rationale behind this strategy is the increased incidence of sternal dehiscence and infections in these patients [2]. Postoperative antibiotic prophylaxis was cephazolin 1 g qid iv for 2 days followed by oral amoxicillin/clavulanic acid 1 g bid for 1 week. We studied wound related complications, namely superficial and deep sternal wound infections, sternal dehiscence and mediastinitis.
Superficial wound infection was defined as infection limited to cutaneous and subcutaneous tissue which could be treated with simple surgical debridement and antibiotherapy based on culture results, whereas deep sternal wound infection was defined as infection involving sternal osteal tissue and mediastinum treated with radical debridement, antibiotherapy, negative pressure wound therapy (NPWT) and sternal repair [4]. Non-infectious sternal dehiscence was defined as non-infectious dehiscence or separation of the sternum treated with sternal repair [1].
“/” sternal wiring (Durukan technique) vs. Robicsek weave closure
In the defined method, the sternum is closed with standard 5 mm/45 cm surgical stainless steel sternal wires (Doğsan, Trabzon/Turkey) as in the “figure of 8”. However, the wires are knotted laterally with the corresponding previous one sequentially on the lateral side of the sternum rather than midline knotting as in the “figure of 8” (Figures 1 A–C, 2 A, B). The name comes from the surgical view of wires when the sternum is closed. The wires are in the form of “/” (Figure 3).
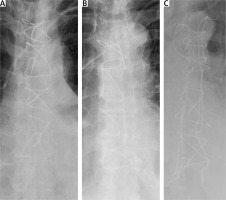
Figure 1
Schematic wiring order: A – sternal wires are applied in order from a to d, B – in “figure of 8” wiring “a”s are knotted with “d”s, C – in “/” wiring, each “a” is knotted with the next “a”, and each “d” is knotted with the next “d”
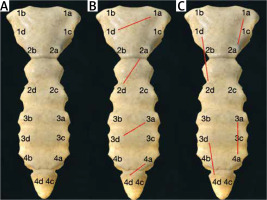
Robicsek weave is performed as defined originally by the author [3] (Figure 2 C).
The technique we defined here is actually a modification of the “figure of 8”. Therefore, we did not perform any animal study prior to human use, which may raise concern. Theoretical mathematical formulation and computer-based simulation confirmation was performed by a physics engineer. The technique was explained to each patient person to person by the surgeon and informed consent was obtained.
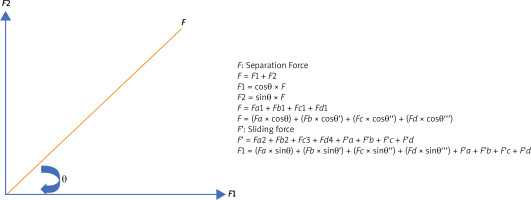
The mechanical forces applied on the sternum are shown in Figure 4 and the mathematical formulation is depicted in Figure 5. Force F is the vectoral sum of forces F1 and F2. F1 in the vertical direction spreads load on the lateral sternum and prevents sliding, therefore cutting of the sternum, whereas F2 prevents bone from separating.
Statistical analysis
Statistical analyses were performed using IBM SPSS software for Windows version 26.0 (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). Continuous variables were expressed as mean values ± standard deviation (SD). Categorical variables were expressed as numbers and percentages. Outcomes of the matched groups were compared using the Mann-Whitney U test for continuous variables and the c2 test and Fisher’s exact test for categorical variables. The conformity of continuous variables to normal distribution was evaluated with the Shapiro-Wilk test. A p-value under 0.05 was considered as statistically significant.
Results
There were 50 patients with Robicsek weave (mean age: 65.74 ±7.47 years) and 50 patients with “/” wiring (mean age: 66.12 ±7.23 years). There were 39 (78%) male and 11 (22%) female patients in the Robicsek weave group, whereas there were 36 (72%) male and 14 (28%) female patients in the “/” wiring group. There were 22 (44%) and 26 (52%) diabetic patients in Robicsek weave and “/” wiring groups, respectively. Bilateral IMA use was 5 (10%) in the Robicsek weave group and 6 (12%) in the “/” wiring group. Surgeon’s intraoperative evaluation revealed the sternum to be osteoporotic in 10 (20%) patients in the Robicsek weave group and 8 (16%) in the “/” wiring group. There were 10 (20%) and 8 (16%) COPD patients in the Robicsek weave group and the “/”wiring group respectively. Nineteen patients (38%) had a BMI > 25 kg/m2 in the Robicsek weave group and 21 (42%) in the Durukan weave group (Table I).
Table I
Perioperative characteristics of patients
| Parameter | Robicsek weave (n = 50) | Durukan weave (n = 50) | P-value* |
|---|---|---|---|
| Age, mean ± SD | 65.74 ±7.47 | 66.12 ±7.23 | 0.999* |
| CPB, mean ± SD | 50.5 ±9.27 | 50.8 ±9.69 | 0.874* |
| Intubation time [hours] mean ± SD | 9.66 ±6.86 | 9.88 ±3.33 | 0.838* |
| ICU stay [days] mean ± SD | 2 ±1.66 | 1.98 ±0.98 | 0.941* |
| HLOS [days] mean ± SD | 6 ±1.51 | 6.56 ±1.82 | 0.097* |
| Female gender, n (%) | 14 (28) | 11 (22) | 0.183** |
| Bilateral IMA, n (%) | 5 (10) | 6 (12) | 0.762** |
| Diabetes mellitus, n (%) | 22 (44) | 26 (52) | 0.432** |
| COPD, n (%) | 10 (20) | 8 (16) | 0.615** |
| Osteoporotic sternum, n (%) | 10 (20) | 11 (22) | 0.812** |
| BMI > 25 kg/m2, n (%) | 19 (38) | 21 (42) | 0.689** |
| Superficial wound infection, n (%) | – | 1 (2) | 0.999*** |
All patients underwent on-pump coronary bypass surgery with midline median sternotomy for standardization. The mean cardiopulmonary bypass time was 50.5 ±9.27 minutes in the Robicsek weave group and 50.8 ±9.69 minutes in the “/” wiring group. The median follow-up was 1 month, which we thought was adequate for documenting occurrence of sternal wound related problems and dehiscence.
The mean intubation time was 9.66 ±6.86 hours in Robicsek group whereas it was 9.88 ±3.33 hours in the Durukan technique group. Mean length of intensive care unit stay was 2 ±1.66 days and 1.98 ± 0.98 days respectively. Mean hospital length of stay was 6 ±1.51 days in the Robicsek weave group and 6.56 ±1.82 days in the Durukan technique group. None of the patients developed superficial sternal wound infections in the Robicsek weave group, whereas 2% (1) did so in the “/” wiring group. There were no deep sternal wound infections in either group. There was no non-infectious sternal dehiscence in either group (Table I).
Discussion
Despite advances in minimally invasive techniques, full midline sternotomy is still the most frequently preferred technique for exposure in open heart surgery [1–5]. Following median sternotomy, still, but with lowering rates, superficial and/or deep sternal wound infections and non-infectious sternal dehiscence are observed [5]. Each mentioned morbidity increases hospital length of stay, causes surgical re-exploration, further antibiotherapy and/or NWPT and mortality, and therefore costs [6, 7]. The Medicare and Medicaid Services defined surgical site infections particularly in surgical revascularization as a “never event” and did not allow reimbursement for this preventable complication by US federal health care programs [8]. Our national re-imbursement program also does not cover such postoperative morbidities in the first postoperative month.
Co-morbidities mentioned above increase the risk of sternal wound related complications, and therefore require intraoperative prophylaxis. It is well documented that sternal closure technique is as important as preoperative morbidities causing sternal wound related problems. Single and “figure of 8” patterns of sternal wiring are the most frequently employed techniques despite their lower effectiveness compared to Robicsek weave in high-risk patients [2]. The sternal wires may pull the sternum during cerclage and when the patient coughs or moves. The micro- and macro-trauma may cause sternal cutting by wires since the knotting of wires is performed in the midline. When single wiring and “figure of 8” wiring were compared, a lower rate of sternal instability was noted with “figure of 8” wiring (4% vs. 14.7 %, OR = 0.25) [9]. Robicsek weave is certainly effective since it provides a parasternal approach and shifts the force applied laterally [2, 3]. The main disadvantage of the technique is its time-consuming nature, and surgeons hesitate to perform it in the final step of surgery. Our rationale in defining “Durukan weave” was to shift the load on wires laterally while saving time, thus reducing hesitation. The lateral knotting strategy provides this lateral shift of load on wires while avoiding extra manipulation and extra wiring. The lateral shift of load also provides better and faster bone healing, avoiding further chronic loading trauma on the sternum. The results documented in the study may be evaluated as this novel technique is equivalent in effectivity to Robicsek weave, keeping in mind that further patients should be studied to prove it. Despite the low number of cases, propensity score matching increases statistical reliability. The cost for two wires is approximately $20. It may not cost much, but avoidance of two extra wires used in Robicsek weave may be advantageous, particularly in high volume centers. The cost for rigid sternal plates is $125 USD per plate and $12.5 per screw used, which makes $700 to $1400 per patient. For thermoreactive nitinol clips, the cost is around $550 per patient. Extra time consumed in Robicsek weave is the time for lateral wiring of two wires. The average time was not measured during the study, but the average for an experienced surgeon is maximum 5 minutes. However, for clips and plates, the time required for implantation depends on the surgeon and is much more.
The use of rigid sternal plates or cross-over plates extending from the ribs laterally is also proven to be effective. They are suggested for use in re-exploration since the procedure is more traumatic, necessitates radical subcutaneous dissection and has higher costs [10]. In a meta-analysis, they are proven to reduce sternal complications in high-risk patients, improve perioperative survival and decrease hospital length of stay. The technique provided 77% risk reduction. The main concern was increased health care costs [11].
Thermoreactive nitinol clips are also used to prevent sternal complications, but similar to sternal plates, they are mostly suggested in re-explorations. In cases of non-infectious sternal dehiscence, they have the advantage of avoiding dissection. They can be placed at different angles, even semi-vertically. However, the cost is increased, there is limited size availability and intercostal holing may cause hemorrhage [2]. Sarıkaya et al. compared clips with Robicsek weave by propensity score matching and documented effectivity equivalence, which may lead to the conclusion that the extra cost does not provide further advantages [12].
Limitations: The study has a small study population and is a single center study; therefore it is too early to generalize the results. The sequential knotting of wires may be disadvantageous. When one wire is broken, it will lead to failure of 2 wires. The surgeon must always place an even number of wires since sequential knotting is essential.
Conclusions
Sternal wound related problems will continue to be of concern while open heart surgery is still performed. Ease and applicability of sternal closure techniques as well as providing safer closure are the key points for avoidance. We believe that lateral shift of load on the sternum and on wires provided by the well-documented Robicsek weave is a consensus and “/” wiring may provide equivalent effectivity with the advantages of using 2 wires less, taking a shorter time and being less challenging.