Introduction
Immune checkpoint inhibitors (ICIs), such as anti-PD1 and anti-PD-L1 anti-bodies, are novel antineoplastic agents that have been widely used in the treatment of multiple malignancies. ICIs are fully humanized IgG monoclonal antibodies that target the human programmed death receptor-1 (PD1), leading to upregulated T-cell destruction of malignant cells. ICIs play an important role in the management of different types of cancer and are included in the guidelines for various malignancies. The increased use of these agents has significantly improved the prognosis of many cancers. However, their mechanism of action has also led to a rise in immune-related adverse events. For this reason, it is important for clinicians to keep in mind the possibility of rarer side effects presenting with common symptoms, such as gastrointestinal disorders.
Specifically, there is only a limited number of reported cases involving upper gastrointestinal tract disorders induced by ICIs. Immune-related gastritis is identified by widespread inflammation of the gastric mucosa, which appears erythematous and edematous. On histologic examination, the it shows signs of surface layer loss (epithelial denudation) along with a heavy presence of inflammatory cells [1].
There are only a few reported cases of immune-related gastritis in the literature, despite the widespread use of this immunotherapy over the past decade. Here, we present three cases from our hospital involving immune-mediated gastritis, along with a review of the literature on other published cases.
Case presentation
A 61-year-old female patient was diagnosed with stage IIIA lung adenocarcinoma. She underwent surgery – lobectomy – and received adjuvant chemotherapy. After completing chemotherapy, she was treated with pembrolizumab. She was admitted to the hospital due to gradually worsening gastric discomfort, pain, nausea, and vomiting. The symptoms had started two weeks prior to admission. Her clinical examination on admission revealed mild epigastric tenderness. An initial workup showed elevated levels of amylase in both blood and urine. An abdominal X-ray ruled out obstruction. A computed tomography (CT) scan of the chest and abdomen was performed soon after, revealing diffuse gastric wall edema and a halo sign (mucosal enhancement surrounded by submucosal and gastric wall edema). Upper endoscopy showed erythematous gastric mucosa and hemorrhagic gastritis involving the entire gastric mucosa. Histologically, findings of the gastric mucosa showed significant alterations consistent with chronic active gastritis and mucosal ulcerations. Within the inflammatory infiltrate, cell aggregates were observed without notable cytological atypia and strongly positive for the pancytokeratin marker. These findings suggested an autoimmune process. Methylprednisolone (1 mg/kg) was initiated, along with a proton pump inhibitor (PPI; esomeprazole 40 mg four times a day). Symptoms improved within a few days. The patient was discharged from the hospital and conti-nues oral methylprednisolone and PPI at lower doses.
In the second case, a 76-year-old male patient with metastatic gallbladder cancer was treated with cisplatin, gemcitabine, and durvalumab. He was admitted to the hospital due to persistent nausea and vomiting, especially after meals, following 6 cycles of immunotherapy. Gastro-scopy performed a few days later revealed erythematous gastric mucosa with sectional erosions. Histologic exami-nation revealed chronic inactive gastritis and inflammatory cell infiltration within the gastric tissue, predominantly composed of lymphocytes and plasma cells, accompanied by thickening of the muscularis mucosae. He was prescribed a PPI twice daily, with subsequent symptom improvement.
In the last case of this series, a 71-year-old female patient with metastatic microsatellite instability (MSI)-high endometrial carcinoma was treated with dostarlimab. After receiving 10 cycles of immunotherapy, she was hospitalized due to persistent epigastric pain lasting for weeks. During the clinical examination, no abnormal findings were detected. She underwent an upper endoscopy, which revealed duodenitis along with edematous and erythema-tous gastric mucosa. A histological examination showed epithelial denudation with severe lymphocytic inflammation. She started on PPI therapy, resulting in clinical improvement. Immunotherapy was discontinued.
Review of the literature
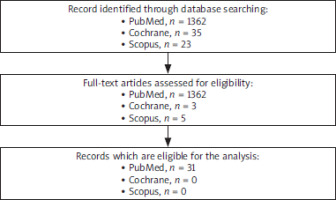
A review of the literature was performed, and three different databases (PubMed, Cochrane and Scopus) were searched to obtain a thorough understanding of the subject. A flowchart was created to describe the procedure of our search (Figure 1).
A total of 31 cases were found in which gastritis following immunotherapy was described. Although it is a side effect noted by the manufacturers, it is not as common as other side effects. For this reason, it is important to consider gastritis as a potential cause when a patient presents with gastrointestinal symptoms [6–36].
The most common immunotherapies were nivolumab and pembrolizumab, with 14 and 16 cases respectively. The most common clinical signs and symptoms are nausea, vomiting and gastric pain. Anorexia and bloating have also been described [6–36].
The main histological observations comprised chronic active gastritis, which featured an elevation in intraepi-thelial lymphocytes and apoptotic cells, along with a focal- enhancing injury pattern. This injury pattern was distinguished by localized areas of periglandular lymphohistiocytic inflammation and the presence of neutrophils infiltrating the glandular epithelium, all occurring without extensive chronic inflammatory alterations [6–36].
Finally, treatment for ICI gastritis typically depends on the severity of any accompanying ICI-related adverse events. In some cases, patients with only ICI gastritis can be managed with just a PPI and may continue their ICI therapy. However, the majority of patients need glucocorticoids to alleviate symptoms that do not respond to PPIs alone [6–36].
Discussion
Immunotherapy is an important treatment for various types of cancer. However, like other therapies, it is asso-ciated with side effects that every oncologist must be aware of. As immunotherapy continues to play a larger role in the management of oncology patients, irAEs will become more frequent. With this new reality, rarer side effects will also emerge. To our knowledge, only 31 cases of gastritis due to immunotherapy have been described. In addition, we have observed three cases in our department [2, 6–36].
In patients undergoing ICI therapy, a typical histological sign of mucosal damage is chronic active gastritis charac-terized by lymphoplasmacytic infiltration. This pattern is often associated with Helicobacter pylori infection. To rule out H. pylori as the cause in suspected cases of ICI gastritis, it is essential to perform a thorough evaluation of all biopsy samples. Although the histological features of both conditions may appear similar, H. pylori gastritis typically shows a neutrophilic or mixed infiltrate, while ICI therapy-associated gastritis predominantly exhibits a lymphocytic infiltrate [3–5].
Treatment for ICI gastritis typically depends on the severity of irAEs. The most common initial therapeutic approach is the use of PPIs, but in most cases, the use of glucocorticoids or PPIs may be necessary. Additionally, it is not always required to stop immunotherapy after diagnosing the side effect. Patients can continue their immunotherapy once their symptoms are managed [2, 6–36]. In our case series, only one of the patients required glucocorticoids, while the other two were managed with PPI therapy, leading to symptom relief. None of them has received ICIs again yet.
Conclusions
Gastritis associated with immune ICI therapy can occur in patients receiving these antineoplastic agents. Steroid treatment often alleviates symptoms and allows for the continuation of ICI therapy. Early identification of this complication is crucial, relying on clinical assessment, endoscopy, and histological analysis. Future research is needed to identify methods to prevent this therapy- related complication and explore more effective treatment options.