Introduction
Surgical treatment, regardless of the method used, always results in tissue damage and the subsequent metabolic response of the organism [1, 2]. There is no single and major parameter of measuring oxidative stress; thus many biomarkers can be used in different settings [3]. Numerous clinical trials have focused on the comparison of the organism’s clinical and metabolic reactions following classic vs. laparoscopic surgery [4–8]. The results of those studies have proven that minimally invasive surgery results in less severe damage and is generally less harmful to the patient. This, in turn, positively correlates with healing, a lower proportion of postoperative complications and faster return to normal physical activity. The next step in the development of minimally invasive techniques was single-port laparoscopy, where an optical trocar and surgical instruments are introduced via the same port-trocar called a multiport. This enables only one incision to be used instead of three. Among the advantages of single-port laparoscopy better cosmesis, lower pain levels, and a smaller number of complications are usually mentioned [9–11]. Based on the current European Hernia Society guidelines, the methods of choice for the treatment of inguinal hernia are the Lichtenstein and totally extra peritoneal (TEP) repairs [12]. Lately, single incision technique (TEP-SI) is growing in popularity in hernia operations [13, 14]. A number of studies comparing single-incision laparoscopic totally extra-peritoneal inguinal hernia repair with standard TEP procedure have been published in recent years [15–18]. However, they did not prove a significant advantage of TEP-SI over TEP. Instead, TEP-SI is considered a more difficult technique due to the loss of triangulation and external and internal conflict [19, 20]. In this paper we try to investigate whether TEP-SI has an advantage over the standard TEP procedure by analyzing the oxidative stress levels, which reflect the extent of the patient’s surgical trauma.
Aim
The aim of the study was to compare the oxidative stress response in patients treated operatively for inguinal hernia with TEP or TEP-SI technique. In order to do that, thiobarbituric acid reactive substances (TBARS) and total antioxidant status (TAS) were measured and compared before and after surgery.
Material and methods
The study was performed in accordance with the Declaration of Helsinki for Human Research 1975. The study protocol was approved by the appropriate bioethics committee. The participants of the study gave informed consent to the study procedure. A randomized group of 34 patients with one-sided inguinal hernia (M1 or L1 according to the EHS classification, with the width < 1.5 cm) were enrolled in the study. All the patients had a normal body mass index (BMI), did not suffer from chronic diseases, had not been using long-term medications and presented no signs of active infection during surgery. 17 patients were treated with a standard TEP method (group 1) and the other 17 patients were treated with the TEP-SI technique (group 2).
Surgical approach – TEP-SI
The procedure was performed under general anesthesia. First, the surgical site was disinfected. Next, a 25 mm-long transverse incision was made to the side of the hernia, above the umbilicus and then Langenbeck hooks were used to retract the wound edges. As a result, the anterior surface of the rectus sheath of the rectus abdominis muscle was revealed. The rectus abdominis medial edge was revealed following the incision of the anterior rectus sheath. Having moved the muscle aside, the index finger was placed beneath it and then moved down across the muscle’s posterior surface. This allowed the preperitoneal area to be dissected. The following steps involved introduction of a 10 mm-trocar in the area, administration of carbon dioxide and insertion of a surgical camera. The camera was then set in a swinging motion in order to dissect the preperitoneal area towards ASIS to the pubic symphysis. Next, two dissectors were introduced below the umbilicus. Packing suture was used for skin suturing so that pneumoperitoneum was maintained between the surgical instrument and the trocar in the preperitoneal area (Photo 1).
The dissectors were used to continue dissection in the preperitoneal area. First, it was dissected below the pubic symphysis in the midline and then to the side, when the lower edge of Douglas’ line was found. Next the hernia sac was dissected and then removed from the inguinal canal. With lateral inguinal hernia, spermatic cord elements were also dissected from the sac. The extent of dissection was the same in each type of hernia. The next stage involved inserting a 15 × 13 cm propylene mesh. Then the desufflation procedure was performed using the camera to observe how the peritoneum spread on the mesh. It was not necessary to suture the mesh. A single absorbable suture was used to close the incision of the anterior rectus sheath of the rectus abdominis muscle. Then the skin incision was closed with an intra-dermal suture.
Surgical approach – TEP
The procedure was performed under general anesthesia. After the disinfection of the surgical site, a 13 mm-long transverse incision was made to the side of the hernia, above the umbilicus. The operative technique was the same as in the TEP-SI approach up to the stage of pre-peritoneal area dissection. Instead of inserting two 5 mm tools next to the optical trocar, two additional incisions were made and the instruments were inserted. The first one was introduced through the 5 mm trocar (a 6 mm incision in the midline, around 3 cm below the incision for the optical trocar) and the second one was inserted through the second 6 mm incision, made close to the anterior superior iliac spine of the hernia side. The subsequent steps were the same as in the TEP-SI procedure.
Blood sampling and biochemical analysis
Ulnar venous blood samples were collected from all the participants three times (fasting, between 6:00 AM and 7:00 AM): before surgery (0), 1 day (1) and 4 days (2) after surgery. Baseline blood samples (0) were used for routine pre-operative laboratory assessment, including complete blood count, basic coagulation tests, C-reactive protein, glucose electrolyte levels and oxidative stress markers including TAS and TBARS measurements. Post-surgical blood samples (1 and 2) included assessment of TAS and TBARS only. Next, ratios expressing changes of these levels in time were calculated (1 : 0, 2 : 1; 2 : 0). The quotient of approximately 1.00 for any TAS ratio or any TBARS ratio means that there were no changes of total antioxidant status or lipid peroxidation products in plasma between the time points indicated. We also proposed an index which evaluates changes in TAS concentrations in relation to changes in TBARS levels, i.e. TAS (1 : 0)/TBARS (1 : 0). TAS were measured spectrophotometrically (RANDOX Laboratories, Crumlin, Antrim, UK) using Statfax 1904Plus (Awareness Technology, Palm City, FL) and TBARS were determined according to the Okhawa method [21] (Sigma reagents, Germany) using Specord M40 (Carl-Zeiss, Germany). The intra- and inter-assay coefficients of variation were as follows: TAS – 1.6% and 3.7%, TBARS – 1.9% and 3.8%.
Statistical analysis
Statistical analysis was performed using Statistica software version 10.0. The normality of value distribution was checked using the Shapiro-Wilk test. Next, nonparametric analyses were used to compare two study groups (Mann-Whitney U test) and to assess the changes of parameters during the time of observation (Friedmann ANOVA). A p < 0.05 was chosen to indicate a significant difference. Data are presented as median and interquartile range (in parentheses).
Results
There were no statistically significant differences in age, preoperative (0 blood sample) WBC and CRP levels, TAS and TBARS concentrations between the two groups of patients. Preoperative data of the two study groups are presented in Table I.
Table I
Characteristics of the study groups
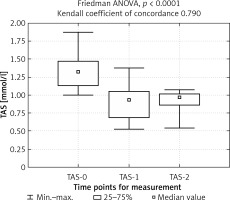
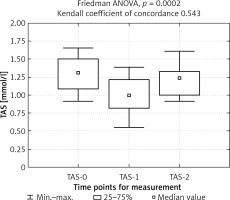
The duration of surgery was higher in group 2 (mean: 57.5 min) than in group 1 (mean: 50.0 min), p = 0.0286. The analysis of TAS concentrations at the three time points showed a decreased total antioxidant status on the first day after surgery (1 blood sample) in both groups. Sustained reduction on the fourth day after surgery (2 blood sample) was observed in group 1, whereas in group 2 an increase followed (Figures 1, 2).
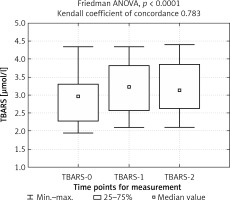
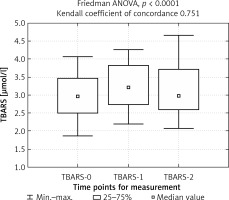
Moreover, a statistically significant difference was observed in TAS (2 : 0) ratio with a meaningful decrease in group 1. TBARS concentration was elevated 1 day after surgery in both groups, and remained at an elevated level in group 1, while in group 2 it decreased (Figures 3, 4).
TBARS (2 : 0) and TBARS (2 : 1) ratios were significantly elevated in group 1. Finally, higher TAS (2 : 1)/TBARS (2 : 1) and TAS (2 : 0)/TBARS (2 : 0) indexes were obtained in group 2. Detailed preoperative and postoperative data of oxidative stress markers of the two study groups are presented in Table II.
Table II
Results
Discussion
Laparoscopic surgery techniques were developed to improve treatment outcomes, reduce post-operative complications, accelerate healing and return to normal physical activity as well as minimize cosmetic defects in patients. Any form of trauma, including surgery, is known to result in oxidative stress development. In many clinical trials the severity of metabolic results of surgery-caused injury has been ascertained based on the assessment of oxidative stress/antioxidant status parameters, e.g. malondialdehyde (MDA), total antioxidant capacity, thiobarbituric acid substances, reduced glutathione, superoxide dismutase (SOD), catalase, glutathione peroxidase (GPx), oxidized LDL autoantibodies (oLAB), neopterin [3]. It is not clear which of these parameters is the best indicator of the oxidative stress response. Of the many indicators of oxidative stress we decided to use TBARS and TAS, which have been used in many trials aimed at assessing tissue trauma after surgery [22–26]. Results of studies comparing open and laparoscopic methods are greatly divergent, with some studies indicating less oxidative stress following laparoscopic surgery [27], others pointing to increased oxidative stress with laparoscopic surgery [8], and still others finding no differences in terms of oxidative stress between open and laparoscopic surgery [28]. Lack of a clear advantage of laparoscopic techniques compared to open techniques may be caused by increased intra-abdominal pressure during pneumoperitoneum and inflation-deflation, which may cause ischemia reperfusion and can subsequently lead to the elevation of oxidative stress level during laparoscopic surgery [29]. Further development of laparoscopic surgery technique focused on decreasing the number of incisions in single incision laparoscopic surgery, which is also used in hernia operations. Available scientific evidence does not demonstrate a clear clinical advantage of single incision laparoscopic surgery used in hernia repair over traditional laparoscopic surgery in terms of length of hospital stay, operative time, pain, recurrence, post-operative complications, issues related to ergonomics, surgical learning curve, and equipment needs [15–18, 30–32]. Our study tries to join in the discussion about advantages of TEP-SI over TEP by revealing the differences in oxidative stress levels between two types of surgery. It seems that if TEP-SI cannot be shown as less invasive than TEP, its only advantage would be slightly better cosmesis, since TEP-SI does not address more vexing problems related to hernia surgery, e.g. postoperative neuropathy, which causes chronic pain in patients who have undergone hernia surgery [33, 34]. So far, no other authors have compared metabolic responses between TEP and TEP-SI. Less invasive TEP-SI character may eventuate – although it has to be stressed that this is only a conjecture – from the fact that although the sum of lengths of all three incisions performed in TEP (13 mm + 6 mm + 6 mm) was equal to the length of one incision performed in TEP-SI (25 mm), in TEP-SI only one localized inflammatory response area is present instead of three inflammatory focuses in TEP. The small patient group and using only two oxidative stress factors are suggested to be the limitations of our study. However, this preliminary short-term observation may attract clinicians’ attention to the problem of perioperative metabolic stress and the significance of its reduction.