The incidence of thymoma during elective cardiac surgery ranges from 0.2% to 0.7% [1]. These tumours have a broad spectrum of clinical presentation, including local and paraneoplastic global symptoms [2]. In some cases, cardiac tamponade due to heart compression was the first presentation of the disease [3]. The treatment protocol includes surgical resection, additional adjuvant radiotherapy, and chemotherapy [4]. Unfortunately, the recurrence rate is around 15–30% even after complete resection [5].
We present a case of total surgical resection of a large thymoma, incidentally revealed during minimally invasive cardiac surgery.
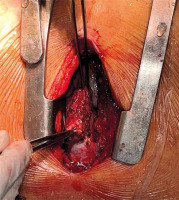
A 58-year-old female patient was admitted to the hospital for elective aortic valve surgery. The patient had experienced symptoms including chest pain on exertion, palpitations, and one episode of syncope in the previous 6 months. Except for a murmur over the aortic confluence, the rest of the physical examination, neurological status and standard laboratory analysis were unremarkable. The medical history revealed hypertension and diabetes mellitus. X-ray imaging showed a cardiovascular shadow typical for aortic valve disease and additional imaging techniques were not required. After the standard preoperative protocol for elective cardiac surgery, a surgical procedure was performed through the partial upper sternotomy. In the upper part of the anterior mediastinum, a large dark red calcified tumefaction suspicious for thymoma was detected (Figure 1). The tumourous tissue infiltrated the surrounding connective tissue, without infiltrating deeper structures of the mediastinum. The thymoma with dimensions of 60 × 40 × 24 mm was completely removed along with the surrounding healthy tissue (Figure 2). The resected tissue was sent for histological analysis. After that, the operation continued as a routine procedure according to our institutional protocol. The post-procedural period was uneventful, and the patient was discharged from the hospital 6 days after the procedure. A month after the operation, the first cardiological follow-up showed a satisfactory clinical state of the patient. The histopathological diagnosis of the patient that was confirmed by an immunohistochemical study showed WHO B2-type thymoma. It is an encapsulated tumour with a neoplastic epithelial component positive for CK AE1/AE3, p40, CK7, GLUT 3, thymocytes positive for CD5, CD99, Tdt, and Ki-67 proliferation index with 40% positivity in tumour cells. According to institutional recommendations, the patient was referred to the oncology council, where no additional radiotherapy or chemotherapy was indicated. The patient had no symptoms for the first 6 months after the operation, and there was no radiologically confirmed tumour recurrence.
Thymomas or thymic neoplasms are rare neoplasms with a frequency of less than 1% of all malignant tumours. Although neoplasms of this type are well known in thoracic surgery, they are a rare condition in cardiac surgery [3]. Due to slow growth, they can be unrecognized for an extended period, and usually patients are asymptomatic in the early stages of the disease [6]. Tumours can be accidentally detected through routine computed tomography (CT) and magnetic resonance imaging (MRI) before and during cardiac surgery [2]. We do not routinely use CT or MRI unless there is an indication. In some patients, the first manifestation of the disease was cardiac tamponade produced by heart compression [3]. However, our patient did not experience the latter, despite having a tumour larger than those previously described in the literature [1]. Patients with thymoma, in most cases, are split into three groups depending on their symptoms. The first group consists of patients with symptoms that develop because of mediastinal compression (dyspnoea, cough, or cardiac tamponade); the second group consists of patients with signs of myasthenia gravis as a paraneoplastic syndrome; and the third group consists of asymptomatic patients, as in our presentation [2, 3].
According to the new Masaoka-Koga classification, thymic neoplasms can be assigned to several groups depending on their macroscopic and microscopic features [7]. Our patient had B2-type thymoma, which means that it was in the early to medium phase of its development. Because of the absence of knowledge about its infiltration and stage of development, extensive resection into the healthy tissue is the best approach.
The literature describes several treatment modalities depending on the type and stage of the tumours: radiotherapy, chemotherapy, and surgical resection. Complete extirpation of the tumours is recommended as a definitive or staged therapy for all cases of thymoma [5].
If surgery is an option for the treatment of thymic neoplasm, the usual approach is medial sternotomy [6]. In our case, we performed partial upper sternotomy, as a routine step for minimally invasive aortic valve surgery, and we decided to perform a thymectomy through this surgical approach. In our case, the tumour did not spread more profoundly in the mediastinum toward vital organs, so we decided to carry out a total resection of the tumour mass, taking out part of the healthy tissue of the anterior mediastinum.
In conclusion, in cases of incidental discovery of a mediastinal tumour during cardiac surgery procedures, complete surgical resection is necessary to prevent potential tumour recurrence. The standard surgical approach for this particular medical condition is medial sternotomy. In cases where a tumourous mass is accidentally revealed but has not infiltrated deeper structures, partial upper sternotomy may be a suitable option if it provides good tumour exposure. However, if the tumour cannot be removed, conversion to full sternotomy is necessary to provide adequate surgical treatment.