Introduction
Pelvic organ prolapse (POP), a common and benign condition, is characterized by the descent of one or more aspects of the vagina and uterus. Women worldwide have a 50% chance of developing POP in their lifetime; 12–19% of women are at risk of requiring surgery for prolapse or incontinence [1, 2]. A number of mesh-based surgical techniques have been proved to be effective in the treatment of POP [3–5]. Laparoscopic lateral suspension with mesh (LLSM), a promising, minimally invasive procedure originally introduced by Dubuisson et al., was reported to effectively treat POP [6].
Aim
This study evaluated the clinical application of a modified version of this technique (mLLSM) for the management of apical and anterior POP.
Material and methods
Patients and study design
In this retrospective study, data from women suffering anterior and apical POP were obtained from the Department of Gynecology, Zhejiang Provincial People’s Hospital. All patients evaluated were diagnosed between January 2017 and December 2021.
Pelvic organ support was clinically assessed using the Pelvic Organ Prolapse Quantification Grading system (POP-Q). Inclusion criteria included symptomatic patients with a stage 2 or greater anterior and apical POP, and either lack of or presence of a mild rectocele (at point Aa, Ba, C, D > –1 cm beyond the hymen). Exclusion criteria were rectocele location at point Ap, Bp > +1 cm beyond the hymen, presence of a moderate severe rectocele, current treatment with corticosteroids, a history of genital cancer, contraindications to laparoscopy, or inability to comprehend questionnaires, return for evaluation or provide informed consent. Minimal follow-up for all patients was at 12 months postoperatively. Clinical, demographic and surgical data were obtained by review of medical records. Parameters including age at time of surgery, parity, prior delivery methods, body mass index, menopausal hormonal status, sexual activity, bladder functions, hysterectomy status, intestinal symptoms, and co-morbidities were noted. Perioperative data including surgical time, estimated blood loss, operative complications and postoperative follow-up data at 3 month and 12 months were also collected.
Anatomic outcomes were evaluated using the POP-Q to grade prolapse stage at all sites and defined as less than stage 1 (at least 1 cm above the hymen at all sites on Valsalva). Patient subjective satisfaction rate was considered a secondary outcome and assessed using the Pelvic Floor Impact Questionnaire 7 (PFIQ-7) and the Pelvic Floor Distress Inventory (PFDI-20). Significant improvements in POP symptoms, quality of life and postoperative sexual activity, as compared to baseline, were noted using the questionnaires at 12-month follow-up.
Our research protocol was approved by the Ethics Committee of the Zhejiang Provincial People’s Hospital (registration No: 2022QT019) and the study has been registered in the Chinese Clinical Trial Registry (registration No: ChiCTR2200062131).
Surgical technique
All patients underwent the mLLSM and all operations were performed by the same surgical team. Surgery was performed under general anesthesia with patients in the lithotomy position. A pneumoperitoneum was created, and four laparoscopic ports were placed: one 10-mm trocar was introduced into the umbilicus and two 10-mm trocars were introduced into the left and right suprapubic iliac areas (one each). A 5-mm trocar was introduced laterally at the left anterior-superior iliac crest.
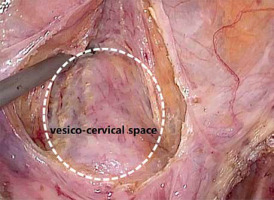
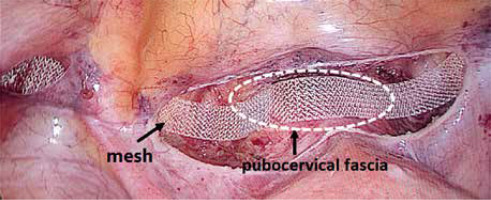
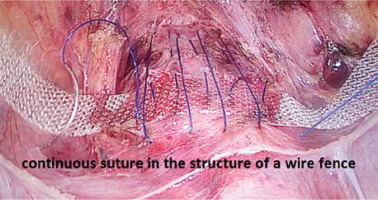
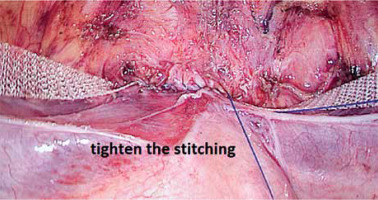
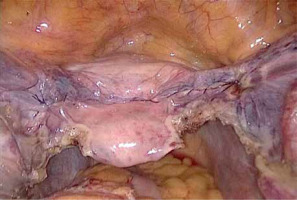
First, the vesicouterine pouch was opened to expose the vesico-cervical space well beyond any defects of the anterior vaginal wall (Photo 1). Next, a polypropylene mesh 1 cm wide and 45 cm long (Herniamesh SRL, Medical, Italy) was introduced via a 10-mm trocar into the peritoneal cavity to suspend the uterus. Laparoscopic forceps were pushed toward the round ligament at the level of its lateral peritoneal insertion into the anterior cervical plane. The mesh arm was subsequently grasped and retracted backward through the peritoneal tunnel. The central part of the mesh was flattened over the pubocervical fascia (Photo 2). In the third step, the middle of the mesh was sutured to the pubocervical fascia using a non-absorbable 2.0 polypropylene suture (Prolene, Ethicon, Johnson & Johnson Intl., Belgium). Meanwhile, the anterior vaginal and pubocervical fasciae were reconstructed using the same suture via a modified Darn repair technique. Fasciae were sutured continuously from top to bottom and left to right, in the structure of a wire fence (Photo 3). The anterior fascia and mesh were fixed together. When the suture was tightened, the anterior vaginal fascia was folded and lifted, thus covering the underlying mesh (Photo 4). The peritoneal incision was closed to cover the mesh and the peritoneal cavity completely sutured (Photo 5). After appropriately adjusting mesh tension, the mesh ends were fixed at the anterior abdominal fascia. When indicated, transvaginal posterior vaginal wall repair using native tissue was performed when the prolapse extended beyond the hymen or the patient suffered preoperative constipation.
Statistical analysis
Statistical analyses were performed using SPSS 22.0 (IBM, USA). Continuous variables were expressed as mean ± standard deviation (SD). Categorical data were reported as absolute numbers or percentages. Parametric data were not found to be normally distributed during preoperative and postoperative data comparisons when normality testing and homogeneity of variance; data were analyzed using the rank sum test in nonparametric tests. Rank sum test findings where significant data of all groups were statistically analyzed. A p-value of < 0.05 was considered significant.
Results
Demographics (Table I)
Out of 109 patients assessed for eligibility (Figure 1, CONSORT flow diagram), 109 underwent the (aforementioned mLLSM) procedure; data are presented in Table I. Patient median age was 63.40 ±10.10 years, mean body mass index was 23.31 ±2.12 kg/m2, mean parity was 2.36 ±0.96. In all, 103 (94.50%) patients had a history of vaginal delivery; of the 90 (82.57%) postmenopausal patients none were treated with hormone replacement regimens. A total of 47 (43.12%) patients suffered hypertension while 24 (21.02%) suffered diabetes. Dysuria, stress incontinence and constipation were noted among 86 (78.90%), 23 (21.10%) and 10 (9.2%) patients, respectively.
Table I
Demographics and characteristics of patients (n = 109)
Surgery record (Table II)
A total of 6 (5.50%) patients had undergone hysterectomy previously, 4 (3.67%) had undergone prior surgery for prolapse while none had a history of prior surgery for stress incontinence. While all patients underwent mLLSM, some additionally underwent concurrent surgical procedures (74.31% underwent transvaginal posterior vaginal wall repair; 80.73% underwent bilateral salpingo-oophorectomy; 13.76% underwent bilateral salpingectomy; 7.34% underwent hysterectomy; 5.50% underwent subtotal hysterectomy). Mean total operative time from uterovesical fold opening to complete mesh reperitonealization was 91.56 ±15.33 min. Mean estimated blood loss was 55.42 ±36.73 ml. No intraoperative complications including conversion to laparotomy, reoperation, blood transfusion, urinary injury, postoperative pelvic pain and mesh erosion were noted.
Table II
Surgery record (n = 109)
Anatomical outcomes (Table III)
Detailed assessments of anatomical and functional outcomes at preoperative, postoperative, 3 and 12-month timepoints were made. A total of 4 patients were lost to follow-up after 3 months. Anatomical success rates for prolapse were 96.33% and 94.50% when assessed using the POP-Q scale at 3- and 12-month follow-up. Apical and anterior POP-Q point measurements revealed significant improvements at 3 and 12 months postoperatively as compared with preoperative data. No significant differences in apical and anterior POP-Q point measurements were observed between 3- and 12-month postoperative time points. No significant improvement in the posterior compartment or differences in total vaginal length or genital hiatus were noted postoperatively as compared to preoperatively. Significant postoperative improvements were noted in perineal body measurement.
Table III
Anatomic outcomes and subjective success rate assessed at 3-month and 12-month follow-up by comparing the pre- and postoperative POP-Q parameters
Functional outcome data (Table IV)
Our results revealed lasting improvements in functional outcomes and quality of life. Functional outcomes were assessed using the PFIQ-7 and PFDI-20 questionnaires; data are shown in Table IV. Significantly lower PFIQ-7 and PFDI-20 scores were noted at 3- and 12-month follow-ups as compared to preoperatively in both groups. No significant differences between 3- and 12-month data were found. Recurrence of POP, however, was observed in 6 (5.50%) cases; 4 cases involved recurrence of anterior compartment prolapse (point Ba > 1 cm) after 3 months, which was treated with a pessary. Two cases manifested with asymptomatic clinical rectocele (point Bp > 0 cm) after 12 months, without further treatment.
Table IV
Comparison between pre- and post-operative questionnaire scores
Discussion
Here, we detailed mLLSM, a modified surgical technique useful for treating patients suffering anterior and apical POP. Our findings confirm that mLLSM is a safe and effective procedure with numerous advantages including shorter operating time, less blood loss and low rates of both intra- and postoperative complications. Importantly, mLLSM produced significant improvements in both anatomic and functional outcomes at minimal 12-month follow-up, as well as subjective symptoms.
Dubuisson et al. [6] first reported the LLSM technique for management of POP in 1998. Since then, numerous studies describing LLSM modifications have underscored the safety and efficacy of this approach in managing both anterior and apical POP [7–12]. Fixation of a pre-shaped mesh to the lateral vaginal wall and mesh arm suspension towards the lateral abdominal wall via a sub-peritoneal tunnel characterize this operation.
Here, we optimized the LLSM technique using a simple-shape (rather than tailored) mesh, reconstructing the anterior vaginal and pubocervical fasciae using non-absorbable sutures instead of mesh and fixing the mesh to the anterior fascia. Use of a simple-shape mesh eliminates the need for mesh cutting and reduces total mesh area. Although the unmodified LLS procedure carries a very low risk of perioperative complications, erosion of soft tissues by mesh products (e.g. bladder erosion) has been reported [13, 14].
The anterior fascia was thickened and strengthened using non-absorbable sutures, thus covering the entire anterior fascia in a fence-like manner and avoiding contact with the bladder. In addition, the anterior fascia was folded and lifted upon suture tightening, thereby covering the underlying mesh. Such suturing of the anterior and cervical fasciae enabled the anterior compartment to be drawn by the same suspension traction as the apical compartment. Of note, uterine preservation was reported superior to hysterectomy in the setting of LLS [11, 15, 16]. Similarly, uterine preservation is preferred in the setting of mLLSM unless hysterectomy is pathologically warranted. Noted advantages of uterine preservation were isthmic fixation of the mesh and reduction of bladder and vaginal erosion. In cases of warranting hysterectomy or in the setting of prior hysterectomy, the mesh was fixed to the apical vaginal compartment and covered via suturing; the anterior fascia was folded. These modifications did not increase the complexity of this procedure. Mean total operating time was 91.56 ±15.33 min and mean estimated blood loss was 55.42 ±36.73 ml.
Analyses of pre-and postoperative POP-Q data revealed significant improvement after a 12-month follow-up period. Apical and anterior compartment anatomical success rates were found to be 96.33% and 94.50%, respectively, similar to those reported in prior literature [17–20].
As a remarkably effective technique, mLLSM utilizes less mesh and achieves identical treatment goals. Here, we noted significant subjective outcome improvements when comparing pre- and post-operative PFIQ-7 and PFDI-20 scores. The quality of life of patients suffering POP as well as their associated symptoms of urinary incontinence, dysuria and urinary retention also markedly improved. Since few patients we evaluated were sexually active, sexual function questionnaires were not employed in this study. Our modified technique not only reduced mesh usage while safely accomplishing treatment objectives, but also eliminated bladder and vaginal erosion throughout a minimal 12-month follow-up period.
The LLS procedure offers the major advantage of significantly fewer postoperative complications [9, 21–23]. In agreement with prior reports, we noted no intraoperative complications in patients who underwent mLLSM. However, most procedures using mesh performed for POP management are later complicated by mesh erosion, especially in the case of transvaginal surgery [24, 25].
The small sample size evaluated and lack of control group are major limitations of the study. Importantly, our small sample size did not allow for ideal estimation of outcomes and complications. We are currently performing a prospective study that will further explore the advantages of utilizing mLLSM surgery for the treatment of apical and anterior POP.
Conclusions
The modified laparoscopic lateral suspension with mesh (mLLSM) is an effective and safe treatment for patients suffering apical and anterior POP. Here, we found that it offers such advantages as excellent outcomes and fewer mesh-related complications, underscoring the need for its consideration as an alternative treatment technique for the management of apical and anterior POP.