Introduction
Performing conventional tissue biopsy is a key step in cancer diagnosis, but it can be cumbersome and difficult to repeat, especially for monitoring cancer progression. Therefore, there is a growing need for a less invasive method to efficiently access information about tumour biology and progression.
Great progress has been made in the field of circulating tumour cells (CTCs), which are malignant cells released from solid tumours into the peripheral blood of cancer patients [1].Circulating tumour cells were first described in 1869 by Thomas Ashworth but have only gained interest as a potential biomarker in cancer management in the last decade [2, 3].
These cells are extremely rare or absent in the peripheral blood of healthy subjects and patients with non-malignant diseases [4]. In cancer patients, millions of tumour cells are released into the bloodstream during tumour progression, but only some of them will be able to induce metastasis in distant sites [5]. Circulating tumour cells must therefore be properly isolated, identified, and characterized. Many enrichment techniques have been developed for this purpose. These techniques can be classified into 2 categories: affinity-based methods that are designed to detect, at the level of CTCs, the expression of surface molecules such as epithelial cell adhesion molecule (EpCAM), and non-affinity-based methods that identify CTCs by their biophysical properties such as size or density [1, 6].
Cytology is used to diagnose or support the diagnosis of various pathologies based on the morphological appearance of isolated cells [7]. Compared to tissue biopsy, cytology is more convenient and economical; it requires minimal equipment and can be used to explore many sites when accessible [8]. Cytocentrifugation is one of many procedures for cytological analysis, but it only allows the processing of a certain volume of the cell suspension without the possibility of further investigation because the rest of the sample is not preserved; this could be a problem in the isolation of CTCs. Cytological cell blocks (cytoblocks) are therefore the alternative method to process, analyse, and especially store the entire cell suspension and liquid aspiration samples without any loss of biological material [9].
In our laboratory, we have focused on the preparation of cytoblocks from the peripheral blood buffy coat to detect CTCs that would be found among lymphocytes due to their close sedimentation coefficients.
The aim of this article was to detail our step-by-step development of a protocol that is the amalgamation of technical adjustments made to existing protocols for cytology specimen processing. We modified parameters from 3 different protocols [9–11], and the result was a manual protocol based on density gradient centrifugation of whole blood, cytoblock construction, formalin fixing and paraffin embedding (FFPE), and staining for in situ morphological study of the cellular material. We then applied our protocol for the isolation, processing, and characterization of CTCs.
Material and methods
Ethical considerations
Our project was approved by the Hospital Ethics Committee of the IBN ROCHD University Hospital (Casablanca, Morocco) and by the National Commission for the Protection of Personal Data (CNDP, Rabat - Morocco); authorizations numbered A-RS-261 and A-RS-262.
The protocol was developed on blood from healthy volunteer donors and then used and validated on blood samples from cancer patients.
All subjects explicitly consented to participate in the study. In total, we processed a dozen blood samples from healthy donors and 259 blood samples from lung and colorectal cancer patients.
Study design
We based our protocol refining on 3 published papers: La Fortune et al., Nam et al., and Balassanian et al., who respectively reported on the construction of gel blocks based on gelatin from the blood of cancer patients, the construction of HistoGel®-based cytoblocks with prefixation in 10% buffered formol from aspirate fluids, and finally the construction of HistoGel®-based cytoblocks with prefixation in 95% ethanol from aspirate fluids [9–11]. After density gradient centrifugation of Ficoll, we compared 2 solidifying agents (gelatin and HistoGel®), then 2 prefixation agents (formalin and ethanol), and finally the processing parameters (duration and temperature of bath immersing).
The selected experimental protocol is the result of technical adjustments of protocols using solidifying agents such as HistoGel® and gelatin. We describe below the procedure for the progressive development of this protocol. At each step, we modified one parameter at a time, and for each test, we simultaneously performed 2 or more manipulations on the same blood sample provided by a healthy donor. We then tested and validated our innovative protocol on blood samples from lung cancer and colorectal cancer patients from whom it was necessary to isolate, identify, and characterize CTCs.
Sample preparation
5–10 ml of venous blood samples were collected in EDTA tubes (MediPlus K3EDTA, China) from healthy donors or cancer patients. Blood samples were stored in crushed ice (0°C) or in the refrigerator (+4°C) for no more than 4 h before handling.
The collected blood was transferred to a 50-ml conical tube and diluted with phosphate-buffered saline (pH 7) (v : v). A volume of Ficoll (Lymphosep, Biowest serum specialist) equal to the initial volume of blood was placed in a new 50-ml conical tube. The diluted blood was gently placed on the Ficoll and centrifuged at 600 g for 20 min at 25°C (accel 5, decel 0) in a HERMLE Z 236 K centrifuge. Then, the first layer corresponding to the plasma was removed, and only the buffy coat likely to contain CTCs was collected and transferred into a new 50-ml conical tube. The buffy coat was rinsed in 3 times its volume of phosphate-buffered saline with a centrifugation at 330 g for 10 min at 25°C (accel 9, decel 4). At the end of the centrifugation, the supernatant was removed, and the pellet was technically processed to make a cytoblock.
Choice of solidifying agent
According to Nam et al., a gel block is generated by mixing the pre-obtained pellet with an equal volume of gelatin and allowing it to solidify at 4°C [10]. This gel block was fixed in buffered formalin overnight. The gel block was then put in crayon paper and placed in a cassette.
We tested HistoGel® as a replacement of gelatin for the resuspension of the pellet, which is a product composed of hydroxyethyl agarose, which proved to have 2 major advantages: faster solidification, and the use of a smaller volume and the suppression of crayon paper.
Pre-fixation
However, the use of HistoGel® is conditioned by a preliminary step of sample fixation, called pre-fixation. This pre-fixation is carried out, according to the manufacture’s data sheet accompanying HistoGel®, with ethanol at 95°C. To optimize this pre-fixation, we tried replacing the 95° ethanol with 10% formalin, commonly used for histological samples; this formalin pre-fixation was used by Balassanian et al., 2016 in the context of a cytoblock preparation with HistoGel® [11].
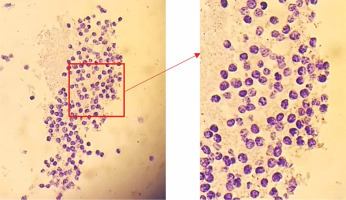
We tested both prefixation agents. It was found that ethanol-treated specimens were morphologically better preserved (Fig. 1 A) than with formalin, which induces over-fixation. However, prefixation with ethanol was not sufficient.
Fig. 1
Slide containing peripheral blood mononuclear cells (PBMC) from a healthy donor, prefixed in 95% ethanol, conserved in HistoGel®, and stained with haematoxylin and eosin (400×) (A), slide containing PBMC from a healthy donor, prefixed in 10% formalin, conserved in HistoGel®, and stained with haematoxylin and eosin (400×) (B)
An additional fixation step after suspension in HistoGel® would therefore be necessary for better preservation of the nuclei.
Optimal volume of HistoGel®
According to Rekhtman et al., the optimal added volumes of HistoGel® are 250 µl for pellets of 1–2 ml and 500 µl for pellets of volumes greater than 3 ml [12].
Although the pellets obtained in our manipulation were not larger than 3 ml, we found the 500 µl volume to be more convenient for our cytoblock construction and in terms of handling.
Cytoblock construction protocol
The suspension (Histogel® + pellet) was then placed in a square metal mould (15 × 15 × 6 mm) and left to cool and thus solidify on a cold accumulator. The HistoGel® block thus obtained was placed in a cassette.
Additional fixation
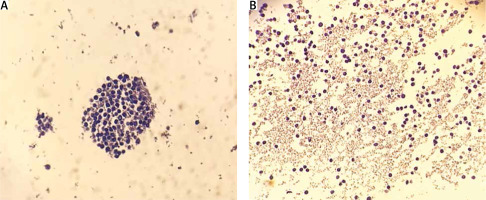
The cassette containing the HistoGel® block was then placed in 10% formalin for the additional fixation step for a duration that varies between 16 and 20 h. However, to avoid the risk of possible over-fixation, we decided to test the temperature parameter by keeping the same duration, i.e. to proceed with the additional fixation at room temperature and at +4°C (Fig. 2). This second fixation, performed at room temperature, over a period of 16–20 h, gave poorly preserved cells with damaged cytoplasm and retracted nuclei (Fig. 2 B) resulting from too much fixation. The fixation at 4°C, still over a period of 16–20 h, proved to be the best in terms of preservation of cell morphology thanks to a careful fixation process, which was much slower and without over-fixation. We therefore chose the formula of a cytoblock fixation in 10% formalin at +4°C and over a period of 16–20 h (Fig. 2 A).
Fig. 2
Slide containing peripheral blood mononuclear cells (PBMC) from a healthy donor, prefixed in 95% ethanol, conserved in HistoGel®, then fixed in 10% formalin at +4°C for 16 hours and stained with haematoxylin and eosin (400×) (A), slide containing PBMC from a healthy donor, prefixed in 95% ethanol, stored in HistoGel®, then fixed in 10% formalin for 16 hours at room temperature and stained with haematoxylin and eosin (400×) (B)
Processing program
After fixation, the cassette containing the gel block was passed through a circulating machine (STP 120 Thermo Scientific) for paraffin impregnation. We tried to use the same program that Nam et al. used but with some changes to fit our machine [10].
Their program was 13 h under vacuum impregnation at 20 lbs; the vacuum allowed faster penetration of the fluids. Our machine was not equipped with a vacuum device, so we made changes in terms of increasing the bath times. The final program was as follows: 80% ethanol (AnalaR NORMAPUR VWR) with one change (1.15 h each), 96% ethanol (1 h), 100% ethanol with 2 changes (2 h each), ethanol/toluene 1 : 1 (1 h); toluene with 3 changes (1 h each), and paraffin wax at 60°C (2 h), due to the absence of vacuum in our apparatus.
Inclusion
For this, we proceeded with the inclusion of the cytoblock in paraffin/Paraplast with a volume of 50/50. After this step we could keep our blocks as long as we wanted, until we used them for cytochemical and immunocytochemical techniques.
Microtomy and preparation for staining
The final FFPE cytoblocks can be microtomized, stained, or immunostained. Microtomy on cytoblocks is easier due to a lower cell density than in tissues. The section was performed at 2–3 µm. The sections were spread out on glass slides.
They were dewaxed in toluene and then rehydrated in ethanol at decreasing concentrations and finally in a distilled water bath.
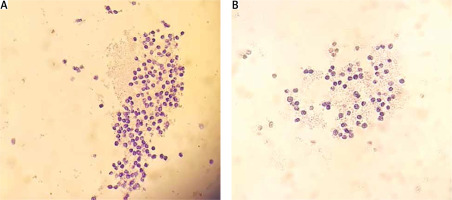
Haematoxylin and eosin staining
The slides were immersed successively in haematoxylin for 10 minutes and then in eosin for 5 minutes, with a rinsing step with tap water in between. They were then prepared for mounting by dehydration in ethanol at increasing concentrations, followed by clearing in toluene. The mounting was performed using a mounting resin. Figure 3 below shows the slide resulting from the above steps.
Immunocytochemistry
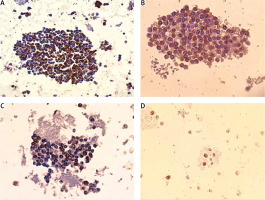
We also performed an immunocytochemistry (ICC) tech-nique using antibodies respectively directed against the common leukocyte antigen CD45 to distinguish lymphocytes and epithelial markers such as cytokeratin (CK) and EpCAM to reveal CTCs. Sections were placed on SuperFrost ® Plus slides (Thermo Scientific). After rehydration as explained above, the slides containing the sections were pretreated by heat-induced antigen restoration (100°C) in EDTA buffer (pH 8) for CD45 for 30 minutes and in citrate buffer (pH 6) for CK and EpCAM for 20 minutes. Preparation of the stain was by blocking endogenous peroxidases as well as non-specific binding. Primary antibodies (anti-CD45, clone: 2B11+PD7/26, 1 : 100 dilution, anti-CK clone AE1/AE3, 1 : 100 dilution, and anti-EpCAM clone Ber-Ep4, 1 : 150 dilution) were then applied OVN at 4°C for optimal results. The Dako EnVision™ FLEX detection system (horseradish peroxidase-coupled polymer followed by DAB [3,3’-Diaminobenzidine]) was used to reveal antigen-antibody binding. Mayer’s hemalun was applied to counterstain the nuclei. Finally, the slides were prepared for analysis by dehydration in ethanol at increasing concentrations, clearing in toluene, and mounting with resin mounting medium. Figure 4 below shows a slide resulting from the above steps.
Fig. 4
Expression of CD45 in a cell block leucocyte preparation (400×) (A), expression of cytokeratin (CK) in circulating tumour cells (CTCs) in blood from a lung cancer patient (400×) (B), expression of CK in CTCs in blood from a colorectal cancer (CRC) patient (400×) (C), expression of surface molecules such as epithelial cell adhesion molecules in CTCs in blood from a CRC patient (400×) (D)
Results
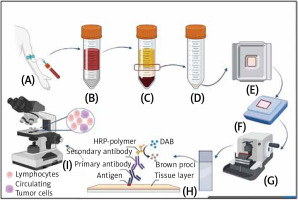
We succeeded in modifying a protocol for the construction of cytoblocks and applied it to study CTCs in lung and colorectal cancers, respectively (Fig. 5). We relayed the results regarding the cytoblock construction yield.
The protocol was followed to make a total of 259 cytoblocks from the blood samples of cancer patients. During the dehydration process, 22/259 cytoblocks were shrunken and were therefore excluded, for an estimated preparation success rate of 91.52%. The shrinking would occur every 10 processing cycles, so we countered it by changing the alcohol baths twice as frequently as usual.
Fig. 5
Schema summarizing the final protocol steps. 5–10 ml venous blood is collected in an EDTA tube (A), diluted blood with phosphate-buffered saline (pH 7) is gently placed on Ficoll (B). After centrifuging, only the buffy coat likely to contain circulating tumour cells (CTCs) is collected (C), and rinsed in 3 times its volume of phosphate-buffered saline with centrifugation. Only the pellet is kept afterwards, prefixed in ethanol 95° (D), resuspended in Histo- Gel®, and then placed in a square metal mould and left to cool (E). The HistoGel® block is then placed in a histological cassette and fixed in 10% formalin for 16–20 h at 4°C, then processed in a 13.5-hour circulating program and embedded in paraffin/Paraplast(50/50) (F). Microtomy is performed at 2–3 μm (G), and an immunocytochemistry technique is performed using antibodies respectively directed against the common leukocyte antigen CD45 and epithelial markers such as cytokeratin and expression of surface molecules such as epithelial cell adhesion molecule to reveal CTCs I). Interpretation of the slides under the microscope (H) The figure was created using BioRender.com (accessed: 18.04.2023).
After exclusion, 237 cytoblocks were immunostained as shown in Figure 4. Morphological and immunocytochemical evaluation was carried out by an anatomo-cytopathologist, according to whom the cellular material was well preserved, allowing the distinction between lymphocytes and non-blood cells, and the immunostaining was easily assessed in terms of specificity (membrane or nuclear staining) intensity and percentage of expression.
Discussion
In this article, we have detailed a protocol – as well as the adjustments that led to its establishment – for the construction of cytoblocks for the detection and characterization of CTCs. This protocol is based on a pre-fixation step with 95% ethanol, a block construction step with HistoGel®, and finally an overnight fixation step in 10% formalin at a temperature of 4°C to avoid the problem of over-fixation. This parameter, which is a key step in the success of our protocol, is reported for the first time in the literature in the field of cytology by our study.
Cytoblocks could be prepared from a variety of cellular suspensions and fine needle aspirations. The applications for this sample preparation method ranges from morphological and phenotyping (haematoxylin and eosin staining and ICC) to molecular testing (fluorescence in situ hybridization, polymerase chain reaction, and next-generation Sequencing) [11].
We applied this protocol to the detection and characterization of CTCs in lung and colorectal cancers, which allowed us to preserve long-term samples previously prepared as cytoblocks. It also allowed us to study CTCs at the morphological level in addition to the immunocytochemical phenotyping performed by targeting both epithelial and mesenchymal markers, unlike other techniques based only on epithelial markers such as EpCAM. Moreover, the cytoblock could also potentially be processed at the molecular level because it would allow the extraction of tumour DNA from CTCs.
Conclusions
The protocol described herein allows the detection and characterization of CTCs. The cytoblock, which represents a quasi-manual approach, which is relatively simple to reproduce and less costly, enables the preservation of CTCs as well as the performance of other investigations. The latter could be achieved by targeting antigens to phenotype CTCs regardless of their heterogeneity in comparison with the primary tumour. It is even possible to extract the DNA from these CTCs and thus study their molecular profile by identifying the mutations likely to generate resistance to treatment. Circulating tumour cell detection and characterization could become a steppingstone towards a better understanding of the metastatic stage in tumour progression. This protocol may also be of interest in other fields of research, notably in haematology for haematological malignancies and in immunology.