The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic has caused a unique burden on healthcare facilities and a substantial organisational challenge. Due to the extremely high contagiousness of the disease, governments and healthcare authorities face the problem of limiting spread of the infection in the society, especially in healthcare workers. The problem has particularly impacted perioperative medicine, especially anaesthesiology due to the potential risk for patients and threat of staff contamination during aerosol generating procedures [1–4]. Children represent 1–5% of total coronavirus disease 2019 (COVID-19) cases [1, 5]. Manifestation of the disease in children is gene-rally mild or asymptomatic [6–9]. The rate of asym-ptomatic children in the population is assessed as 5–16%, but the data may be underestimated as there is no cross-sectional testing in the population [9]. In addition, most observations regarding infected children are based on small groups of patients. Meanwhile, there are interesting data from analysis of children admitted to the hospital for the purpose of general anaesthesia [10]. Safety of general anaesthesia in children infected with SARS-CoV-2 is also a matter of concern [11–14]. Single reports concerning anaesthetic complications in small groups of SARS-CoV-2 infected children suggest that although the rate of asymptomatic cases is quite high (63–92%) even the asymptomatic patients are still at higher risk of anaesthetic respiratory complications [15, 16]. As some of these observations differ from what we see in everyday practice, we performed a retrospective, case control study analysing the clinical course of SARS-CoV-2 infection and risk of general anaesthesia in children admitted to a tertiary paediatric university hospital in Poland for the purpose of an urgent procedure requiring general anaesthesia between April 1st and September 30th, 2021. The procedure was assessed as urgent when it had to be performed within 6 hours from admission. The control group consisted of SARS-CoV-2 negative children consecutively admitted to the hospital for the same reason during the first month of observation. Our hypothesis was: a child with SARS-CoV-2 infection can be safely anaesthetised.
METHODS
The local Bioethical Committee was informed, but as the analysis was conducted retrospectively, its consent was waived.
Data were extracted from medical records: age, gender, American Society of Anesthesiologists (ASA) physical status classification, SARS-CoV-2 test result, type of procedure performed, type of anaesthesia (intravenous, inhalational), type of airway management, preoperative symptoms (fever > 38°C, dyspnoea, pneumonia, running nose, anosmia, hypogeusia, diarrhoea), duration of surgery, anaesthetic respiratory complications (bronchospasm, laryngospasm, intraoperative desaturation below 94%, desaturation below 94% after awakening – observed during first hour after anaesthesia, unplanned postoperative mechanical ventilation), hospital length of stay.
Anaesthetic complications are routinely noted in patients’ anaesthesiology records in a predefined way because in our hospital these data are analysed annually for quality assessment.
The patients’ further medical history was studied as well, searching for any late cardiac, thrombotic, haemorrhagic complications, unplanned ICU admissions or deaths during hospitalisation.
SARS-CoV-2 infection was diagnosed by a polymerase chain reaction (PCR) test obtained from a routinely taken nasopharyngeal swab before surgery/anaesthesia.
Examined group: children diagnosed as SARS-CoV-2 positive, admitted for the purpose of an urgent procedure requiring general anaesthesia within 6 hours of admission.
Control group: SARS-CoV-2 negative children requiring general anaesthesia for the same reasons.
“Children” refers to patients up to 18 years old.
The patients were matched based on the type of the procedure. Based on previously published data we assumed that a control group at least 3 times larger than the examined one would be suitable to prepare a reliable analysis so we decided to analyse records of SARS-CoV-2 negative children consecutively anaesthetised during the first month of observation.
Exclusion criteria were: preoperative ventilation, cyanotic congenital heart disease, newborns, children admitted for procedures that could not be matched between groups.
Intravenous anaesthesia using propofol and fentanyl was used for endoscopy, diagnostic or small surgical procedures (nose setting). All surgical procedures with skin incisions were performed in general anaesthesia with intubation. General anaesthesia with intubation was performed using propofol, fentanyl and rocuronium for induction and sevoflurane and repeated dosages of fentanyl and rocuronium if necessary, for maintenance.
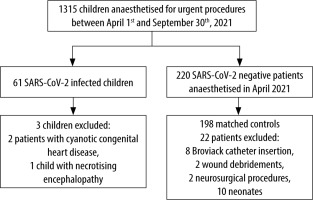
The procedures were performed between April 1st and September 30st, 2021 (Figure 1).
Study endpoints: primary – anaesthetic respiratory complications (bronchospasm, laryngospasm, intraoperative desaturation below 94%, desaturation below 94% after awakening, unplanned postoperative mechanical ventilation); secondary – hospital length of stay, thrombotic, cardiac, haemorrhagic events, admission to the intensive care unit (ICU), deaths during hospitalisation.
Statistical analysis
The quantitative data (age, saturation, etc.) were reported as medians and quartile range.
The Mann-Whitney method was used to compare the medians (age, saturation) between the studied groups, and in the case of dependent data (comparison of saturation after and during the procedure) the Wilcoxon test was used. When comparing the observed cases, the χ2 test was used, and for a low number of observed cases, the same test with Yates’s correction was applied together with the quartile range. Subsequently, logistic regression – uni- and multivariate analysis – was performed.
P-values below < 0.05 were considered statistically significant.
RESULTS
The epidemiological data are presented in Table 1. For the purpose of analysis, we assessed asymptomatic SARS-CoV-2 positive children without other problems as ASA I. The median ASA score was I E for both groups. 31.37% of SARS-CoV-2 positive patients and 17.2% of SARS-CoV-2 negative patients were assessed as ASA III E and IV E.
TABLE 1
Epidemiological data
SARS-CoV-2 infection was confirmed in 61 patients. In 17 patients there was a history of family contact with SARS-CoV-2 infected person. In 42 (71.1%) the PCR test was done only in relation to surgery. Three patients were excluded from the analysis although their anaesthesia was uncomplicated: two patients with cyanotic congenital heart disease and one mechanically ventilated patient with acute haemorrhagic necrotising encephalitis anaesthetised for the purpose of magnetic resonance imaging.
In April 2021, 220 SARS-CoV-2 negative children required emergency procedures in general anaesthesia – 22 children were excluded – 10 neonates with congenital malformations, and 12 children who could not be matched with patients from examined group: 8 children anaesthetised for Broviac catheter insertion, 2 wound debridements and 2 neurosurgical procedures.
In both groups anaesthesia was performed for laparoscopy appendectomies, laparotomies, gastroscopies for foreign body removal, testis torsion surgery, orthopaedic surgery (limb injuries), bronchoscopy for foreign body aspiration, computed tomography, and nose setting.
Preoperative symptoms: 53 (89.83%) SARS-CoV-2 positive patients were asymptomatic.
None complained of anosmia, hypogeusia or diar-rhoea. All the data are shown in Table 2. There was no difference between the rate of assessed symptoms between SARS-CoV-2 positive and negative patients.
TABLE 2
Incidence of infection symptoms
The rate of complications in both groups was very low, with no significant difference between the groups (Table 3).
TABLE 3
Incidence of anaesthetic complication. Numbers refer to complication rate
Complications were observed in 4 children in the SARS-CoV-2 positive (6.90%) and 6 children in the SARS-CoV-2 negative group (3.03%), OR [95% CI] = 2.370 [0.646–8,704], P = 0.1681.
Only one SARS-CoV-2 infected patient – a boy after abdomen injury – required unplanned postoperative mechanical ventilation due to prolonged complicated surgery.
The only differences observed were a higher frequency of desaturations in the awakening period in the SARS-CoV-2 positive patients and longer time of hospitalisation.
Median saturation in both groups was 100%, but IQR was 2.0 in the examined and 1.0 in the control group, P = 0.0112. Median hospital length of stay in control group was 5.5 days [IQR 2–10] and 2 days in the control group [IQR 2–5], P = 0.000028. No thrombotic, haemorrhagic, or cardiac events, unplanned ICU admissions or deaths were observed in any case during hospitalisation.
Factors influencing anaesthetic risk were assessed using logistic regression (Table 4).
TABLE 4
Factors influencing the rate of anaesthetic complications
DISCUSSION
Generally, children account for a minority of SARS-CoV-2 infections and the course of the disease is milder than in adults. Several mechanisms are taken into account as responsible for this phenomenon: compared to adults, children have higher expression of ACE-2 receptors in the type II lung pneumocytes, a higher level of natural killer cells (NK cells), a heightened interferon response and T cell immunity [17]. Additionally, their contribution to the spread of the epidemic has not been clearly evaluated. At the same time there is no cross- sectional testing in the population so the data may be underestimated. Against this background data obtained from preoperative testing have additional value [10]. The interesting point of our study is that probably the percentage of symptomless children is much higher than evaluated: 71.1% of our SARS-CoV-2 positive patients had neither symptoms nor history of contact with an infected person. In addition, 3 patients complaining of fever had no respiratory symptoms and were diagnosed with appendicitis, so perhaps they also should be counted as SARS-symptomless cases. If it were not for preoperative testing they probably would not be diagnosed. At the same time, they could be a potential source of infection in the population.
The risk of anaesthetic respiratory complications in infected children is still a matter of concern. In our examined group the incidence of complications was very low. Only 1 patient had laryngospasm (the boy with COVID-19 pneumonia) and 3 patients had incidents of desaturation below 94% after awakening. The only patient requiring postoperative mechanical ventilation was a 14-year-old boy after car injury and abdominal trauma without respiratory problems. In comparison, Saynhalath et al. [16] reported 13.7% risk of anaesthetic complications in infected patients: 7.9% respiratory, 2% cardiovascular adverse events and 3.9% both. The probability of respiratory complications observed in this study did not differ from what had previously been reported in other respiratory infections [18]. Interestingly, in the mentioned report complications also occurred in the symptomless patients. Probably it was connected not only with the infection itself – in this study 49% of patients were assessed as ASA III and IV. In another study concerning anaesthesia in SARS-CoV-2 positive children the authors reported 26% risk of anaesthetic complications with no difference between patients with or without respiratory symptoms. In this study 60% of infected patients were assessed as ASA III and IV, compared to only 31.7% in our examined group [15]. The results of multivariate logistic regression conducted by us prove that the risk of complications is connected with patient physical status and duration of the procedure, which is obvious for anaesthesia risk in children [19, 20]. Our observations are consistent with other published observations of local experience [14, 21]. It is worth noting that risk of anaesthesia in children is connected with anaesthesiologist’s experience [19]. As our hospital is a Teaching University Hospital, in our institution the children are always anaesthetised by or under the close supervision of an experienced specialist.
Interestingly, the main complication in our study was hypoxaemia after awakening. Fortunately, it did not lead to serious sequelae. A recently published study showed that children infected with SARS-CoV-2 are predisposed to desaturation during airway management even if the patient was symptomless; the authors however did not examine saturations in the post-anaesthesia period [22].
Of course, the limitation of our study was the size of the study group, but at the same time authors who reported greater numbers of patients had to organise multi-centre studies; e.g. Reiter et al. [14] reported 266 procedures requiring anaesthesia in SARS-CoV-2 infected children in 20 (!) American hospitals performed from March to October 2020. Our report confirms that locally SARS-CoV-2 infection in children imposes neither an excessive burden on the healthcare system nor a special risk for patients – especially asymptomatic – so perhaps the suggestion that there is no need for a delay in surgery should be seriously considered [21, 23].
The small number of patients was the reason why we did not assess the influence of drugs chosen for anaesthesia. We made the distinction only between anaesthesia with and without endotracheal intubation.
Another limitation is the short time of observation: we collected the data only during hospitalisation, with a median time of 5 days, whereas serious events occurring up to 30 days after surgery/anaesthesia have been reported [13].
CONCLUSIONS
In our experience, anaesthesia of SARS-CoV-2 infected children can be safely performed. Comparison of our results with published data suggests that the duration of the procedure and accompanying factors are the main factors influencing the risk of anaesthesia. Infected patients whose physical status is assessed as ASA III and more are at higher risk of complications. Desaturation in the early postoperative period was the main complication observed. It is a clear indication that saturation should be closely monitored after general anaesthesia in SARS-CoV-2 infected children.
In addition, the results of preoperative testing in symptomless patients suggest that the exact number of infected children in the population is probably greater than assessed. The group size and time of observation are the main limitations of our study.