Summary
In the present study, for the first time in the literature, we demonstrated that prestroke CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes mellitus, stroke, vascular disease and sex) score was significantly and independently associated with success of recanalization as assessed with Modified Thrombolysis in Cerebral Infarction (mTICI) score in a cohort of acute ischemic stroke patients regardless of atrial fibrillation presence who underwent endovascular treatment. Additionally, a CHA2DS2-VASc score of more than 3.5 was associated with unsuccessful reperfusion as assessed by ROC curve.
Introduction
Cerebrovascular events are one of the leading causes of morbidity and mortality worldwide. There are two types of cerebrovascular accident and ischemic stroke is the most common type [1, 2]. The vast majority of ischemic stroke events occur due to thrombosis and/or embolism in the atherosclerotic background [3]. While only symptomatic treatment, secondary prevention and rehabilitation were possible in the treatment of acute ischemic stroke for a long time, the FDA approved recombinant tissue plasminogen activator (rt-PA) treatment in 1996. More recently, endovascular treatment methods emerged not only as an alternative treatment modality but also as a better option for eligible patients with ischemic stroke [4].
Although endovascular treatment is an effective treatment especially in the first 6 h after the onset of symptoms, it has also been proven to be effective between 6 and 24 h as a treatment method that has also been recommended by the guidelines for appropriate patients [5–7]. However, 20% of acute stroke patients undergoing endovascular treatment have suboptimal or failed reperfusion. Risk factors for unsuccessful reperfusion include but are not limited to anatomy of the occluded vessel, time from symptom onset to the procedure and etiology of stroke [8].
CHA2DS2-VASC score (heart failure, hypertension, age, diabetes mellitus, stroke, vascular disease, and female gender) is a simple risk stratification algorithm used to predict thromboembolic risk in patients with atrial fibrillation (AF) and to guide anticoagulant therapy. People with a high score have a high thromboembolic risk and these patients should receive lifelong anticoagulant therapy unless contraindicated [9]. However, there are no clear and conclusive data regarding the relationship between response to endovascular or thrombolytic therapy in ischemic stroke and CHA2DS2-VASc score.
Aim
In the present study, we therefore investigated whether pre-stroke CHA2DS2-VASc score is associated with success of endovascular therapy in patients with acute ischemic stroke with and without AF undergoing percutaneous thrombectomy.
Material and methods
We conducted a retrospective analysis based on data collected from 159 consecutive acute ischemic stroke patients with or without AF, who were admitted to the Bezmialem Vakıf University Hospital and Memorial Hospital between September 2013 and December 2018 and underwent endovascular treatment within the first 6 h after symptom onset.
The inclusion criteria were as follows: patients older than 18 years, anterior or posterior circulation large vessel occlusion without intracranial hemorrhage confirmed by computed tomographic angiography (CTA) or magnetic resonance angiography (MRA) within 6 h from symptom onset, pre-stroke modified Rankin Scale (mRS) < 2, a National Institutes of Health Stroke Scale (NIHSS) score ≥ 6 at admission and an Alberta Stroke Program Early Computed Tomography Score (ASPECTS) ≥ 6 based on non-contrast brain computed tomography (CT) or diffusion-weighted magnetic resonance imaging (MRI). Comorbidities, vital conditions and CHA2DS2-VASc scores of all patients were recorded. Cerebral angiography was performed with a Phillips Allura Xper (Amsterdam, Netherlands) device and mechanical thrombectomy and thrombus aspiration were the methods used as endovascular treatment. Modified Thrombolysis in Cerebral Infarction (mTICI) flow scores of all patients were recorded after endovascular treatment
Patients with insufficient laboratory or clinical data, carotid artery dissections and spontaneous revascularization after intravenous tissue plasminogen activator (tPA) were excluded. Additionally, patients were excluded from the study if they were pregnant, were receiving any immunomodulatory drugs, if they had concurrent or recent infections, recent myocardial infarction (< 1 month before the study), patients with known collagen tissue diseases, patients with a history of gastrointestinal bleeding or major trauma within the last 1 week, hematological malignancy, severe hepatic or renal disease, or if no clinical outcome follow-up was available at 3 months.
All patients underwent mechanical thrombectomy with a stent-like retriever (Solitare [Covidien, Irvine, CA, USA] or Trevo [Stryker, Fremont, CA, USA]). Rescue therapies (balloon angioplasty, stent implantation, intra-arterial thrombolysis, or intracatheter tirofiban administration, etc.) were performed when the target artery recanalization failed with a stent-like retriever. In addition, on a smaller number of patients who were considered to have atherosclerotic occlusion, balloon angioplasty was performed with or without stent implantation directly.
Brain CT scan was performed in order to rule out hemorrhagic stroke on admission. MRI with diffusion weighted imaging was performed for the assessment of occluded vessels. After the interventional procedure, a brain CT scan was performed routinely in order to rule out intracerebral hemorrhage (ICH). Endovascular thrombectomies were performed under conscious sedation or general anesthesia (determined by the interventionist and anesthesiologist in consensus depending on the clinical situation of the patient).
For evaluation of the degree of leptomeningeal collaterals, occlusion status of the occluded vessel was confirmed by performing angiography after locating the guiding catheter to the left internal carotid artery. A first-line aspiration with a large-bore aspiration catheter or a stent retriever with manual aspiration during stent retrieval was performed by a triaxial system. The choice of thrombectomy technique varied depending on the operator’s preference. In the event of a partial or no response, the operator decided to switch to another technique or repeat the initial maneuver. The goal was to finish the procedure when successful reperfusion was observed. Successful reperfusion was defined as mTICI 2 c or mTICI 3 flow on the latest angiography. The patients were divided into two groups according the mTICI grade after endovascular therapy. Patients with mTICI grade 2c or 3 were defined as group 1, and those with mTICI grade 0, 1, 2a or 2b were group 2. The mTICI flow grade of the study population was evaluated by a cardiologist and an interventional neurologist.
Hypertension was defined as systolic blood pressure ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg, previously diagnosed hypertension or use of any antihypertensive medications. Hyperlipidemia was defined as serum total cholesterol ≥ 240 mg/dl, serum triglyceride ≥ 200 mg/dl, low-density lipoprotein cholesterol ≥ 130 mg/dl, previously diagnosed hyperlipidemia or use of lipid-lowering medication. Diabetes mellitus was defined as fasting plasma glucose levels more than 126 mg/dl in multiple measurements, previously diagnosed diabetes mellitus or use of antidiabetic medications such as oral anti-diabetic agents and/or insulin. Smoking status was defined as a history of tobacco use at admission or in the 6 months prior to the visit. Coronary artery disease was defined as a history of stenosis of ≥ 50% in any coronary artery or coronary revascularization. Heart failure was defined as an ejection fraction of ≤ 40% or a history of hospitalization for heart failure. The diagnosis of AF was based on a 12-lead electrocardiogram and 24-hour Holter monitoring or a history of paroxysmal AF. The CHA2DS2-VASc score was calculated for each patient by assigning 1 point each for the following factors: age between 65 and 74 years, hypertension, diabetes mellitus, and heart failure, and 2 points for age ≥ 75 years and a previous stroke or transient ischemic attack. The study was approved by the local Ethics Committee.
Statistical analysis
Continuous data were expressed as mean ± standard deviation or median, while categorical data were presented as number or percentage of patients. Depending on the normality of distribution as assessed by the Kolmogorov-Smirnov test, continuous variables were compared using the Student t-test or the Mann-Whitney U test. Categorical variables were compared using Fisher’s exact test or the χ2 test. Correlation analysis was done with the Pearson or Spearman test where applicable. Multivariate logistic regression analysis (backward) was performed to determine the independent predictors of successful reperfusion. Parameters that were significant in univariate analysis were included in the multivariate logistic regression analysis. Odd ratios (ORs) and 95% confidence intervals (CIs) were calculated. Receiver operating characteristic (ROC) curve analysis was performed to determine the cut-off value of CHA2DS2-VASc score for predicting successful reperfusion. All tests used a 2-tailed p-value of 0.05 as a threshold for significance. All analyses were carried out with SPSS version 16.0 software for Windows (SPSS Inc., Chicago, Illinois, USA).
Results
71 (44.7%) of the patients included in the study were female and the mean age of the patients was calculated as 65.7 ±12.9. Considering the comorbidities of the patients, 63 (39.6%) patients had AF, 80 (50.3%) patients had hypertension, and 17 (10.7%) patients had a history of stroke or transient ischemic attack. Demographic characteristics of the patients are presented in Table I. The mean CHA2DS2-VASc score of the patients in the study was found to be 3.2. The median NIHSS score, which indicates the severity of ischemic stroke, was 18. Considering the occlusion localizations in the large vessels in CT angiography/MR angiography performed on the patients, internal carotid artery (ICA) occlusion was found in 42 (26.4%) patients and occlusion of the middle cerebral artery (MCA)’s M1 and M2 branches was observed in 104 (65.4%) patients. Before endovascular treatment, IV tPA was given to 35 (22%) patients. Of 159 patients, 34 were treated with a stent retriever only, 5 were treated with thrombo-aspiration only, and 120 were treated with both methods.
Table I
Demographic characteristics of the study population
Successful reperfusion was observed in 130 (81.8%) of all patients who underwent endovascular treatment (mTICI flow ≥ 2c) and first-pass reperfusion was observed in 107 (67.3%) patients. When the patients with successful (mTICI flow ≥ 2c) and unsuccessful (mTICI flow ≤ 2b) reperfusion were divided into groups, no significant difference was observed between the patients in terms of comorbidities such as AF, hypertension, hyperlipidemia, coronary artery disease and cerebrovascular accident history. Patients with unsuccessful reperfusion were older than patients with successful reperfusion (71.4 ±11.2 v. 64.5 ±13.01, p = 0.006), with a higher CHA2DS2-VASc score (4.1 ±1.5 vs. 3.04 ±1.6, p = 0.002). In addition, the duration of the procedure was longer in the unsuccessful reperfusion group (92.4 ±27.2 min vs. 65.0 ±25.1 min, p < 0.001). CHA2DS2-VASc score significantly correlated with successful recanalization (correlation coefficient; 0.243, p = 0.002). Additionally, the number of attempts was higher (2.5 ±1.9 vs. 1.9 ±0.9, p = 0.003) in the group with a higher CHA2DS2-VASc score. Comparison between successful and unsuccessful reperfusion groups is presented in Table II.
Table II
Comparison of clinical and procedural parameters in groups with and without successful reperfusion
Multivariate logistic regression analysis revealed that only CHA2DS2-VASc score (OR = 1.43, 95% CI: 1.09–1.87, p = 0.006) and procedure time (OR = 1.03, 95% CI: 1.01–1.05, p < 0.001) were independent predictors of successful reperfusion. The results of the multivariate logistic regression analysis are presented in Table III.
Table III
Multivariate logistic regression to predict successful reperfusion
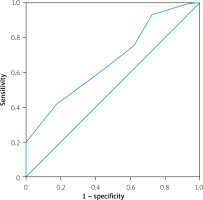
The ROC curve was used to determine the cut-off value for the CHA2DS2-VASc score that best predicts successful reperfusion. The optimal threshold was 3.5, with a sensitivity of 58.6% and specificity of 59.2% (area under the curve (AUC) = 0.669, p = 0.005). The ROC curve for CHA2DS2-VASc is presented in Figure 1. After a follow-up of 90 days, a favorable outcome (mRS ≤ 2) was observed in 71 (44.7%) of the patients evaluated via mRS, whereas 24 patients died (mRS: 6).
Discussion
In the present study, for the first time in the literature, we demonstrated that pre-stroke CHA2DS2-VASc score was significantly and independently associated with success of recanalization as assessed with mTICI score in a cohort of acute ischemic stroke patients regardless of AF presence who underwent endovascular treatment. Additionally, a CHA2DS2-VASc score of more than 3.5 was associated with unsuccessful reperfusion as assessed by ROC curve.
Although endovascular treatment is an effective treatment especially in the first 6 h after the onset of symptoms, it has also been proven to be effective between 6 and 24 h as a treatment method that has also been recommended by the guidelines for appropriate patients [5–7]. However, 20% of acute stroke patients undergoing endovascular treatment have suboptimal or failed reperfusion. Risk factors for unsuccessful reperfusion include but are not limited to anatomy of the occluded vessel, time from symptom onset to the procedure, and etiology of stroke [8].
The CHA2DS2-VASc score is a widely used scoring system for regulation of anticoagulant therapy in patients with AF. Many studies have shown that this scoring system also affects prognosis in some diseases other than AF [10–13]. In a study of AF-related cardioembolic stroke patients, Nezu et al. found a positive correlation between the CHA2DS2-VASc score and the NIHSS score, which indicates the severity of stroke [12]. In another study conducted in patients with acute ischemic stroke, Topaz et al. found that each 1-point increase in the pre-stroke CHA2DS2-VASc score increased the risk of serious disability by 21% [13]. In another study conducted in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease, Huang et al. investigated the relationship between CHA2DS2-VASc score and slow flow/no-reflow. As a result of this study, the presence of slow flow/no-reflow in patients with a CHA2DS2-VASc score of 3 was found 1.7 times more often than in patients with a score of < 3 [11]. However, so far there are no clear and conclusive data regarding the relationship between response to endovascular or thrombolytic therapy in ischemic stroke and CHA2DS2-VASc score [14–16]. In the present study, we therefore investigated whether pre-stroke CHA2DS2-VASc score is associated with success of endovascular therapy in patients with acute ischemic stroke with and without AF undergoing percutaneous thrombectomy.
It is known that each component of the CHA2DS2-VASc score can cause thrombotic events, and various studies have been carried out to evaluate the results of this score after percutaneous interventions, especially in acute coronary syndromes. As a result of these studies, the relationship between slow flow/no-reflow phenomenon and high CHA2DS2-VASc score after percutaneous intervention in patients with acute coronary syndrome with or without ST elevation has been demonstrated [10, 11]. However, there is only one study in the literature investigating the relationship between the results obtained after endovascular intervention and the CHA2DS2-VASc score in patients with acute ischemic stroke.
In a recent study, Yaşar et al. investigated the relationship between postprocedural mTICI flow and CHA2DS2-VASc score in 102 patients undergoing endovascular treatment for acute ischemic stroke. As a result of this study, the CHA2DS2-VASc score was found to be significantly higher in the patient group with mTICI flow < 2c (2.78 ±1.44, 5.02 ±1.77, p < 0.001). In addition, a CHA2DS2-VASc score ≥ 3 was determined as a predictor of a failed attempt (area under the curve (AUC) = 0.827, 95% CI: 0.739–0.895, p < 0.001) [17]. Similarly, in our study, the CHA2DS2-VASc score of the patients with a flow < mTICI 2c after thrombectomy was found to be significantly higher than in the patients with a flow of mTICI 2c and 3 (4.1 ±1.5 vs. 3.04 ±1.6, p = 0.002).
Although our study design is similar to the one published by Yasar et al., our study population is bigger. Additionally and more importantly, in our study CHA2DS2-VASc score but not presence of AF was associated with procedural success. In the study reported by Yasar et al., AF and the CHA2DS2-VASc score were independent predictors of successful reperfusion, whereas in our study AF was not associated with reperfusion success. Our findings are concordant with the study published by Ntaios et al., which reported that pre-stroke CHA2DS2-VASc score predicted long-term stroke outcomes (mortality, stroke recurrence and cardiovascular events) in non-AF patients with acute ischemic stroke [18].
It is known that the components of hypertension, older age, heart failure, diabetes and vascular disease history in the CHA2DS2-VASc score contribute to the development of thrombus and therefore cause undesirable events [19–23]. Arterial hypertension causes direct damage to the vascular endothelium due to increased shear stress and thus causes remodeling in endothelial cells. After these changes observed in endothelial cells, a decrease in nitric oxide (NO) bioavailability and synthesis, deterioration of anti-oxidant mechanisms, and inhibition of endothelin mechanisms that prevent cell adhesion are observed. Inhibition of endothelial vasodilation due to a decrease in NO secretion causes the release of pro-inflammatory and pro-coagulant substances. When all the effects of these factors come together, vasoconstriction, platelet aggregation and adhesion are observed. As a result, thrombus development is inevitable [19]. In addition, in a study conducted in hypertensive patients, thrombin production in hypertensive patients was found to be significantly higher than that in the healthy control group [20]. In a study conducted in patients with acute ischemic stroke, hypertension was demonstrated to be one of the predictors of unsuccessful recanalization after thrombectomy in the anterior circulation [21].
Although in our study, when patients with successful and unsuccessful perfusion were compared separately in terms of CHA2DS2-VASc components, no significant difference was observed. The combinational/cumulative effect of high CHA2DS2-VASc scores might have affected the post-procedural reperfusion.
Vascular complications are frequently seen in patients with diabetes mellitus. These complications can be clinically reflected in the form of involvement of large vessels (diabetic macroangiopathy) or small vessels (diabetic microangiopathy). It has been shown that hyperglycemia seen in diabetic patients causes damage by causing a decrease in the amount of NAD+ in endothelial cells and an increase in superoxide production, causing low-density lipoprotein (LDL) oxidation. As a result of this damage, endothelial dysfunction develops and pro-coagulant molecules are released, resulting in a state of hypercoagulability [22]. In the presence of heart failure, various causes, especially low cardiac output, are added to causes such as increased inflammation, high prothrombotic substances, and endothelial dysfunction; it gives us an idea why the thrombotic complication rate is high in heart failure patients even if they are in sinus rhythm [23].
Among the possible reasons for endovascular treatment failure are a large thrombus load and the thrombus type. A study by Rai et al. showed that internal carotid artery occlusion may be one of the predictors of unsuccessful recanalization in patients undergoing endovascular treatment for acute ischemic stroke and the reason for this is high thrombus load [24]. In addition, in acute ischemic stroke patients with non-valvular AF, Deguchi et al. found in a study that the incidence of internal carotid artery occlusion increased as both the CHADS2 and CHA2DS2-VASc scores increased [25]. The presence of atherosclerotic plaque may be another reason for failure of endovascular therapy. This situation is more common especially in patients with typical cardiovascular risk factors such as hypertension and diabetes mellitus [26]. Since hypertension and diabetes mellitus are components of the CHA2DS2-VASc score, they might have affected the outcome of our study.
Although the relatively small number of patients, retrospective design and single-team experience might be considered among the study limitations, our results provide novel and practical findings which have clinical implications. In conclusion, we observed that pre-stroke CHA2DS2-VASc score was significantly and independently associated with success of recanalization as assessed with mTICI score in a cohort of acute ischemic stroke patients regardless of AF presence who underwent endovascular treatment, which deserves to be verified with large scale prospective trials.