Cardiac tamponade is a life-threatening condition in which the accumulation of fluid or blood within the pericardial sac leads to elevated intrapericardial pressure, impaired diastolic filling of the cardiac chambers, and reduced cardiac output, ultimately resulting in circulatory failure and organ ischemia [1]. The most common causes of acute tamponade include blunt or penetrating chest trauma, myocardial free wall rupture following acute myocardial infarction, aortic dissection, and complications after cardiac surgery or interventional cardiology procedures [2]. Chronic causes include malignant disease, pericarditis of infectious or autoimmune etiology, and complications of uremia [1]. Diagnosis is based on clinical presentation and imaging studies, with transthoracic or transesophageal echocardiography playing a central role in assessing effusion size, identifying hemodynamic signs of chamber compression, and guiding interventional procedures [3]. The goal of treatment is rapid relief of pericardial pressure and restoration of hemodynamic stability, which, depending on the clinical scenario, may involve echocardiography-guided pericardiocentesis, surgical drainage via subxiphoid approach or thoracotomy/sternotomy, and, in recurrent or loculated effusions, the creation of a pericardial window [4].
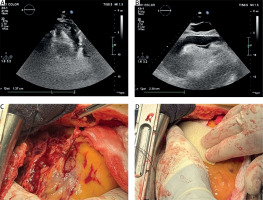
A 78-year-old male patient with chronic heart failure, hypertension, permanent atrial fibrillation (AF), previous stroke, history of gastrointestinal bleeding and prior percutaneous coronary intervention (PTCA) with stent implantation was admitted with blunt thoracic trauma the day after a bicycle accident. Due to the presence of coronary stents and permanent AF, the patient was maintained on combined antiplatelet and anticoagulant therapy. Upon admission, the patient was unconscious and mechanically ventilated, exhibited hemodynamic instability, and was on high doses of inotropic drugs. Trauma computed tomography revealed heterogeneously dense pericardial fluid, intracerebral and subdural hemorrhages, which did not require neurosurgical intervention, facial fractures, suspected cervical spine injury, and free fluid within the abdominal cavity. Transthoracic echocardiography identified systolic collapse of the free wall of the right ventricle, with a pericardial effusion measuring 24 mm anterior to the RV with an organized clot measuring 15 mm (Figures 1 A, B). In light of the patient’s numerous clinical comorbidities and the concomitant administration of antiplatelet and anticoagulant therapies, it was deemed necessary to proceed with a minimally invasive pericardiocentesis performed via a pigtail catheter under echocardiographic guidance. Attempted percutaneous drainage resulted in iatrogenic puncture of the right ventricular free wall, prompting urgent conversion to sternotomy. During the procedure, it was confirmed that the pigtail catheter was placed in the right ventricle. The catheter was carefully withdrawn, and the insertion site in the diaphragmatic surface of the right ventricle was secured with 4.0-sutures and Teflon patches. Intraoperatively, an epicardial flap tear (2 × 3 cm) of the anterior wall of the right ventricle was identified. In addition, multiple epicardial-pericardial adhesions divided the pericardial sac into compartments with varying amounts of clots (Figure 1 C). Hemostasis was successfully achieved with application of a TachoSil patch (Baxter) (Figure 1 D). Due to thrombocytopenia (platelet count of 72,000/μl), elevated INR level (1.7) and antiplatelet and anticoagulant therapy, delayed chest closure was performed. The chest was finally closed the next day. Postoperatively, the patient required mechanical ventilation, high-dose vasoactive support, dialysis, and anticonvulsant medication. Despite maximal intensive care treatment, the patient progressed to refractory multiorgan failure. Unfortunately, on the sixth day after the operation the patient died. Blunt cardiac trauma (BCT) is an uncommon but potentially fatal consequence of chest injury, with reported incidence less than 10% in all trauma admissions although it is responsible for approximately 25% of traumatic deaths [5]. Among its severe complications, cardiac tamponade though rare requires urgent identification and management. In this case, a 78-year-old man with multiple comorbidities sustained blunt thoracic trauma complicated by pericardial tamponade. Pre-existing pericardial adhesions likely resulting from prior cardiac history facilitated tamponade development. The patient’s chronic anticoagulant and antiplatelet therapy for AF and coronary artery disease impaired physiological hemostasis, contributing to ongoing hemorrhage and complicating conservative management of the pericardial effusion. This illustrates the difficult balance between bleeding risk and thromboembolic protection in cardiovascular patients [6]. Transthoracic echocardiography revealed localized tamponade with systolic collapse of the right ventricular free wall, a dynamic finding linked to uneven pericardial pressure from organized clot and adhesions. Faced with acute hemodynamic instability and high hemorrhagic risk, an echocardiography-guided pericardiocentesis was performed. Although image-guided pericardiocentesis is considered safe in trauma settings, in this patient it led to iatrogenic ventricular laceration, necessitating urgent conversion to open sternotomy for definitive repair. This case underscores several key clinical insights. First, cardiac tamponade is a life-threatening condition that requires immediate intervention, and neither comorbidity nor coagulopathy should be viewed as a complete contraindication to lifesaving procedures. Second, even echocardiography-guided pericardiocentesis may be unsafe or ineffective when loculated effusions, adhesions, or organized clots are present. Lastly, structural vulnerability such as surgical adhesions combined with pharmacological anticoagulation can convert seemingly minor blunt trauma into a catastrophic event, highlighting the importance of tailored procedural planning and preparedness to escalate to surgical intervention.