Percutaneous coronary interventions are among the most frequently performed cardiological procedures both in Poland and worldwide. Like all invasive procedures, they carry a risk of complications. Among the relatively rare but life-threatening events are coronary vessel perforations. These complications predominantly occur during coronary angioplasty, while perforations during coronary angiography are significantly less common. We present a case of a coronary angiography complication involving the rupture of a small intermediate branch of the left coronary artery caused by the pressure of injected contrast medium [1–3].
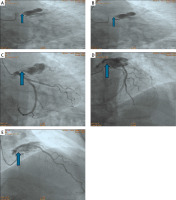
A 69-year-old patient with a history of previous coronary interventions was admitted to the Cardiology Department due to symptoms of class II angina (CCS II) for elective coronary angiography. After appropriate preparation, angiography of the right coronary artery was performed using a diagnostic catheter (JR 4.0, 6F), which revealed no significant angiographic lesions. Subsequently, the diagnostic catheter was replaced with a left coronary catheter (JL 4.0, 6F), and following vessel intubation, contrast injection revealed contrast extravasation in the course of a small intermediate branch at the site of catheter positioning (Figure 1).
Figure 1
Angiography of the left coronary artery in various projections showing perforation of a small vessel. A – LAO 2.3°; Caudal 17.7°; time: 8:07 PM, B – LAO 2.3°; Caudal 17.7°; time: 8:07 PM, C – LAO 2.3°; Caudal 17.7°; time: 8:07 PM, D – LAO 14.4°; Cranial 19.2°; time: 8:08 PM, E – RAO 25.2°; Cranial 26.4°; time: 8:09 PM
An urgent echocardiographic examination was performed, excluding the presence of pericardial effusion. The patient remained hemodynamically stable and asymptomatic, with no recorded cardiac arrhythmias. After correcting the diagnostic catheter’s position, the procedure was completed, revealing no significant angiographic lesions in the coronary arteries. The patient was subsequently managed conservatively. During further observation, serial echocardiographic evaluations showed no significant abnormalities. The diagnosis of vessel perforation with blood extravasation into the myocardial tissue was established. Following a period of observation, the patient was discharged in good general condition with recommendations for continued outpatient follow-up.
Coronary vessel perforations are relatively rare but potentially severe complications. Cases caused by vessel rupture due to the pressure of injected contrast are almost anecdotal. Other potential causes of contrast extravasation include pre-existing vessel fragility due to atherosclerosis, microvascular disease, or previous interventions that may weaken the arterial wall. Additionally, excessive injection pressure, inadvertent catheter-induced trauma, or anatomical variations in coronary artery structure can contribute to vessel rupture. In this case, a detailed analysis of the patient’s previous angiogram allowed for the identification of the perforated vessel and the establishment of the final diagnosis. A similar complication can also occur during RCA cannulation when the catheter enters a small branch of the cone, and the contrast is injected too aggressively. The present case shows that early recognition and immediate echocardiographic assessment allowed for the exclusion of more serious complications, such as cardiac tamponade, facilitating the safe completion of the procedure. Enhancing coronary angiography techniques, including ensuring proper catheter positioning, plays a crucial role in minimizing the risk of complications such as vessel perforations. The patient’s favorable outcome underscores the importance of appropriate in-hospital monitoring and subsequent outpatient follow-up to evaluate the long-term consequences of such events [4, 5].








