Introduction
Ovarian masses in postmenopausal women are a frequent clinical finding and pose a significant diagnostic challenge, especially when they exhibit complex imaging features. Differentiating between benign and malignant lesions is crucial for planning appropriate surgical management while avoiding overtreatment. The integration of multimodal imaging – including transvaginal ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) – alongside serum biomarkers and validated risk models such as the International Ovarian Tumor Analysis (IOTA) ADNEX model, has improved diagnostic accuracy in this setting.
Ovarian lesions that present with solid components, papillary projections, and ascites raise a high index of suspicion for malignancy, particularly in postmenopausal patients. The IOTA ADNEX model allows clinicians to estimate the risk of malignancy by integrating clinical, biochemical, and ultrasound findings. However, even with advanced tools, diagnostic pitfalls remain possible, especially in cases of benign lesions with atypical imaging features.
We present the case of a 49-year-old postmenopausal woman with acute abdominal pain and a complex left adnexal mass identified on ultrasound, CT, and MRI [1–3].
Case presentation
A 49-year-old nulliparous woman presented to the Emergency Department with severe abdominal pain. Her medical history was unremarkable. She reported menarche at 13 years of age, regular menstrual cycles until menopause, which had occurred approximately one year prior. She had received combined estrogen-progestin hormone replacement therapy for 6 years. No family history of gynecologic cancer.
Transvaginal ultrasound revealed a unilocular-solid left adnexal mass with a maximum diameter of 13 cm, composed of a cystic portion measuring up to 8 cm and a solid internal component of 5 cm, three papillary projections exhibiting central vascularization on color Doppler. Ascites (pelvic fluid collection) was present. No posterior acoustic shadowing was observed (Fig. 1).
Fig. 1
Transvaginal ultrasound: unilocular-solid mass measuring13 cm with a 5 cm solid component and vascularize papillae

Abdominal ultrasound confirmed the presence of a left adnexal fluid-solid lesion and peritoneal fluid. A subsequent non-contrast-enhanced CT scan of the upper and lower abdomen showed a left adnexal fluid-solid lesion approximately 13 cm in size, with a prominent solid component and peritoneal effusion in the perihepatic, perisplenic, and interloop regions, consistent with ascites. No iliac or obturator lymphadenopathy or signs of peritoneal carcinomatosis were observed.
Pelvic MRI (with and without contrast) confirmed a unilocular-solid mass with a projecting solid component (dimensions 42 × 22 × 24 mm), moderate post-contrast enhancement, pelvic ascites, and an enlarged uterus with fibroids. No adjacent organ infiltration (Fig. 2).
Fig. 2
Pelvic MRI: unilocular adnexal mass with an internal solid component and moderate post-contrast enhancement
CA 125 was 35.4 U/ml; HE4 was not available. The IOTA ADNEX model, calculated using clinical and ultrasound data through freely accessible online tools (not integrated in the ultrasound equipment used), estimated an overall malignancy risk of 81.2%.
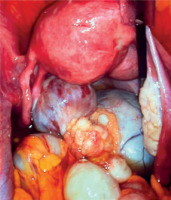
Given the patient’s severe pain, evident clinical distress, and the oncologic suspicion, the entire preoperative workup was conducted in an emergency setting, and an urgent exploratory laparoscopy was performed. Intraoperatively, the left ovary appeared enlarged with a cystic formation approximately 13 cm in size and two external surface vegetations clearly visible on the ovarian wall. The mass appeared partially twisted on its axis, contributing to the suspicious intraoperative appearance. No signs of carcinomatosis or lymphadenopathy were observed. A left salpingo-oophorectomy was performed with retrieval in an endobag. Simultaneously, peritoneal and cystic fluid samples were taken and sent for cytological examination (Fig. 3).
Fig. 3
Intraoperative appearance of the left adnexal mass: large, partially twisted lesion with smooth surface, without evidence of carcinomatosis

Final histological examination revealed a benign serous cystadenofibroma. The papillary component consisted of serous epithelial proliferations without atypia. Cytological analysis of the peritoneal and cystic fluids was negative for atypical cells.
Postoperative recovery was regular and the patient was discharged on the second day.
Discussion
As evaluated clinically by the attending gynecologic team, this case illustrates a situation in which, despite highly suspicious imaging features (vascularized papillae, ascites, postmenopausal status, mass > 10 cm), the histological findings confirmed a complex benign lesion. Although the IOTA ADNEX model is validated and useful in clinical practice, it may overestimate malignancy risk in the presence of lesions such as cystadenofibromas, which can mimic borderline or malignant neoplasms on imaging.
Although not applicable to this benign case, there is growing interest in the use of liver-directed interventional oncology techniques such as transarterial chemoembolization (TACE), radioembolization, and thermal ablation for the management of unresectable hepatic metastases from ovarian cancer. These locoregional strategies may represent future therapeutic avenues in selected oncologic scenarios with limited metastatic burden [4].
Recent literature has also highlighted the role of biomolecular markers and gene expression profiling in refining the differential diagnosis of adnexal masses. These tools, while not directly applied in the present case, may support risk stratification in ambiguous or recurrent lesions [5].
In addition, although the final histopathological diagnosis in this case was benign, it is important to consider the broader differential diagnosis including borderline ovarian tumors. According to Pecorino et al. [6], the recurrence rate of borderline tumors has been reported at approximately 3.5%, particularly in cases managed conservatively. This underlines the importance of long-term follow-up even in lesions initially considered benign but with complex imaging features.
While the IOTA ADNEX model estimated a high risk of malignancy (81.2%), it is worth considering whether this value might have been influenced by the patient’s acute clinical presentation. Acute abdominal conditions, such as adnexal torsion or peritoneal irritation, may alter sonographic features, particularly vascularity and complexity, thereby potentially affecting the accuracy of predictive scoring systems. Existing literature suggests that risk models, though validated in elective settings, may yield false-positive estimates when applied during emergency presentations [7].
Correlation between imaging, biomarkers, intraoperative evaluation, and histology remains essential for appropriate management. The laparoscopic approach enabled both diagnosis and treatment in a minimally invasive fashion, even in a high-risk clinical context [8, 9].
Conclusions
Despite an IOTA ADNEX risk of 81.2%, the final histological diagnosis confirmed the benign nature of the lesion. This case highlights the importance of multidisciplinary integration in the evaluation of suspicious ovarian masses that sometime is not enough to avoid overtreatment in patients with benign but complex-appearing lesions.










